Traumatic Optic Neuropathy – A Conundrum
Vinoth Kanna Selvaraj1, Ramachandran Viswanathan2, Vasudevan Devanathan3
1 Assistant Professor, Department of Neurology, Saveetha Medical College Hospital, Saveetha University, Thandalam, Kancheepuram, Tamil Nadu, India.
2 Assistant Professor, Department of Neurology, Saveetha Medical College Hospital, Saveetha University, Thandalam, Kancheepuram, Tamil Nadu, India.
3 Head of Department and Professor, Department of Neurology, Saveetha Medical College Hospital, Saveetha University, Thandalam, Kancheepuram, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramachandran Viswanathan, RVR Foundation F6 Plot 3004, 5th Main Road, Ram Nagar South, Madipakkam, Chennai-600091, India.
E-mail: vrc@rvrfoundation.com
Visual impairment following head injury may be an enigma especially if the onset of symptoms were to be few days after the actual trauma and the bias arising out of the initial normal ophthalmological examination is not neutralised by unbiased repeated formal clinical evaluation aided with electrophysiology. We report and discuss here a 32-year-old lady with delayed onset of indirect traumatic visual loss with anaemia who failed to improve after blood transfusion but improved immediately following steroid therapy seven days after trauma. Though steroids have not been shown to have a significant contribution on outcomes following Traumatic optic neuropathy, this report rekindles its role in delayed progressive visual loss following head trauma and the need to re-analyse the role of steroids in patients with delayed progressive visual disturbance following head injury excluding those with acute onset symptoms in view of different pathologies in both these presentations. This paper also highlights potential mechanisms for the two major types of presentation.
Delayed visual loss, Erythropoietin, Iron deficiency anaemia, Steroid
Case Report
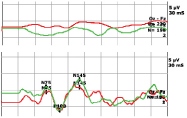
A 32-year-old lady presented to the emergency department with head injury following a fall from a bike. Following the fall, the patient was unconsciousness for around five minutes and had vomited twice. Eyewitness denied any seizures or ENT bleed. At the time of presentation around 3 hours after the event, the patient was conscious, oriented with normal vitals, neurological and ophthalmological findings. The patient however had multiple abrasions over the right foot and the back and two lacerated wounds over the left parietal and occipital regions. The lacerated wounds were sutured and the patient was admitted with the general surgeon for observation. A CT scan Brain revealed left parietal sub-galeal haematoma and left parietal sub centimetric calcification. Neurosurgeons recommended conservative management. Patient was noticed to have significant anaemia with Hb 4.5gm%, MCV 55; MCH 14 and MCHC 25 and a blood picture suggestive of an iron deficiency anaemia suspected due to a nutritional deficiency. The patient was therefore transfused packed cells on day 3 while concomitantly starting haematinics. On Day 4 the patient complained of hazy vision and visual impairment in the left eye. A formal bedside neurosurgical and ophthalmic consultation were re-obtained as also MRI brain and optic nerves. Patient could count fingers well at 3 meters with both eyes at this stage. Formal visual acuity testing was not performed. Haemoglobin at this juncture following packed cell transfusion raised levels to 5.8gm% and the patient continued haematinics. The visual complaints slowly progressed and on Day 6 the patient complained of absent vision in left eye. A formal neurological opinion was sought on day 7. Neurological examination then revealed a conscious, cooperative subject with a Relative Afferent Pupillary Defect (RAPD) in the left eye with ability to see well at 3m with the right eye. The vision on the left eye was restricted to perception of hand movements at 1 meter. Extra-ocular movements were normal and full. Visual Evoked Potential (VEP) revealed a left optic neuropathy with the left eye showing absence of occipital potentials [Table/Fig-1a]. In view of the deteriorating visual acuity with normal radiological findings in this patient with trauma and anaemia, high dose parenteral intravenous methyl-prednisolone (1 gm per day) was given for five days. The patient subjectively felt better from Day 8, within 24 hours of initiation of steroid therapy. VEP done on Day 11 was normal in both eyes [Table/Fig-1b] as also the visual acuity.
