Sporotrichosis of Maxillary Sinuses in a Middle Aged Female Patient from Rural Area of Eastern India
Anita Nandi (Mitra)1, Saumik Das2, Ramanuj Sinha3, Neeraj Aggarwal4, Sriparna Chakravorty5
1 Assistant Professor, Department of Microbiology, Medical College, Kolkata, India.
2 Associate Professor, Department of ENT, Medical College, Kolkata, India.
3 Professor and Head, Department of ENT, Medical College, Kolkata, India.
4 Postgraduate Trainee, Department of ENT, Medical College, Kolkata, India.
5 Postgraduate Trainee, Department of Microbiology, Medical College, Kolkata, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anita Nandi (Mitra), BD 173, Salt Lake, Kolkata-700064, India.
E-mail: Anitanandi20121964@gmail
Sporotrichosis is commonly a chronic infection caused by Sporothrix schenckii, a saprophytic fungus and is usually limited to cutaneous and subcutaneous tissues. Disseminated systemic, osteoarticular or pulmonary sporotrichosis have been reported but nasal sinusitis by this fungus is extremely infrequent. Earlier report from southern India documented a case of maxillary sinusitis by Sporothrix schenckii. Here we report a similar case of bilateral maxillary sinusitis in a middle aged female from a village of Bihar, a state in eastern India. She underwent endoscopic maxillary sinus surgery for nasal symptoms and diagnosed to have sporotrichotic infection of maxillary sinuses. The diagnosis was done by mycological and histopathological examination and patient improved under antifungal chemotherapy.
Maxillary sinusitis, Mucopurulent discharge, Sporothrix schenckii
Case Report
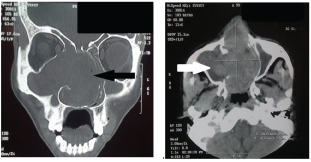
A 45-year-old female patient attended the outpatient ENT clinic of our tertiary care hospital with chief complaints of nasal stuffiness and frequent blood stained nasal discharge for around six months. She experienced mild to moderate headache infrequently. Her illness started about a year back. Initially, there was unilateral nasal congestion with mucopurulent discharge from left nostril. After six months she developed stuffiness of the right nostril too and along with blood stained mucopurulent discharge intermittently. She had no history of cough or respiratory distress or any skin lesion. She was a farmer by occupation. On clinical examination, no mass or polyp was visible in nasal cavity. She was advised CT scan of paranasal sinuses which showed a soft tissue mass filling both maxillary sinuses along with erosion of bony wall of both sinuses and perforation of nasal septum [Table/Fig-1a&b].
(a) CT scan of paranasal sinuses (coronal view). (b) CT scan of paranasal sinuses (axial view).
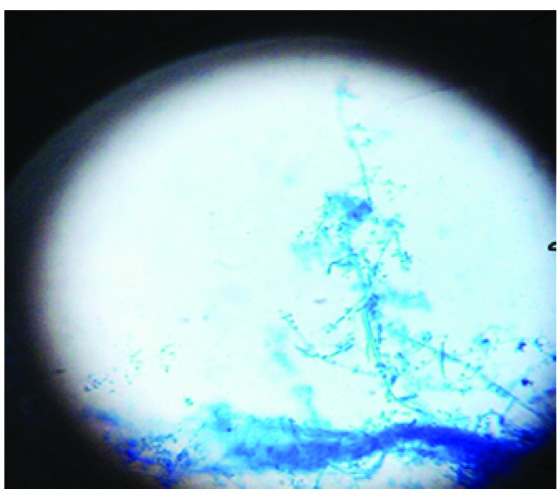
She was planned for FESS (Functional Endoscopic Sinus Surgery) as the mass appeared to be a malignant invasion. Routine preoperative tests were advised. Her blood picture showed Hb%– 10gm%, RBC -3,80,000/ cu.mm, WBC -5,500/ cu.mm, neutrophil-68%, lymphocyte-20%, eosinophil-10%, monocytes-2% and basophil-0%. Postero-anterior view of X-ray chest showed normal bilateral lung fields and cardiac silhouette. On endoscopy both maxilla were seen to be occupied with a soft mass. The bony walls were eroded and perforation of nasal septum was confirmed. The tissue was then removed completely and specimen sent for mycological examination. A portion of same specimen was sent for histopathological study. Mycological study included direct microscopy of the sample in 10% KOH and culture in Sabouraud Dextrose Chloramphenicol Agar (SDCA) medium at 250c and 370c. In KOH mount only few ovoid yeast like structure were seen but no fungal hyphae was visible. Culture at 250C showed the growth of greyish white dirty colony slightly velvety and lobed in obverse side and tanned in colour on reverse side. Microscopic examination with Lactophenol cotton blue demonstrated ovoid micro-conidia clustered like bouquets at the tip of conodiophore resembling the arrangement in Sporothrix species. Few conidia were directly attached to conidiophore by sterigmata. The hyphae were very slender [Table/Fig-2].
