Peritonitis continues to be one of the major infectious problems confronting a surgeon. Peritonitis due to hollow viscus perforation is one of the most common surgical emergencies to be attended by a surgeon on call duty. This may be due to persistence of the various risk factors among the general population like H.pylori infection, non-steroidal anti-inflammatory drugs, enteric fever and several others. This condition most of the times needs an emergency surgical intervention. Despite many advances in anti-microbial and supportive care, the mortality rate of diffuse suppurative peritonitis remains unacceptably high. The treatment of peritonitis and the evaluation of different therapeutic approaches are hampered by lack of precise classification. A scoring system should be able to assess the need, type and quality of the care required for a particular patient.
Several scoring systems are in place to stratify the patients with peritonitis due to hollow viscous perforation like Peptic Ulcer Perforation (PULP) score, Acute Physiology and Chronic Health Evaluation, BOEY score [1–6]. Utilization of scoring systems would be of great help in salvaging a priceless life by risk stratification with preferential care and by surgical audit.
Realizing the need for a simple accurate scoring system in these conditions the present study was undertaken to evaluate the performance of three different scoring systems in predicting the risk of mortality in patients with peritonitis due to hollow viscus perforation.
Hence the aim of this study is to identify a scoring system which is most accurate at predicting the outcome and thus help in prognostication of the patient.
Materials and Methods
Patients admitted in the surgical ward with a diagnosis of perforation peritonitis during the period of December 2012 to August 2014 were included in the study. Total number of cases were 100.
The study was a prospective and observational study so a detailed history of general physical and systemic examination was obtained.
All cases with signs and symptoms of perforative peritonitis due to traumatic, infective and neoplastic aetiology were included. Cases of primary and tertiary peritonitis, iatrogenic and pediatric patients were excluded. A detailed clinical history was taken regarding the symptoms which included abdominal pain, abdominal distension, vomiting, altered bowel habits, and fever along with the duration of symptoms. History of other co-morbid conditions like diabetes mellitus, hypertension was taken. Details regarding past history of any significant cardiac or respiratory history, history of invasive procedures, drug intake and personal history were taken.
General examination of the patient included the assessment of the vitals i.e. pulse, blood pressure, central venous pressure, temperature, Glasgow Coma Scale (GCS) and respiratory rate.
Detailed per abdomen examination of the patient included tenderness, guarding, rigidity and a palpable mass all checked for. The remaining systemic examination included the respiratory system, cardiovascular system and the central nervous system.
All patients underwent routine biochemical investigations which included the blood counts, renal function tests, serum electrolytes, liver function tests and arterial blood gases, bedside bleeding and clotting time measurements, radiological investigations such as x-rays of chest and erect x-ray of abdomen along with ultrasonography of abdomen and pelvis and electrocardiogram. In patients with free air under diaphragm demonstrated by erect x-ray abdomen or pyoperitoneum demonstrated by ultrasound, computed tomography of the abdomen was not done. CT of abdomen was done in 6 cases.
All patients on admission were identified to have septic shock and started on volume resuscitation with two large bore IV lines (16 gauge) with bolus administration of 20 ml/kg crystalloid, patients were catheterized to monitor urine output and maintain an output of more than 30 ml per hour. Central venous access obtained and central venous pressure monitored. 8-12 mmHg pressure was used as the target central venous pressure. Blood cultures were obtained and empirical antibiotics started. Antibiotics on admission included third generation cephalosporin with amikacin and metronidazole. Patients with fecal contamination were put on higher antibiotics like pipercillin and tazobactam. Antibiotics were changed according to culture sensitivity reports. Doses were adjusted according to creatinine clearance in patients with renal insufficiency. Patients were also given ranitidine, an H2 receptor blocker. If after 4 litres of crystalloid solution administration patient still remained hypotensive, patient was started on vasopressor support with norepinephrine to maintain a mean arterial pressure of more than 65 mmHg.
All necessary surgical procedures which included primary closure of the perforation, resection anastomosis of the diseased bowel segment and closure with proximal diverting stomas were done as indicated with proper written informed consent. Intra-operative findings of total blood loss, site of perforation, presence of malignancy, peritoneal contamination were noted. All patients were given adequate postoperative care. Parameters such as wound soakage, appearance of bowel sounds, chest infections, postoperative shock and duration of stay postoperatively were noted. Wound swab culture sensitivity was sent when indicated. The data regarding the patient particulars, diagnosis, investigations, surgical procedures and outcome were collected in a case recording form.
