Nescient Aetiology of Splenic Laceration – An Enigma Unveiled
Saraswathy Sreeram1, Hanaganahalli B Sridevi2, Urmila N Khadilkar3, Deepa Adiga4
1 Postgraduate Student, Department of Pathology, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
2 Assistant Professor, Department of Pathology, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
3 Professor, Department of Pathology, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
4 Associate Professor, Department of Pathology, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hanaganahalli B Sridevi, Assistant Professor, Department of Pathology, Kasturba Medical College, Manipal University, Mangalore, Karnataka- 575 003, India.
E-mail: drsri.20@gmail.com
Malaria is a common endemic disease prevalent in developing countries like India that presents with wide spectrum of clinical symptoms and complications. Splenic rupture is an uncommon but life-threatening complication which can be either spontaneous or as a result of trauma. We present a case of 50-year-old man with left upper quadrant pain following a polytrauma. Based on the radiological evidence of laceration and rupture of markedly enlarged spleen, emergency splenectomy was performed. Postoperative haematological evaluation established the co-infection of Plasmodium falciparum and vivax with high parasitaemia and marked thrombocytosis. The incidences of splenic rupture due to malaria are under-reported. In endemic areas, the management of splenic rupture in malaria should be focused on splenic preservation, thereby reducing the risk of future attacks of malaria in those patients who are highly susceptible to Plasmodium species and also reducing the incidence of overwhelming sepsis.
Endemic, Malaria, Splenic rupture, Thrombocytosis
Case Report
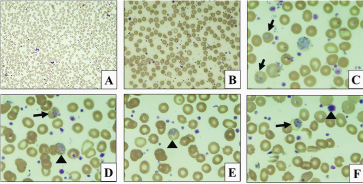
A 50-year-old man was admitted in surgery ward (Postoperative) and was evaluated routinely for complete blood counts and peripheral smear examination. The thin blood smear showed normocytic normochromic anaemia (Hb-8.4g/dL), with significant polychromasia and presence of few normoblasts. There was also neutrophilic leucocytosis (24,600 per mm3) and thrombocytosis (7.8 lakhs per mm3) with many giant platelets and platelet clumps. High malarial parasitaemia (more than 50% of parasitized RBCs) with both Plasmodium vivax and Plasmodium falciparum species was observed [Table/Fig-1a-f]. Thick blood smear also revealed high parasitaemia (3+). A retrospective evaluation was done for the unusual coexistence of thrombocytosis with mixed malaria of high parasitaemia. It revealed that the present patient admission was for a routine hospital care. He had undergone splenectomy 10 days ago in a peripheral hospital for splenic laceration, rupture and haemoperitoneum following fall from a height.
Peripheral smear. a,b: Thrombocytosis and neutrophilia with presence of numerous giant platelets. (Leishman stain; 40x). c: Trophozoite of Plasmodium vivax (arrow) (Leishman stain;1000x). d: Mixed malaria- Trophozoite of Plasmodium vivax (arrow) and multiple ring forms of falciparum (arrow head). (Leishman stain; 1000x). e: Multiple ring forms of falciparum (arrow head). (Leishman stain; 1000x). f: Trophozoite of Plasmodium vivax (arrow) and a giant platelet (arrow head). (Leishman stain; 1000x)
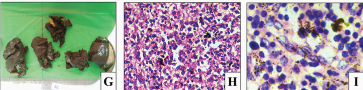
On persistent questioning, he gave a history of fever associated with chills and rigours before sustaining the trauma accounting for the vulnerability of enlarged spleen secondary to malaria, which underwent laceration. The surgical pathology section had received an enlarged spleen in multiple pieces having a slate grey appearance, characteristic of malarial infection [Table/Fig-1g]. Histological sections, on review, also revealed the parasites and malarial pigments in the red pulp [Table/Fig-1h,i]. Artesunate therapy (2.4 mg/kg BW IV) was initiated in the patient for mixed malaria along with routine Postoperative care.
g: Splenectomy specimen with multiple pieces of lacerated spleen having slate grey appearance. (H&E; 200x). h&i: Microscopy of spleen revealed congested red pulp with extensive malarial pigment. (H&E; 400x)
Discussion
Malaria is an endemic infection in 106 countries across the world as per World Health Organisation World Malaria Report 2011. Malaria is an infection well known to cause moderate splenomegaly in 70-80% of cases [1]. The assessment of splenomegaly is an epidemiological tool in the control of malaria where the proportion of palpable spleens in a given population is evaluated (spleen rate). Plasmodium vivax species is presumed to cause marked splenomegaly than the other species [1].
