Anterior Cervical Discectomy and Fusion (ACDF) is an established and proven surgical procedure for treatment of degenerative conditions of the cervical spine with predictably good results [1,2]. This procedure works doubly by decompressing spinal cord and increasing neuroforaminal size and volume by anterior interbody distraction in cervical spine [3,4].
After anterior cervical discectomy, intervertebral fusion can be facilitated by using autograft (Iliac crest, fibula), allograft or bone graft substitutes. Cervical spine can be further stabilised by use of anterior cervical plate, standalone cage or combination of both to maintain curvature and decrease pseudoarthrosis rates. Standalone strut graft has high rate of complications such as graft subsidence, dislodgement, non-union and donor site morbidities. Anterior plating also has inherent deficiencies like plate loosening, screw pullout, breakage, trachea-oesophagal irritation has increased operation time [5,6].
Intervertebral cages have been postulated to avoid some of these difficulties due to their self-fixing construct, ability to contain graft or graft substitute in it. In this prospective study, we evaluated two different fusion and fixation methods: autologous tricortical iliac crest bone graft with locked anterior cervical plate and standalone threaded titanium cage stuffed with cancellous bone cylinders harvested using minimally invasive methods.
Study was conducted to analyse safety and efficacy of tricortical autograft and anterior cervical plate with cylindrical titanium cage filled with cancellous bone in procedure of ACDF for single level degenerative cervical disc disease.
Materials and Methods
The study was carried out in tertiary care referral cum teaching hospital from April 2012 to May 2015. Twenty patients with single level degenerative cervical disc disease in subaxial spine were included in study. After a detailed assessment of neurological status and co-morbidities, radiological confirmation of diagnosis was done with plain radiographs of cervical spine and magnetic resonance imaging. Patients were planned for anterior cervical discectomy and fusion after a fair trial of non-operative measures for at least 8 weeks and failure to obtain patient defined relief.
Mode of fusion and surgical technique was assigned to equal half patients based on computer generated randomisation. 10 patients were operated with Tricortical Iliac Crest autograft and anterior cervical locking plate (Group A) while 10 patients were operated with non-coated threaded cylindrical titanium cage stuffed with cancellous bone harvested using minimally invasive measures (Group B) for fusion after discectomy. The clinical and demographic profiles were comparable in both groups [Table/Fig-1].
Patient particulars undergoing ACDF for degenerative cervical spine disease.
| Parameters | Tricortical graft with plate group | Cage group |
|---|
| Number of patients | 10 | 10 |
| Male/female | 7/3 | 6/4 |
| Mean age | 49.8(37-59) | 52.3(39-62) |
| Follow-up period | 15.4 months (9-32 months) | 16.1 months (9-31 months) |
| Involved levels |
| C3-C4 | 1 | 0 |
| C4-C5 | 1 | 1 |
| C5-C6 | 4 | 5 |
| C6-C7 | 4 | 4 |
Surgical Approach
All the patients were operated by same surgeon. Patients were operated in supine position with a small bolster under scapular blades to ensure partially extended position of neck. Level of skin incision was ascertained with help of intraoperative fluoroscopy. Transverse skin incision was given from midline till medial border of the sternocleidomastoid muscle at the appropriate level of vertebral pathology. Fascial sheath and platysma were incised in the line of skin incision. Deep cervical fascia immediately anterior to the sternocleidomastoid muscle was incised.
Sternocleidomastoid muscle was retracted laterally and strap muscles (sternohyoid and sternothyroid) were retracted medially. Carotid pulsations were localized with digital palpation and dissection plane was developed between medial edge of carotid sheath and the midline structures by blunt dissection of pretracheal fascia on the medial side of carotid sheath. Carotid sheath with its enclosed structures and sternocleidomastoid were retracted laterally. Plane was developed deep to pretracheal fascia. Prevertebral fascia including anterior longitudinal ligament were divided, and Longus colli muscle was reflected subperiosteally from anterior aspect of vertebral body.
