Minimally Invasive Plate Osteosynthesis with Locking Plates for Distal Tibia Fractures
Ajeet Dhakar1, Rajendra Annappa2, Mahesh Gupta3, Hemeshwar Harshwardhan4, Prem Kotian5, Pooja K. Suresh6
1 Consultant, Department of Orthopaedics, JLN Medical College, Ajmer, Rajasthan, India.
2 Assistant Professor, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
3 Ex Professor and Head, Department of Orthopaedics, JLN Medical College, Ajmer, India.
4 Associate Professor, Department of Orthopaedics, JLN Medical College, Ajmer, Rajasthan, India.
5 Professor, Department of Orthopaedics, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
6 Assistant Professor, Department of Pathology, Kasturba Medical College, Mangalore, Manipal University, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rajendra Annappa, Assistant Professor, Department of Orthopaedics, Kasturba Medical College, Mangalore-575001, Manipal University Karnataka, India.
E-mail: rajendra.orthopaedics@gmail.com
Introduction
Distal tibia fractures are challenging injuries with multiple fixation options. Minimal invasive plating for distal tibia fracture is becoming more popular with documented good outcomes.
Aim
To evaluate the functional and radiological results of fixation of distal tibia fractures with locking plates with Minimally Invasive Plate Osteosynthesis (MIPO) technique.
Materials and Methods
Fifty fractures of distal tibia without Intra-articular extension were operated with locking compression plating with MIPO technique. They were followed up at regular intervals. Functional and radiological results were evaluated at the end on one year.
Results
The fractures united in 48 (96%) patients with 2 (4%) cases of delayed union which took 30 weeks of time. Postoperatively, 2 patients developed superficial skin infection, 2 patients developed deep infection and 3 patients developed ankle stiffness due to loss of postoperative protocol and 4 patients had implant failure in form of screw breakage. Good amount of range of mobility of ankle joint was present in almost all patients.
Conclusion
MIPO with locking plates for distal tibia fractures is associated with good functional outcomes and is an effective treatment for distal tibia fractures. Although, a larger sample of patients and longer follow up are required to fully evaluate this method of treatment, we strongly encourage its consideration in the treatment of such complex fractures.
Biological fixation, Distal tibia locking plates, MIPO for extraarticular fractures
Introduction
Distal tibia fractures are challenging injuries. They are primarily located within a square based on the width of the distal tibia without intra-articular extension. They are often caused by high energy axial compressive, direct bending or low energy rotation forces. These fractures constitute less than 7% of all the tibial fracture and less than 10% of all lower extremity fractures. The aim of treating the fracture is to preserve normal mechanical axis, ensure joint stability and restore a near full range of motion. This is a difficult task to accomplish in each and every case as we face compromised soft tissue condition, variable bone quality and associated medical conditions [1,2].
Conservative management can be done in selected cases whenever fractures are stable with minimal shortening. High rate of complications like malunion, limb length discrepancy, decreased range of motion and early osteoarthritis of the ankle have been reported following conservative treatment of these fractures [3–5].
Surgical fixation is considered for most distal tibia fractures which require meticulous preoperative planning. Available options for stabilizing fractures are external fixators, interlocking nails and locking plates. The factors determining the fixation methods are pattern of fracture, quality of bone and condition of soft tissues [5–8].
Ruedi TP et al., advocated open reduction and internal fixation with plate as the standard method of treatment of distal tibia fractures [3]. Results of conventional osteosynthesis with plates have been suboptimal with reported complications of wound infection, skin breakdown and delayed union or non-union, requiring secondary surgical intervention. Locking compression plating has gained popularity and is being used frequently for fixation of distal tibia fractures. With the use of minimal invasive techniques excellent results are obtained in complex fractures. Many studies are available in literature where encouraging results are reported. Locking compression plating is technically feasible and creates a stable, fixed angle device when locking screw heads lock itself with the plate. Locking plates provide excellent stability compared to a conventional plate and better protection against loss of reduction and minimization of bone contact. Preservation of vascularity of fracture fragments, fracture haematoma and minimal soft tissue damage favour minimally invasive percutaneous plating for distal tibia fractures [6–11].
This study was planned to assess the union rate, deformity, leg length discrepancy, gait and ankle range of motion, return to previous daily and sports activities, and infections and other complications associated with distal tibial plates.