LCB mount from colony of Sporothrix spp.
The subculture in Brain heart infusion agar from SDCA maintained at 370C showed the conversion from hyphae to yeast form and colony was moist & creamy in appearance. The histopathplogical study reported the case as allergic rhinosinusitis. No antifungal chemotherapy was given as mycological finding did not correlate with histopathological findings.
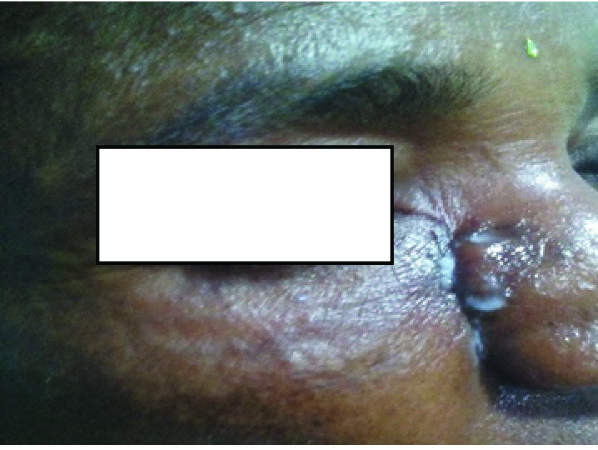
After two months of surgical removal of sinonasal mass the patient returned with a complaint of two discharging sinuses on the right cheek—one near right ala of nose and other at the inner canthus of right eye [Table/Fig-3].
Two discharging sinuses- at ala of nose & at inner canthus of right eye.
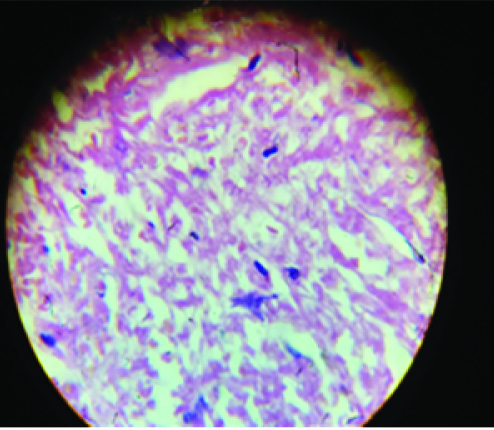
Clinical examination revealed two discharging sinuses. On endoscopical examination, a small mass was seen in right maxillary sinus. The tissue was excised and sent for histopathological as well as mycological study. A 10% KOH mount showed ovoid structures but no hyphae was visible. The colony in SDCA was similar to that which grew previously—the dirty greyish white, slightly velvety and lobed appearance on obverse side and tan coloured reverse. On prolong incubation the colony became tough leathery and dry. Microscopical examination in LCB mount revealed the presence of Sporothrix species again. Histopathological study demonstrated ovoid yeast cells in H&E stained tissue [Table/Fig-4].
H&E Stained tissue from maxillary sinus showing yeast form of Sporothix spp.
Morphological study of the fungus in artificial culture medium demonstrated the mycelial form and histopathological study revealed the yeast form in tissue. The hyphae to yeast and yeast to hyphae conversion was demonstrated by subculture from SDCA to Brain heart infusion agar or BHIA (maintained at 370C) and from BHIA to SDCA (maintained at 250C). On the basis of these findings diagnosis of sporotrichosis of both maxillary sinuses was considered. Speciation of the isolate was not possible as molecular study could not be done. The treatment with amphotericin B for eight weeks was initiated. The sinuses became dry and healed completely [Table/Fig-5]. Then she was prescribed Itraconazole 200 mg orally twice daily for three months.
Healed sinuses (marked with arrow).

The patient has been cured completely of her complaints since completion of treatment.
Discussion
Sporotrichosis caused by Sporothrix schenckii is commonly a chronic pyogranulomatous type infection of cutaneous and subcutaneous tissue [1]. The fungus enters inside the body through traumatic implantation. Occasionally the fungus enters the system on inhalation and commonly causes pulmonary sporotrichosis. In maxillary sinusitis the probable route of entry is inhalational [2]. Sporotrichal infections affecting the sinuses, kidney, subglottic region and retina have been described.