All these data were transformed to a master chart and individual scores calculated for each patient using the following scoring system [Table/Fig-1,2 and 3]. Subjected to statistical methods to compare the three systems in prediction of mortality. Patients were divided into survivors and non-survivors. Individual scores were calculated for each patient. Accuracy of scoring systems were assessed.
Showing the POSSUM scoring sytem.
| Physiological score |
|---|
| Score | 1 | 2 | 4 | 8 |
|---|
| Age (years) | < 60 | 61-70 | > 71 | |
|---|
| Cardiac history | Nil | Drug treatment | Oedema/warfarin | Raised JVP cardiomegaly |
| Chest X-ray | Normal | | Borderline cardiomegaly | |
| Respiratory historyChest X-ray | Normal | Dyspnoea on exertionMild COPD | Limiting Dyspnoea (on flight stairs) Moderate COPD | Dyspnoea at rest Fibrosis/consolidation |
| Systolic blood pressure (mmHg) | 110-130 | 131-170 or 100-109 | >171 or 90-99 | <89 |
| Pulse rate (b.p.m) | 50-80 | 81-100 or 40-49 | 101-120 | <39 or >121 |
| GCS | 15 | 12-14 | 9-11 | <8 |
| Urea (mmol/L) | <7.5 | 7.6-10 | 10.1-15 | >15.1 |
| Haemoglobin (g/L) | 130-160 | 115-120 or 161-170 | 100-114 or 171-180 | <99 or >181 |
| White cell count (x109/L) | 4-10 | 10.1 – 20 or 3.1 - 4 | >20.1 or < 3 | |
| Sodium (mmol/L) | >136 | 131-135 | 126-130 | <125 |
| Potassium (mmol/L) | 3.5-5 | 3.2-3.4 or 5.1-5.3 | 2.9-3.1 or 5.4-5.9 | </= 2.8 or >/= 6 |
| ECG | Normal | | MI>6 months ago AF rate < 90 | MI<6 months ago AF rate > 90 min |
| Operative Severity Score |
| Score | 1 | 2 | 4 | 8 |
| Magnitude | Minor | Intermediate | Major | Major+ |
| Number of operative | 1 | 2 | >2 | |
| Blood loss per (ml) | <100 | 101-500 | 501-999 | >1000 |
| Peritoneal soiling | None | Serous | Local pus | Free bowel content, pus or blood |
| Malignancy | None | Primary only | Node metastases | Distal metastases |
| Timing of operation | elective | - | Emergency >2 h of resuscitation possible; operation within 24 hours | Emergency < 2h (immediate surgery needed) |
b.p.m beats per minute, COPD Chronic Obstructive Pulmonary Disease GCS Glasgow Coma Scale JVP jugular venous pressure, each of the 12 rows is scored accorrding to patient factors. These scores are added to gave a physiological score for the patient.
Physiological score.
Showing Mannheim Peritonitis Index.
| Risk factor | Score |
|---|
| Age > 50 years | 5 |
| Female sex | 5 |
| Organ failure* | 7 |
| Malignancy | 4 |
| Preoperative duration of peritonitis > 24 h | 4 |
| Origin of sepsis not colonic | 4 |
| Diffuse generalized peritonitis | 6 |
| Exudates: | |
| Clear | 0 |
| Cloudy, purulent | 6 |
| Fecal | 12 |
*Kidney failure: Cratinine level > 177 mmol/L or urea level > 167 mmol/L or oliguria < 20 mL/h; pulmonary insufficiency: PO2 < 50 mmHg or PCO2 > 50 mmHg; intestinal obstruction/paralysis > 24 h or complete mechanical ileus; shock hypodynamic or hyperdynamic.
Showing the Sepsis score of Stoner and Elebute.