Materials and Methods
Fifty patients with distal tibia fractures treated with locked compression plating were included in the study. This was a prospective study done in a tertiary care centre from June 2010 to December 2014. All patients with age >18 years, closed fractures without intra-articular extension and Gustillo type 1 fractures were included. Intra-articular fractures, tibial shaft fractures, elderly patients with co-morbid condition, non-weight bearing limb, pathological fractures and Gustillo type II open fractures were excluded. AO/OTA classification system was used to classify fractures [1]. Institutional ethics committee clearance was taken for study. Informed consent was obtained from all patients before surgical procedure and for participation in the study.
Operative Technique
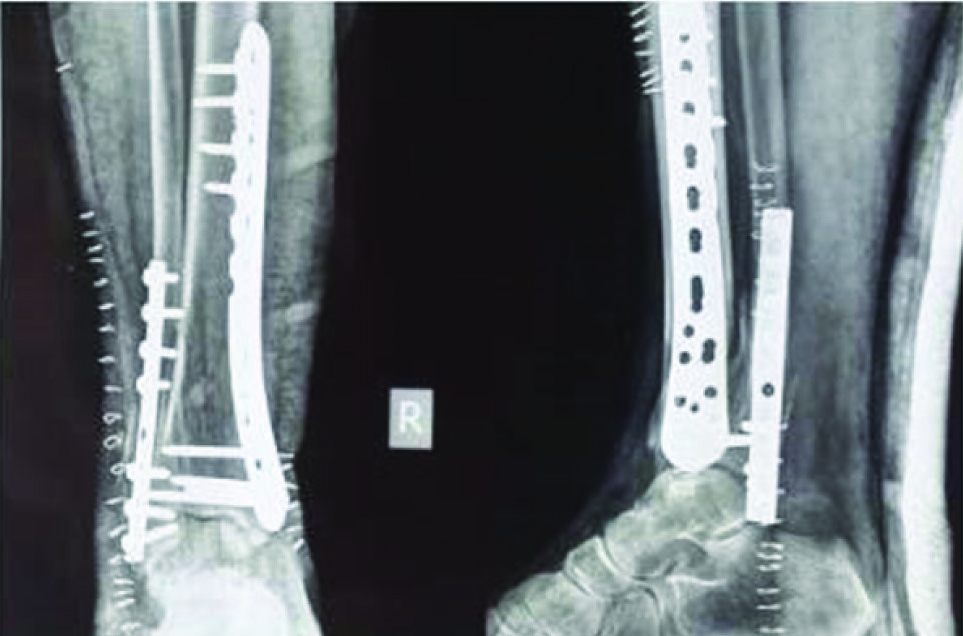
Complete preoperative radiographic assessment was done and preoperative plan was prepared. Broad spectrum intravenous antibiotics were given immediate preoperatively. The patient was positioned supine on a radiolucent operating table under spinal or epidural anaesthesia. Locking Plate Osteosynthesis is done with the MIPO technique. Incision is made over the medial malleolus measuring about 3cms with a gentle curve, sparing the saphenous vein and nerve. Extraperiosteally a tunnel is made by blunt dissection in right orientation. Anatomical distal tibial locking plate is passed through this tunnel by retrograde technique. Locking sleeves can be attached to plate and used to hold the plate at distal end while insertion. Plate is passed in such a way that end of plate is visualized adequately and screws can be inserted distally. Using C arm plate is adjusted to meet the contour of the bone. Fracture reduction is achieved under image intensifier by assessing length, axial and rotational alignment. Plates can be held temporarily by K wires whenever required. Varus-valgus angulation of <50, anterior posterior angulation <100, and shortening of <15mm were considered acceptable reduction. Sagging of distal fragment at fracture site-can be prevented by elevating fracture site with a bolster and plantar flexion of foot [Table/Fig-1]. A locking cortical or cancellous screw is inserted. Fracture reduction is confirmed and cortical screw is inserted into proximal diaphyseal fragment which helps plate to contact with plate surface [8]. Remaining screws are inserted by stab incisions. Associated fibula fractures when present at syndesmotic level was fixed with plates or Rush nail depending on fracture type. Wound was irrigated with saline and closure done in layers. Sterile dressing was done and well padded posterior splint was given with ankle in neutral position [12–15].