Sporotrichosis is worldwide in distribution but temperate and tropical climate favour its growth. Adult male or female patients are equally affected in skin lesion. In extra cutaneous sporotichosis, marked male preponderance, in widely scattered geographic areas is observed [1]. Occupations that predispose individuals to this infection include gardening, farming, outdoor labour, floral work, masonry etc., involving exposure to contaminated soil, decaying organic matter or sphagnum moss, roses, salt marsh hay or prairie hay [1].
Cutaneous or subcutaneous infection is nodulo-ulcerative in nature and spread through lymph channels proximally. Disseminated invasive form spreads through vascular system [1,2].
Rhinosinusitis may occur due to different type of dimorphic and /or invasive fungi like aspergillus or zygomycetes infection [3]. Only very few case of sporothrix involving maxillary sinuses have been reported worldwide.
Molecular studies have demonstrated that Sporothrix schenckii is a complex species. Marimon and colleagues have proposed three species of Sporothrix like Sporothrix globosa Sporothrix mexicana and Sporothrix brasiliensis [3]. Another species Sporothrix lurie also exists. It is a thermo-dimorphic fungus which is not much virulent and produce chronic granulomatous type lesion [3]. It mainly involves cutaneous and sub cutaneous tissues initiated by penetrating injury introducing the fungus [1,3]. Proximal spread of lymphangitis results in multiple nodular ulcerative lesions along the involved lymphatic channels. This is the most common clinical presentation of this fungal infection. The other type of lesions like disseminated, osteo-articular or pulmonary sporotrichotic infections is infrequent presentation [3]. Infection of nasal sinuses by this fungus has rarely been reported and it is not even seen in patients with severe cutaneous or sub-cutaneous lesions. Pema et al., supported this view by their work where a series of patients suffering from cutaneous sporotrichosis did not develop fungal sinusitis [4]. In India previous report of maxillary sporotrichosis was from a Dental hospital where a patient presented with swelling of right chick along with several discharging sinuses [2]. Aspergillus flavus is predominantly seen in India as the causative agent of Allergic Fungal Rhino Sinusitis (AFRS) [5,6]. It is isolated in 80% cases of AFRS in all over India. A 50% case of AFRS seen in Middle East are also caused by A. Flavus [5]. The work of Patric Tang et al., described that primary etiologic agents in Allergic Fungal Sinusits (AFS) are dematiaceous fungi, especially Bipolaris spicifera or Curvularia lunata and in some geographic regions Aspergillus species, and the basidiomycete Schizophyllum commune. Presumably, the disease begins with colonization of the paranasal sinuses by spores of an airborne fungus [7,8]. In our patient inhalation of conidia is thought to be the route of transmission resulting in such rare mycotic infection of maxillary sinuses. Timely intervention and treatment saved her from further complication of disseminated lesion - extension in orbital area, brain or lungs.
Conclusion
Sporotrichosis of maxillary sinuses though rarely occurs but may be detrimental for patients as invasion to other tissues occurs. A quick diagnosis not only helps in curing the patient but also saves from further complication of disseminated disease as experienced in our patient.
[1]. Kwon-Chung KJ, Bennet J, Medical Mycology 1992 Philadelphia, LondonLea & Febiger [Google Scholar]
[2]. Sandeepa NC, Jaishankar HP, Sarath Candra B, Veena SN, Yeshaswini T, Sporotrichosis of Maxillary sinusWorld journal of dentistry 2011 2(3):269-71. [Google Scholar]
[3]. Chander Jagdish, Textbook of Medical Mycology April 2010 Third editionNew Delhi, IndiaMehta Offset Pvt. Ltd [Google Scholar]
[4]. Yoden B Pema, Shrijana G, Peralam YP, Pradhan J, Uttam P, Peggy T, A case series and review of sporotrichosis in SikkimJ Infect Dev Ctries 2011 5(8):603-08. [Google Scholar]
[5]. Dhingra PL, Diseases of Ear, Nose & Throat 2008 Fourth editionNew Delhi, IndiaElsevier [Google Scholar]
[6]. Sekhar CS, Arunaloke C, Epidemiology and Medical Mycology of Fungal Rhinosinusitis Otorhinolaryngology ClinicsAn International Journal 2009 1(1):1-13. [Google Scholar]
[7]. Tang P, Mohan S, Sigler L, Witterick I, Summerbell R, Campbell I, Allergic Fungal Sinusitis Associated with Trichoderma longibrachiatumJ Clin Microbiol 2003 41(11):5333-36. [Google Scholar]
[8]. Anupama T, Malani Anurag N, Primary Pulmonary Sporotrichosis: Case Report and Review of the LiteratureInfectious Diseases in Clinical Practice 2012 20(Issue 1):25-27. [Google Scholar]