| Scoring of Local effects of tissue infection |
| ATTRIBUTE | SCORE |
| Wound infection with purulent discharge/entero-cutaneous fistulaRequiring only light dressing changed not more than once dailyRequiring to be dressed with a pack, dressing needing to be changed more than once daily, requiring application of a bag and/or requiring suction | 24 |
| Peritonitislocalizedgeneralized | 26 |
| Chest infectionsclinical or radiological signs of chest infection without productive coughclinical or radiological signs of chest infection with cough producing purulent sputumfull clinical manifestation of lobar/bronchopneumonia | 246 |
| Deep seated infection (subphrenic abscess, pelvic abscess, empyema Thoracis, acute or chronic osteomyelitis) | 6 |
| Scoring of pyrexia |
| ATTRIBUTE | SCORE |
| Maximum daily temperature (degree Celsius)36-37.437.5-38.438.5-39>39<36Minimum daily temperature > 37.5If 2 or more temperature peaks above 38.4 in 1 dayIf any rigors occur in a day | 01233add 1add 1add 1 |
| Scoring of secondary effects of sepsis |
| ATTRIBUTE | SCORE |
| Obvious jaundice (in the absence of established hepatobiliary disease)Metabolic acidosisCompensatedUncompensated | 212 |
| Renal failureGross disturbance of mental orientation level of consciousness and/ or otherFocal neurological manifestations of pyaemia, septicaemiaBleeding diathesis (from disseminated intravascular coagulation) | 333 |
| Scoring of laboratory data |
| ATTRIBUTE | SCORE |
| Blood cultureSingle positive cultureTwo or more positive cultures separated by 24hrSingle positive culture + history of invasive procedureSingle positive culture + cardiac murmur &/or tender enlarged spleen | 1333 |
| Leucocyte count(* 109/l)12-30>30<2.5 | 123 |
| Haemoglobin level in the absence of obvious bleeding (g/dl)7-10<7 | 12 |
| Platelet count (*103/l)100-150<100 | 12 |
| Plasma albumin level(g/l)31-3525-30<25 | 123 |
| Plasma total bilirubin level in the absence of clinically obvious jaundice >25μmol/l | 1 |
Results
In the study 100 diagnosed cases of perforation were included, 97 of which underwent laparotomy, two patients had drain inserted under local anaesthesia and one patient died before any procedure. Three patients underwent more than one procedure, two of whom underwent resection anastomosis following primary closure and one patient had an ileostomy done after primary closure of the perforation. The total number of deaths was 16 contributing to mortality rate of 16%. Maximum patients were in the age group of 30 to 50 with the trend line being around 40 years; the median age of patients who survived was 40 years while in patients who died the median age was 60 years [Table/Fig-4].
Clinical details of the 100 patients studied.
| Variable | Survived | Died | p-value (Mann-Whitney test, Fischer’s exact test or chi-square test) |
|---|
| Age (in years) | 40 | 60 | 0.0001 |
| Sex | | | |
| males | 64 | 13 | 0.47 |
| females | 20 | 3 | |
| Symptoms (in days) | 2 | 4.5 | 0.0000 |
| Shock | | | |
| present | 7 | 14 | 0.0000 |
| absent | 77 | 2 | |
| Multi organ failure | | | |
| present | 9 | 13 | 0.0000 |
| absent | 75 | 3 | |
| Hospital stay (in days) | 7 | 3.5 | 0.0013 |
There were more males (77%) than females (23%), 64 out of 77 male patients survived and 20 out of 23 female patients survived. Patients who survived had symptoms for median duration of two days while those who died had symptoms for 4.5 days. Two thirds of patients in septic shock stage 3 or higher i.e. 14 of the 21 patients died.
Multiple organ failure defined by creatinine level > 177 umol/L or urea level> 167mmol/L or oliguria 20ml/hour; Pulmonary insufficiency (PO2 < 50 mmHg or PCO2 > 50 mmHg), Intestinal obstruction/paralysis (> 24hours or complete mechanical ileus) and Shock (systolic blood pressure<90mmHg, mean arterial pressure<60mmHg) was present in 22 patients of which 13 expired.
The average duration of hospital stay was found to be seven days for patients who survived as opposed to 3.5 days in those who died. This can be attributed to the fact that patient who presented late with advanced stages of the disease died early.
In the study, it was found that 47 of our patients had gastro duodenal perforations, 34 patients had gastric perforation predominantly prepyloric region and 13 patients had duodenal perforation. None of these 47 gastroduodenal perforation were of malignant aetiology. Of these 47 gastroduodenal perforations four died, followed by ileal perforations, 27 of them of which four died. Appendicular perforations were 13 in number with no deaths. There were five patients with colonic perforations with one mortality and all four patients with jejunal perforations died. We also had one uterine perforation. In the study, there were three patients who presented in the advanced stage of the disease, drains inserted under local anaesthesia in pelvic and in subhepatic regions was the only treatment two of these patients received before succumbing to the disease whereas the third patient died before any intervention could be undertaken [Table/Fig-5].