Sagging at the fracture site
Postoperative Management
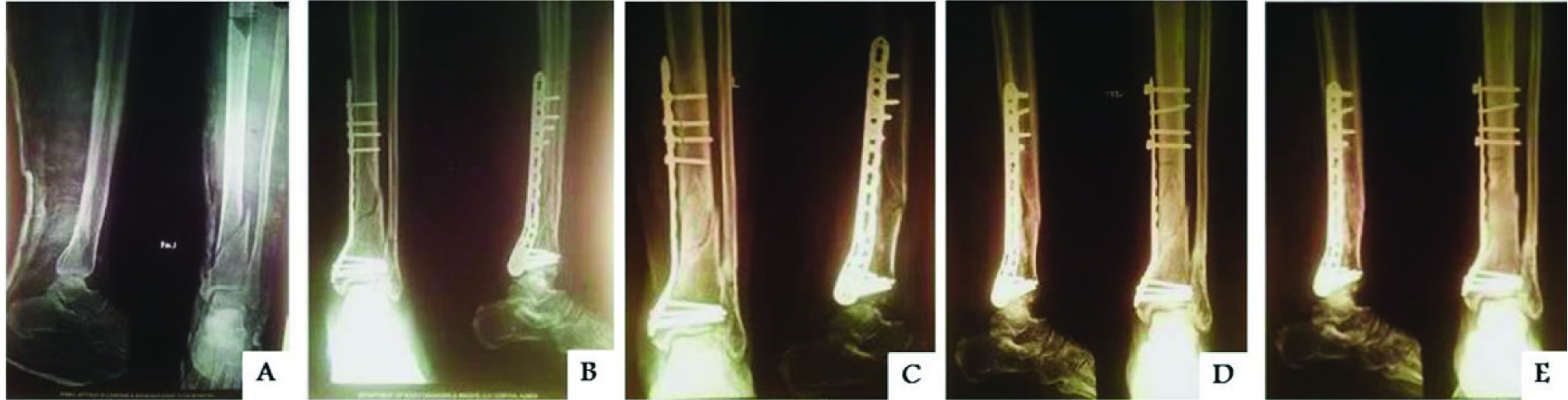
Static quadriceps exercises & toe movements, as tolerated were begun from 1st postoperative day. Ankle mobilization was started from 3rd postoperative day. Intra-venous antibiotics were given for 3 days followed by a course of oral antibiotics for 5 days. Analgesics were given as per need. Suture removal was done on 10th Postoperative day. Protected weight bearing was allowed only once signs of progress toward union were evident, usually at 6 weeks postoperatively. Full weight bearing was allowed after 10 to 12 weeks, depending on the radiographic signs of fracture healing. X-rays would be taken at regular intervals and evaluated for fracture healing, alignment at fracture site & look for any evidence of mal-alignment. Clinically union was defined as painless fracture site during full weight bearing. Radiographically fracture was considered united if 3 of 4 cortices in 2 radiographic views were continuous. Patients were followed up for a period of 1 year at 6 weeks, 12 weeks, 3 months, 6 months and 1 year [Table/Fig-2]. At the final follow up patients were evaluated using American Orthopaedic Foot and Ankle Society (AOFAS) score [16].
(a) Fracture of distal tibia; (b) Plate osteosynthesis with MIPO technique; (c) Uncomplicated union.

Results
In this study, 50 fractures of distal fourth fractures of tibia in adults were surgically managed by reduction and internal fixation with minimally invasive plate osteosynthesis (MIPO). The age of the patients in this study, ranged from 22 years to 62 years average being 41 years. There were 34 male and 16 female patients, 26 patients had fracture of left and 24 patients had fracture of right tibia. Forty three fractures were closed and 7 were open fractures. Road traffic accident (high energy trauma) was etiological factor in 33, 17 cases sustained fractures following fall (low energy trauma). Head injury was present in 5 cases, chest injury in 2 and radius fracture in 1 case. There were 33 cases of associated fibular fractures. Injury surgery interval was less than 8 hours in 14 cases, < 3 days for 20 cases, 3-7 days for 14 cases and more than 7 days in 2 cases. Average surgery time was 49mins, 13 cases took 31-40 minutes, 17 (35%) took 41-50 minutes, 12 (24%) took 51-60 minutes, 8 cases took 61-70 minutes. Average union time was 20.96 weeks. The fractures united in 48 (96%) patients with 2 (4%) case of delayed union which took 30 weeks of time period for the radiological signs of callus formation Postoperative complications are mentioned in [Table/Fig-3]. Plate removal was done in 5 cases; screw exchange was done in 3 cases [Table/Fig-4]. Good amount range of mobility of ankle joint was present in almost all patients. Based on AOFAS scores excellent results were obtained in 33, good in 14 and fair in 3 cases. The limitations of our study were small sample of patients and shorter follow-up.
| Complications | No. of Patients | Percentage (%) |
|---|
| Superficial skin infection | 2 | 4 |
| Deep Infection | 2 | 4 |
| Ankle movement restriction>75%50-75%25-50%<25% | 0021 | 0042 |
| Varus angulation | 2 | 4 |
| Implant Failure | 4 | 8 |
(a)Fracture of distal tibia-Preoperative; (b)Postoperative radiograph; (c) Implant failure-Multiple screw breakage; (d) Screw breakage managed with replacement with new screws; (e) Union.