After exposing the site of involved vertebrae, level of disc to be operated was confirmed by image intensifier. Stab knife was used to cut anterior longitudinal ligament and annulus fibrosis. All possible disc material was removed. Partial curetting of end plate were done. This prevents post operative graft collapse or cage subsidence. Cages can sit through end plates to subchondral bone by their threads. Cage size was determined by preoperative templating, intraoperative evaluation using a trial cage and fluoroscopic guidance.
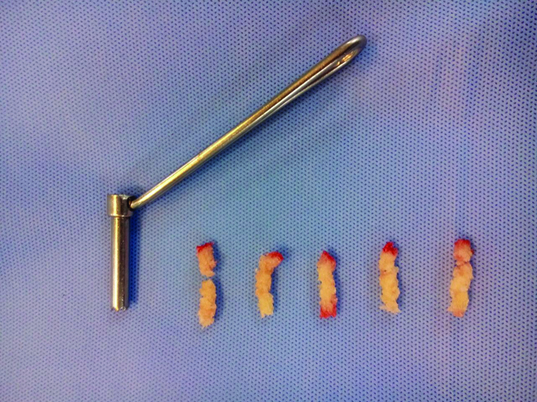
Cage was filled with cylinder of cancellous bone harvested from iliac crest with minimal invasion using a specially made graft harvesting sleeve [Table/Fig-2]. After a small stab incision over widest palpable portion of iliac crest, a sleeve with cutting edges at end and trocar was secured at iliac crest. After removal of trocar, with rotatory movements in direction of iliac blade, sleeve carve out a cylinder of cancellous bone between two tables of ilium. Stability of graft or cervical cage was checked intraoperatively under vision. Anterior locking cervical plate was used for additional fixation in patients receiving tricortical graft. Wound was closed in layers.
Graft harvesting technique cancellous cage stuffing.
Patient’s neck was immobilised in Philadelphia cervical collar post-operatively. Assisted side turning was permitted on same day of surgery. The patients were followed up at regular intervals and examined for relief of pain, neurological status, radiological examination to know the position of grafts its incorporation, position of implant and any complication.
During follow up patients were advised to continue use of Philadelphia cervical collar for 3 months, active and passive motion exercises of extremities were started. On follow-up other than neurological reassessment, radiographs of cervical spine in lateral projection were done to assess for union activity. All patients have minimum of 9 months follow up with range from 9 months to 3 years.
Clinico-Radiological Evaluation
Evaluation of results was done by using criteria suggested by Odom et al., [7,8], Visual pain analogue (VPA) scale [8], activity of union on lateral projection radiographs of cervical spine and overall satisfaction of patient with treatment.
Odom et al., classified functional results as excellent, good, fair, or poor based on union activity between vertebral bodies, radicular symptoms and neurological recovery. Neurological involvement was assessed for motor, sensory, autonomic functions and peripheral reflexes. Motor power was graded based on MRC (Medical Research Council) criteria.
A fusion was considered solid when osseous trabeculae bridged the disc space on lateral radiograph. In cases of threaded titanium cervical cage fusion was considered solid, when on lateral flexion and extension radiograph, the difference of distance between tips of spinous processes at fusion levels was less than 2 mm [8,9]. Patients with persistent symptoms or deteriorating symptoms were planned for further evaluation by magnetic resonance imaging. However, patients with good postoperative functional outcome and radiographic fusion were excluded for postoperative MRI.
VPA Score was measured using Visual pain analogue scale. Patient is asked to indicate perceived pain intensity along a 100 mm horizontal line. A score of 0 mm indicate absence of pain & 100 mm as worst pain even experienced by the patient.
Results
1. Radiological Fusion
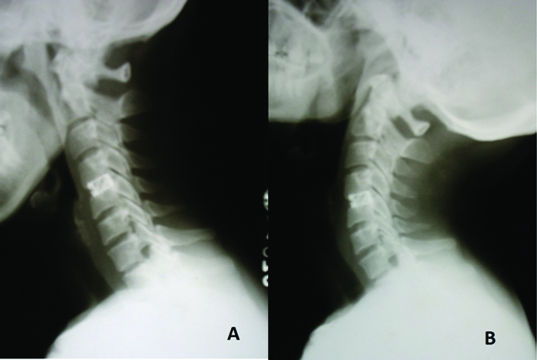
Fusion was achieved in all patients in both groups with duration for fusion ranging from 3- 7 months in both groups with mean duration in tricortical graft group 4.7 months (3-7 months) and cage group 4.2 months (3-6 months) [Table/Fig-3,4].