VEP Left eye a) done on Day 7 following trauma showing absent waves. b) The same eye show normal VEP on Day 11 following steroid therapy
Discussion
This patient presented with progressive delayed visual loss following a head injury that was initially considered psychogenic in nature. However VEP confirmed the organic nature of the problem. High dose steroid therapy given four days after onset of symptoms and seven days following head injury resulted in complete improvement of vision.
Traumatic Optic Neuopathy (TON) is an enigmatic [1] condition encountered in patients following head injury. The visual loss happens immediately after trauma in majority of patients where the diagnosis is straightforward. However, in a proportion of patients 10-22% with visual loss [2,3] and up to 62% [3] with visual disturbance without complete visual loss; the visual disturbance is insidious in onset. Any patient complaining of visual disturbance following even a trivial head injury (especially over superior temporal orbital rim) should be immediately investigated. VEP should be performed in cases of doubt or high clinical suspicion to document an optic nerve dysfunction. Normal cursory examination findings in the initial stages post head injury does not rule out a developing indirect traumatic optic neuropathy. Hence unbiased serial opthalmological examination including formal visual testing where possible (including RAPD); and VEP is mandatory to diagnose and manage TON early.
CT Scan is the investigation of choice to delineate the aetiology for optic nerve trauma [4]. Contrast MRI of the optic nerve may also pick up optic nerve oedema. The patho-physiology of immediate visual loss in TON is related to shearing of axons of the optic nerve. Such lesions are associated with a poor prognosis. Our patient did not show any significant lesion in the optic canal or in the optic nerve.
The patho-physiology of delayed optic nerve dysfunction is thought to be primarily related to compromised blood supply due to nerve sheath haematoma [5] or intrachiasmatic haemorrhage [6] or secondarily due to pressure effects, following a triggered inflammatory response causing oedema within the optic nerve [5]. The role of steroids as a neuro-protective agent is based on its ability to inhibit free radical induced peroxidation and its ability to decrease inflammation and oedema. The dose of steroids is still speculative ranging from low dose (<100 mgs) to high (500 to 2000 mgs) to mega dose (> 5400 mgs) of methyl predinisolone. The use of steroids in TON has been greatly influenced by National Acute Spinal Cord Injury Study (NASCIS) that concluded that mega dose steroids used within 8 hours of injury showed better neurological outcomes. This contrasted with higher mortality associated with mega dose steroids in Corticosteroid Randomisation After Significant Head injury study (CRASH) [7]. Also randomised double blind placebo controlled trial of 31 patients with high dose steroids did not show significant differences in outcomes [7]. Effectively, the current evidence does not support a role for steroids in TON [2,7].
Late onset irreversible visual decline in patients with optic neuropathies have been speculated to be due to age related axonal loss on an already depleted neurons [8]. This is an extreme reason for irreversible visual loss happening over a period of years. Vascular injury invariably results in irreversible nerve damage especially when the patient is acutely symptomatic. In studies on Multiple sclerosis, it is documented that inflammatory release of cytokines locally or systemically could itself induce transient conduction blocks in partially demyelinated nerves [9]. Intravenous methylprednisolone produces clinical effects by reducing the levels of inflammatory cytokines. Unilateral dysfunction in delayed onset TON therefore may be symptomatic after trauma related demyelination. Over time, in patients with untreated or non self-limited inflammation, the chemically mediated injury may ultimately result in an irreversible inflammatory destruction of axons. Steroids may therefore be useful in such patients [10]. The conflicting results of the usefulness of steroids in TON [7] may be due to a combined analysis of patients with non-reversible acute injury and those with potentially reversible injury seen amongst patients with delayed visual loss. Rajiniganth et al., document recovery of vision in patients with TON following steroid therapy who had preserved residual vision at presentation [3]. Five of these eight patients in their series developed a gradual visual loss following head injury. Thus, when the symptoms evolve the pathology too is evolving and hence appropriate steps taken early could potentially reverse the clinical state. One such step could be the use of steroids.