Discussion
Distal diametaphyseal tibia fractures are one of the most problematic injuries to manage. Results of operative treatment are dependent on the severity of the initial injury, the quality and stability of the reduction. The mechanism of injury, status of soft tissues, the degree of comminution and articular damage affect the long term clinical outcome. A variety of treatment options are available. But there is no consensus on the best treatment modality [1–3]. Options for surgical fixation include external fixation, intramedullary nailing and plate fixation. External fixators are used in open fractures with soft tissue injury where nail or plate fixation is contraindicated. Many complications are reported when external fixators are used for definitive management of distal tibia fractures. Review of literature report high rate of malunion (5-25%), nonunion (2-17%), loss of reduction and pin tract infection (10-100%) which makes it less preferred technique [3–5].
Many authors have advocated intramedullary fixation with interlocking nails in distal tibia fractures with good outcomes. Intramedullary nailing has advantages of closed stabilization with preservation of fracture haematoma and no damage to overlying soft tissues [10]. However, due to the widening of medullary canal at metaphysis, angular and rotational stability is not achieved. Inadequate reduction, intraoperative loss of reduction after nail insertion, implant failure and malunion are reported complications [13,17]. Guo JJ et al., in their study concluded nailing to be better option for treating distal tibial fractures with atleast 3cm distal fragment and no articular incongruity. They found no difference in union rate but mean radiation time and operating time were significantly longer in LCP group and no statistical difference was noted in alignment [15,18,19].
Open reduction and internal fixation leads to increased risk of infection and nonunion [6,7]. Minimally invasive plating techniques reduce iatrogenic soft tissue trauma and damage to vascularity of bone fragments, as well as preserve the fracture haematoma resulting in uncomplicated union. Anatomical reduction of fractures should be done under image intensifier before fixation. Different methods for fracture reduction include calcaneal traction, external fixators or distractors, reduction clamps and interfragmentary screws through stab incision [3–5]. Fibula fractures when present also affect fracture reduction. We preferred fixation of fibular fractures before tibia for better alignment. No clear guidelines exist in literature for fibular fixation but when syndesmosis is involved it should be fixed [13,18–20].
Distal tibia fractures are associated with gross swelling, skin injury and blisters because of subcutaneous location. Skin condition determines the timing of surgery. Wound dehiscence and infection are complications when surgery is done with poor soft tissue conditions. Immobilization by splinting, icepacks and delaying surgery help in limiting further soft tissue injury and better preoperative soft tissue condition. Surgery was done when the swelling subsided, and the wrinkle sign was seen. Dorsiflexion of the ankle is done while observing the anterior aspect of the ankle for skin creases; the absence of a skin crease or wrinkle suggests severe swelling [17,20]. In our study 8 cases were operated after 3 days due to poor skin condition. There was no difference in union rates and complications in those who were operated before 3 days or after. Wound dehiscence and infection are of concerns when operated with locking plates. Guo JJ et al., reported more wound complications in LCP group (14.6%) compared to nailing group (6.8%) [15]. Lau et al., reported late infection rate of 15% in fixation with locking plates [19]. Average rate of infection in various literature available was 5-15%. In our study infection was seen in 5 cases (10%). Delaying surgery if limb is swollen and bruised, gentle soft tissue handling and reducing operative time helps in reducing infection rates [13–15,18,19].
Malunion is an uncommon complication after LCP. Rate of malunion in literature varies from 0-5%. Delayed union and nonunion has been reported to be 5-16% in various studies. Collinge et al., reported a reoperation rate of 5% which included secondary procedure like bone grafting for delayed union [11]. Rate of secondary procedures for delayed union or non union or change of hardware has been reported 3.8% to as high as up to 35%. Implant failure has been reported to be 2-6%. Plate bending or breakage is often associated with malalignment, delayed or nonunion [15,18,19].
Pain over medial malleolus, hardware prominence and pain due to impingement of the implant on the skin was common. Gao et al., suggested polyaxial locking plates to gain adequate fixation and to achieve a perfect match between the plate and the distal part of the tibia [12], which in turn may further reduce tension in the soft tissue [13,19].
The great saphenous vein and nerve injury can occur rarely. Careful identification during surgery and adequate drill sleeve placement usually suffice. We did not have any case of saphenous nerve or vein injury. Removal of LCP can be difficult and includes all general risks associated with surgical procedures. Complication rates of 20% have been reported. Stripping of screw head or threads occurs frequently. Screw extraction devices cannot be engaged to remove locking screws which makes the procedure cumbersome [12–15,19].