Flexion extension cage-acdf C4-C5.

Segmental kyphosis was noted in one patient of tricortical graft group associated with partial graft extrusion and graft collapse. But presence of graft collapse and segmental kyphosis was not associated with adverse clinical outcome.
2. Odams criteria
In 90% (9 each) patients of ACDF with cage and tricortical group was having excellent to good result [Table/Fig-5]. One patient in each group had poor results due to persistent radiculopathy and neck pain.
Odam’s clinic-radiological criteria for functional assessment after cervical discectomy and fusion.
| Excellent | Solid fusion on radiograph. No neck or arm pain. Normal finding on neurological examination.
|
| Good | Solid fusion on radiograph. No neck or arm pain. Neurological improvement with mild residual problem.
|
| Fair | Solid fusion on radiograph. Persistent neck or arm pain, Post operative myelogram or magnetic resonance imaging reveals no additional neurological compression.
|
| Poor | Continued symptomatic nonunion Neurological worsening Need for a reoperation.
|
3. VPA Score
There is significant improvement in VPA score in all patients except one in each group after ACDF in both groups at last follow-up. Mean preoperative VPA score in tricortical graft was 62 (range 39-82) which decreased significantly to new mean level of 21 (range 9-47). Similarly, in cage group mean preoperative score was 66(range 33-86) which reduced to a new level of 21(range 5-51) The mean improvement of VPA score after surgery was 41 in tricortical graft group and 45 in cage group [Table/Fig-6].
Functional outcome in both groups: Odom’s criteria, Visual pain analogue score.
| Cage group | Plate + graft group |
|---|
| Radiological fusion |
| • No of patients | 10 | 10 |
| • Non-union | None | None |
| • duration | 4-6 months | 4-7 months |
| VPA score improvement | Mean 45(range 21-59) | 41(29-62) |
| Odom rating of outcome | Excellent- 6 | Excellent - 5 |
| Good- 3 | Good- 4 |
| Fair - 0 | Fair - 0 |
| Poor 1 | Poor - 1 |
4. Neurological improvement
Neurological deficit was present preoperatively in 7 among tricortical graft group and 9 in cage group. There was improvement in neurological status in all patients within 6 months after surgery. Motor deficit was first to improve followed by sensory deficit. Exaggerated reflexes and hypertonia was last to wane.
5. Complications and Patient satisfaction
No intraoperative complication was encountered in any patients. None of patient had post-procedure neurological deterioration. Dysphagia was noted after surgery in 3 patients (two in tricortical graft group and one in cage group), which was transient to settle within a week in all patients. In immediate postoperative period, appropriate positioning of cage and graft was confirmed by bedside radiographs. Partial graft extrusion and graft collapse was present in one patient in tricortical group. Three instances of donor site morbidity were present in group A one having superficial stitch infection and two having chronic operative site pain. Patient satisfaction as reported by patients at the end of follow up was 90% in each group.
Discussion
Anterior cervical discectomy and fusion is established modality for treatment of degenerative conditions of cervical spine with radiculopathy [1,4,5]. Various modifications and methods have emerged in clinical practice without establishing superiority of one over other. One such aspect of procedure with multiple methods in practice is modality to facilitate fusion [5,8,9].
Goal of fusion after anterior cervical discectomy is to provide stability to spinal column. Use of tricortical graft with plate or Biomechanical disc spacers like cage restores the height of the disc space by relieving buckling of posterior longitudinal ligament and ligamentum flavum. This in turn relieves cord compression and restores volume of the neural foramen thereby decompressing nerve root by the principle of ligamentotaxis. A fusion diminishes neural irritation by limiting motion and by allowing resorption of osteophytes partially [8–10].