Another conundrum in this patient was the association of abnormal VEP with anaemia. VEP prolongation can happen due to multiple causes including anaemia [11], vitamin deficiency, trauma and demyelination. Correction of anaemia can potentially reverse VEP abnormalities over a period of weeks [11]. In our patient the acute visual deterioration started following trauma and after the blood transfusion. Moreover the acute visual deterioration continued over days and the clinical improvement happened within 24 hours of steroid therapy even before the haematocrit could rise significantly. It is speculated that erythropoietin that is known to increase more than 1000 times in patients with anaemia [12] could have assisted recovery in this patient. The cause-effect relationship only favours steroids in clinical improvement.
Conclusion
Thus this case report highlights the potential role of steroids in management of patients with progressive delayed onset visual disturbance following head trauma. All such patients should be counselled to ensure informed consent for a trial with steroids.
[1]. Eidlitz-Markus T, Shuper A, Schwartz M, Mimouni M, Delayed post-traumatic visual loss: a clinical dilemmaPediatr Neurol [Internet] 2000 Feb [cited 2015 Aug 23] 22(2):133-35.Available from: http://www.ncbi.nlm.nih.gov/pubmed/10738919 [Google Scholar]
[2]. Levin LA, Beck RW, Joseph MP, Seiff S, Kraker R, The treatment of traumatic optic neuropathy: the International Optic Nerve Trauma StudyOphthalmology 1999 106(7):1268-77. [Google Scholar]
[3]. Rajiniganth MG, Gupta AK, Gupta A, Bapuraj JR, Traumatic Optic NeuropathyArch Otolaryngol Head Neck Surg 2003 129:1203-06. [Google Scholar]
[4]. Peyster RG, Hoover ED, Hershey BL, Haskin ME, High-resolution CT of lesions of the optic nerveAm J Neuroradiol [Internet] 1983 May [cited 2015 Aug 23] 4(2):169-74.Available from: http://www.ncbi.nlm.nih.gov/pubmed/6601426 [Google Scholar]
[5]. Crompton M, Visual lesions in closed head injuryBrain 1970 93:785-92. [Google Scholar]
[6]. Crowe NW, Nickles TP TBEA, Intrachiasmal hemorrhage: a cause of delayed post-traumatic blindnessNeurology 1989 39:863-65. [Google Scholar]
[7]. Yu-Wai-Man P, Griffiths PG, Steroids for traumatic optic neuropathy (Review)Cochrane database Syst Rev 2013 (6):1-21. [Google Scholar]
[8]. Simmons JKJR, Delayed Visual Decline in Patients With “Stable” Optic NeuropathyArch Ophthalmol 2005 123(June 2005):785-88. [Google Scholar]
[9]. Moreau T, Coles A, Wing M, Isaacs J, Hale G, Waldmann H, Transient increase in symptoms associated with cytokine release in patients with multiple sclerosisBrain 1996 119(Pt 1):225-37. [Google Scholar]
[10]. Stonecipher KG, Conway MD, Karcioglu ZA, Haik BG, Haematoma of the optic nerve sheath after penetrating traumaSouth Med J [Internet] 1990[cited 2015 Aug 23] 83(10):1230-31.Available from: http://www.ncbi.nlm.nih.gov/pubmed/2218669 [Google Scholar]
[11]. Sarici SU, Okutan V, Dündaröz MR, Serdar AM, Akin R, Deda G, The effect of iron supplementation on visual-evoked potentials in infants with iron-deficiency anaemiaJ Trop Pediatr [Internet] 2001 [cited 2015 Aug 19] 47(3):132-35.Available from: http://www.ncbi.nlm.nih.gov/pubmed/11419674 [Google Scholar]
[12]. Cazzola M, Mercuriali F, Brugnara C, Use of recombinant human erythropoietin outside the setting of uremiaBlood [Internet] 1997 [cited 2015 Aug 27] 89(12):4248-67.Available from: http://www.ncbi.nlm.nih.gov/pubmed/9192747 [Google Scholar]