Thrombocytopaenia is a common feature of malaria and resolves 1-2 weeks after parasite clearance. Thrombocytosis is observed in the time period between thrombocytopaenia and resumption of normal platelet counts. Persistence of thrombocytosis is associated with focal complications like splenic infarction [2]. In our case, the mismatch of thrombocytosis and high parasitaemia prompted us to elicit the history which revealed that the patient underwent splenectomy 10 days ago. This explains the post-splenectomy reactive thrombocytosis [3].
In the present study, congestion and enlargement of the spleen due to malaria was the cause of traumatic laceration and rupture. Plasmodium falciparum species is known to cause complications like cerebral malaria, thrombocytopaenia and renal failure but splenic rupture is very uncommon. Cases of splenic rupture and infarction due to malaria have been reported in literature with an incidence of 2% in falciparum malaria [1,4–9]. Spontaneous rupture was excluded in the indexed case as there was a history of trivial trauma. In endemic areas, splenomegaly due to malaria can be a cause of splenic laceration and rupture following trivial to severe abdominal blunt trauma.
In a malaria endemic region, a blood smear examination is mandatory for diagnosis and management of patients. This case is unique because the malarial parasites were identified in a background of marked thrombocytosis, which is seldom associated with this infection. In our case, this is a post-splenectomy thrombocytosis, which has an incidence of 75-82% [3].
Conclusion
Plasmodium infection is an important unusual cause of splenic rupture in endemic areas and should be considered during the work up of such patients. This case, to the best of our understanding, is one of the rarest of its kind of untreated malaria with high parasitaemia causing splenic rupture with post-splenectomy reactive thrombocytosis.
[1]. Machado SA, Lopes MBM, Cardoso MG, Ferrer M, Castillo P, Spleen Rupture in a Case of Untreated Plasmodium vivax InfectionPLoS Negl Trop Dis 2012 6(12):e1934 [Google Scholar]
[2]. Kim A, Park YK, Lee JS, Chung MH, Kim ES, A case of symptomatic splenic infarction in vivax malariaKorean J Parasitol 2007 45(1):55-58. [Google Scholar]
[3]. Khan PM, Nair RJ, Olivares J, Tingle LE, Li Z, Postsplenectomy reactive thrombocytosisProc (Bayl Univ Med Cent) 2009 22(1):9-12. [Google Scholar]
[4]. Vidyashankar C, Basu A, Kulkarni AR, Choudhury RK, Spontaneous rupture of spleen in falciparum malariaIndian J Gastroenterol 2003 22:101e-2. [Google Scholar]
[5]. Kim KM, Bae BK, Lee SB, Spontaneous splenic rupture in Plasmodium vivax malariaAnnals of Surgical Treatment and Research 2014 87(1):44-46. [Google Scholar]
[6]. Fareed MI, Mahmoud AE, Spontaneous rupture of falciparum malarial spleen presenting as haemoperitoneum, haemothorax, and haemoarthrosisAm J Case Rep 2013 14:405-08. [Google Scholar]
[7]. Kapoor U, Chandra A, Kishore K, Spontaneous rupture of spleen with complicated falciparum malaria in a United Nations PeacekeeperMedical Journal Armed Forces India 2013 69:288-90. [Google Scholar]
[8]. Aggarwal HK, Nand N, Bharti K, Sen J, Chakrabarti D, Sonia Splenic infarct in malaria- an unusual etiologyJ Ind Acad Clin Med 2005 6(4):331-33. [Google Scholar]
[9]. Waweru P, Macleod J, Gikonyo A, Complicated malaria and a covert ruptured spleen: a case reportJ Sur Case Reports 2014 11doi:10.1093/jscr/rju122 [Google Scholar]