Site of perforation, type of contamination, aetiology and procedure done in study patients.
| Variable | Number of patients | Number that died | p-value |
|---|
| Site of perforation (n=100) |
| Appendicular | 13 | 0 | 0.0000 |
| Colonic | 5 | 1 |
| Gastroduodenal | 47 | 4 |
| Ileal | 27(1 multiple) | 4 |
| Jejunal | 4 | 4 |
| Uterine | 1 | 0 |
| Unknown | 3 | 3 |
| Peritoneal contamination (n=99) |
| Generalised and cloudy purulent exudate | 52 | 7 | 0.001 |
| Generalised and clear | 13 | 0 |
| Generalised and feculent | 13 | 8 |
| Localised and cloudy purulent exudate | 10 | 0 |
| Localised disease with local pus | 7 | 0 |
| Localised disease with clear exudate | 4 | 4 |
| Extent of the disease (n=99) |
| Generalized | 78 | 15 | 0.001 |
| Localised | 21 | 0 | |
| Aetiology (n=97) |
| peptic ulcer disease | 47 | 4 | 0.000 |
| appendicitis | 13 | 0 |
| typhoid | 17 | 0 |
| diverticular disease | 1 | 1 |
| ischemic bowel | 4 | 4 |
| malignancy | 1 | 0 |
| obstruction | 3 | 1 |
| tubercular | 7 | 3 |
| trauma | 3 | 0 |
| uterine | 1 | 0 |
| Procedure done (n=100) |
| resection anastomosis | 10 | 8 | 0.000 |
| primary closure | 67 | 3 |
| appendectomy | 13 | 0 |
| hysterectomy | 1 | 0 |
| drains under local | 2 | 2 |
| closure with tube duodenostomy | 1 | 1 |
| closure with diverting colostomy | 2 | 0 |
| closure and ileostomy | 1 | 0 |
| closure and RA | 2 | 1 |
There were 78 patients who had generalised disease of which 15 died and those who died had either feculent or purulent exudate and all of the 21 patients with localised disease survived.
In the study 67 patients underwent primary closure with three deaths. In ten patients resection anastomosis were done of whom eight died, three of them were due to Superior Mesenteric Artery thrombosis,one case of jejunal diverticular disease who had multiple jejunal diverticuli in the mesenteric border with three perforations of the bowel at 10cm, 30cm and 55cm from the ligament of Treitz and three cases of tubercular perforation requiring extensive resections. Three patients had undergone a second procedure following primary closure. Resection and anastomosis in two, of which one died and ileostomy in the other. All 13 patients who underwent appendectomies survived. One patient had a 1.5 cm perforation of the junction of the first and second part of duodenum, patient underwent a decompressive gastrostomy with pyloric exclusion, tube duodenostomy and feeding jejunostomy as the treatment but didn’t survive. Primary closure with diverting proximal stoma was done in two patients. Hysterectomy was done for the pyometra with uterine perforation.
Discussion
Preoperative duration of symptoms is a significant contributing factor for the prognosis of the patient. With time the disease progresses to become generalised peritonitis followed by multi system involvement which adversely affects the outcome of the patient. The average duration of hospital stay was found to be seven days for patients who survived as opposed to 3.5 days in those who died. This can be attributed to the fact that patient who presented late with advanced stages of the disease died early.
The mortality was confounded by the aetiology as three cases with jejunal perforation had superior mesenteric artery thrombosis and one case had extensive jejunal diverticuli with multiple diverticular perforation and one case of multiple ileal perforation had abdominal Kochs. All of them required extensive resection of the involved segment of the intestines.
Most of the patients who died had advanced disease, requiring extensive resection like Superior Mesenteric artery thrombosis, tubercular peritonitis and complicated diverticular disease. All the patients with ischemic bowel disease died, three patients with tubercular peritonitis died. The median MPI scores were 24.5 in those who survived and 33.5 in those who died. By multiple logistic regression method and by using Receiver Operating Characteristic (ROC) curves, the area under the curve was 0.95 which indicates that the Mannheim Peritonitis Index is a good scoring system to predict mortality in the cases of perforation peritonitis [7–12] [Table/Fig-6].