Conclusion
Effective stabilization of distal tibia fractures can be achieved by distal tibia locking plating through MIPO technique which not only helps in achieving reduction in difficult situations, but also in rapid union, because it facilitates preservation of the blood supply to the fragment and anatomical reduction of the fracture. It is a simple, rapid and straight forward procedure which has good results.
[1]. Barie DP, Pilon fractures. In: Bucholz RW, Court-Brown CM, Heckman JD, Tornetta PRockwood and Green’s Fractures in Adults 2010 7th editionPhiladelphiaLippincott Williams and Wilkins:1928-74. [Google Scholar]
[2]. Sarmiento A, Latta LL, 450 closed fractures of the distal third of the tibia treated with a functional braceClin Orthop Relat Res 2004 428:261-71. [Google Scholar]
[3]. Ruedi TP, Allgower M, The operative treatment of intra articular fractures of the lower end of tibiaClin Orthop 1979 138:105-10. [Google Scholar]
[4]. Court-Brown CM, Walker C, Garg A, McQueen MM, Half-ring external fixation in the management of tibial plafond fracturesJ Orthop Trauma 1999 13:200-06. [Google Scholar]
[5]. Bedi A, Le TT, Karunakar MA, Surgical treatment of nonarticular distal tibia fracturesJ Am Acad Orthop Surg 2006 14:406-16. [Google Scholar]
[6]. Maffuli N, Toms A, McMurtie A, Oliva F, Percutaneous plating of distal tibia fracturesInt Orthop 2004 28:159-62. [Google Scholar]
[7]. Redfern DJ, Syed SU, Davies SJM, Fractures of the distal tibia: minimal invasive plate osteosynthesisInjury 2004 35:615-20. [Google Scholar]
[8]. Hazarika S, Chakravarthy J, Cooper J, Minimally invasive locking plate osteosynthesis for fractures of the distal tibia –Injury 2006 37(9):877-87. [Google Scholar]
[9]. Hasenboehler E, Rikli D, Babst R, Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patientsInjury 2007 38:365-70. [Google Scholar]
[10]. Vallier HA, Le TT, Bedi A, Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailingJ Orthop Trauma 2008 22(5):307-11. [Google Scholar]
[11]. Collinge C, Kuper M, Larson K, Protzman R, Minimally Invasive Plating of High-Energy Metaphyseal Distal Tibial FracturesJ Orthop Trauma 2007 21:355-61. [Google Scholar]
[12]. Gao H, Zhang CQ, Luo CF, Zhou ZB, Zeng BF, Fractures of the distal tibia treated with polyaxial locking platingClin Orthop Relat Res 2009 467(3):831-37. [Google Scholar]
[13]. Shrestha D, Acharya BM, Shrestha PM, Minimally invasive plate osteosynthesis with locking compression plate for distal diametaphyseal tibia fractureKathmandu Univ Med J 2011 34(2):62-68. [Google Scholar]
[14]. Paluvadi SV, Lal H, Mittal D, Vidyarthi K, Management of fractures of the distal third tibia by minimally invasive plate osteosynthesis – A prospective series of 50 patientsJ Clin Orthop Trauma 2014 5(3):129-36. [Google Scholar]
[15]. Guo JJ, Tang N, Yang HL, Tang TS, A prospective, randomized trial comparing closed inramedullary nailing with percutaneous plating in the treatment of distal metaphyseal fractures of the tibiaJ Bone Joint Surg Br 2010 92(7):984-88. [Google Scholar]
[16]. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M, Clinical rating system for the ankle, hindfoot, midfoot, hallux and lesser toesFoot Ankle Int 1994 15:349-53. [Google Scholar]
[17]. Fan CY, Chiang CC, Chuang TY, Chiu FY, Chen TH, Interlocking nails for displaced metaphyseal fractures of the distal tibiaInjury 2005 36:669-74. [Google Scholar]
[18]. Ronga M, Longo UG, Maffulli N, Minimally invasive locked plating of distal tibia fractures is safe and effectiveClin Orthop Relat Res 2010 468:975-82. [Google Scholar]
[19]. Lau TW, Leung F, Chan CF, Chow SP, Wound complication of minimally invasive plate osteosynthesis in distal tibia fracturesInt Orthop 2008 32(5):697-703. [Google Scholar]
[20]. Tull F, Borrelli J, Soft-tissue injury associated with closed fractures: evaluation and managementJ Am Acad Orthop Surg 2003 11:431-38. [Google Scholar]