Conventionally, tricortical autograft is considered gold standard for fusion which provides osteogenic, osteoinduction and osteoconduction properties to graft along with mechanical strength owing to cortical struts in it. Such ideal fulfilments come with another set of concerns like graft collapse, graft extrusion and donor site complications. Graft has poor self-fixing characteristics and it can extrude, collapse or fail to heal resulting in symptomatic pseudoarthrosis [5,10,11]. Prevention strategy for such complications requires addition or augmentation of fixation with anterior plate system. Minimal invasive harvesting of iliac crest graft aims to minimise various complications of graft harvesting, while giving benefits of autograft. Essentially, it saves surgical time by avoiding complex en-block harvesting of tricortical graft fills cage very well due to cancellous nature. Allograft eliminates donor site morbidity but having chances of disease transfer like HIV or hepatitis, though very rare [12].
Newer surgical techniques attempt to eliminate donor site morbidity and graft related complications. Extrapolating from lumbar spine experience, a titanium cervical cage is proposed as an alternative method for cervical spine fixation and fusion simultaneously providing strength of cortical strut and osteogenic potential with minimal morbidities [12]. Biomechanical spacer made of materials like Polyetheretherketone (PEEK), Methymethacrylate, Hydroxyappetite ceramics and Implant made of carbon fiber, titanium, tantalum etc are there in use. Interbody fusion cages rely on the principle of annular tensioning (ligamentotaxis) restoring disc height and volume and size of neuroforamen indirectly [10,11,13]. Threaded titanium cages have advantage of providing immediate stability, minimising donor site morbidity, easier implantation technique having less operative time and less chances of cage related complication [11,14–18].
Cage subsidence is most common complication associated with standalone cages with varied incidence rate by various investigators [16–19]. Barsa et al., reported 19 of 144 inserted cages (13.2%) subsided in his series [19], while Bartels et al., noticed an incidence of 29.2% in series of 69 patients [20]. In our patients, we reported no incident of cage subsidence. Intraoperative fluoroscopic assessment of stability and adequate immobilisation in postoperative period may help avoidance of few incidents of cage displacement.
Clinical outcome (fusion and symptomatic relief) is independent to incidence of cage subsidence and does not correlate with it. Moon et at., Bartels et al., and Gereck et al., found no correlation between poor functional outcome and cage subsidence [18–21]. Graft subsidence also seems to be independent of functional outcome. One patient in our series had graft subsidence, but good functional outcome. In our series, persistent pain in one patient in each group was evaluated with MRI and adjacent disc disease was incriminated as cause of pain and poor satisfaction at the end of treatment.
Various cage materials have been studied in comparative studies. Titanium cage and PEEK cages have been compared with respect to physical properties, functional outcome and incidence of complications. Although modulus of elasticity is higher for titanium cages, it does not translate into higher incidence of complications with use of titanium cages as compared to other cage designs. Cabraja et al., did not found any statistical difference between two materials of cage with respect to cage subsidence, fusion rates and lordosis maintenance [22].
Thom et al., found cage as safe modality for fusion as compared to tricortical autograft with better functional outcome in cage group with a concern for graft donor site morbidity [23]. In our study also, although functional outcome of both groups is comparable with similar complication profile, graft site morbidity occurred in three patients in tricortical group. Every study has some drawbacks, so has our study. An investigator blinded study will larger number of study subjects will establish true clinical superiority of one technique over other.
Cancellous graft required in cage group is small in volume and can be easily harvested using trochar-sleave instruments as shown in [Table/Fig-2]. It yields small cylinders of pure cancellous bone, which can be easily stuffed in titanium cage. It is minimally invasive and does not inflict donor site morbidity associated with harvesting and dissection of large tricortical graft.
Conclusion
Use of titanium cage filled with cancellous graft is a less invasive, simple procedure for anterior cervical discectomy and fusion. It reliably alleviates cervical degenerative radiculopathy by attaining adequate interbody fusion. Authors conclude that titanium cages after cervical discectomy constitute a safe and equally efficient alternative to iliac crest autograft and anterior cervical plating by providing adequate stability. Minimally invasive harvesting of cancellous graft saves surgical time and various complications associated with other methods.