Showing median scores and area under ROC curves of the three scores.
| Scores | Survived | Died | p-value | AUC |
|---|
| MPI | 24.5 | 33.5 | 0.0000 | 0.95 |
| POSSUM | 40 | 58.5 | 0.0000 | 0.99 |
| Sepsis score | 11 | 25 | 0.0000 | 0.98 |
The median POSSUM score for those who survived was 40 and those who died was 58.5. By multiple logistic regression method, the area under the ROC curve was 0.99. POSSUM score is an excellent score for prediction of mortality [13–16].
The median sepsis score for those who survived was 11 while it was 25 in those who died. The area under the curve was 0.98. Sepsis score is an excellent predictor of mortality [17].
An optimal cut off point is one at which the maximum values of sensitivity and specificity of the score can be obtained and it is identified from the ROC curve.
ROC curves are plotted by using sensitivity and specificity. Sensitivity is plotted along the y-axis and specificity along the x-axis i.e. true positive rate versus the false positive rate. At different points on the curve, the sensitivity and specificity of the test vary as they are inversely proportional.
Thus, of the three scores POSSUM and Sepsis score were excellent in prediction of outcome (accuracy > 93%). POSSUM, with a slightly low positive predictive value, over predicted mortality. Although MPI had a sensitivity and specificity of more than 80 %, was inferior as compared to the above two scores in prediction of outcome accurately (accuracy 82.8%). With a low positive predictive value of 46% MPI also over predicted mortality. Even optimisation of the cut-off point does not achieve acceptably low false positive rate of prediction to justify the use of score in the care of individual patients [Table/Fig-7].
Showing sensitivity, specificity, accuracy and predictive values of the scores.
| Score | Sensitivity (%) | Specificity (%) | Accuracy (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|
| MPI score 29 | 80 | 83 | 82.8 | 46 | 96 |
| POSSUM score 51 | 92.3 | 94.04 | 93.8 | 70.5 | 98.75 |
| Sepsis score 22 | 86.67 | 97.5 | 95.9 | 86.67 | 97.5 |
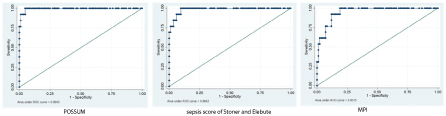
These data suggest that with an area under curve of 0.99 POSSUM score predicted mortality more accurately than MPI (0.95) and Sepsis score of Stoner and Elebute (0.98) in patients of perforative peritonitis undergoing surgical management of the underlying condition [Table/Fig-8]. However, all the three scores with area under the curve of more than 0.95 are good scores in prediction of mortality. If ease of calculation of scores is taken into consideration, Mannheim peritonitis index with few variables needed for calculation which can be obtained in a short time period and very little intra operative details and POSSUM score which has two components, physiological and operative severity, seem easier to calculate than the Sepsis score which requires postoperative information about local effects of tissue infection and information about blood culture sensitivity reports which take longer, up to four days or even more at times, so the final score can only be calculated after that. Thus none of these scores are strictly preoperative.
Limitation
The fundamental difficulty in prediction of outcome in patients with peritonitis is the occurrence of unpredictable complications. Unforeseen events may occur that influence the course of the disease. Furthermore, the diversity and individuality of biological response may prevent accurate prediction in quite a large proportion of the patients. In this respect we must find out, with further studies, whether in these group of patients having inaccurate predictions, whether the prediction instrument is faulty or data is inadequate [18].
Conclusion
Increasing age of the patient, longer duration of symptoms, advanced disease process, generalised peritonitis with purulent or feculent exudate, shock at presentation and development of multi organ failure are all associated with mortality and contribute to dismal outcome of the patient significantly. Gender of the patient has no bearing on the outcome of the patient in the similar risk group.
Although all the three scores are good predictors of mortality, POSSUM and sepsis score of Stoner and Elebute are excellent predictors of outcome in terms of accuracy as compared to MPI. Both POSSUM and MPI, with a slightly low positive predictive value, over predict mortality rate in a borderline and/or equivocal risk group.
b.p.m beats per minute, COPD Chronic Obstructive Pulmonary Disease GCS Glasgow Coma Scale JVP jugular venous pressure, each of the 12 rows is scored accorrding to patient factors. These scores are added to gave a physiological score for the patient.
Physiological score.
*Kidney failure: Cratinine level > 177 mmol/L or urea level > 167 mmol/L or oliguria < 20 mL/h; pulmonary insufficiency: PO2 < 50 mmHg or PCO2 > 50 mmHg; intestinal obstruction/paralysis > 24 h or complete mechanical ileus; shock hypodynamic or hyperdynamic.