Thyroid Gland Involvement in Carcinoma Larynx and Hypopharynx-Predictive Factors and Prognostic Significance
Elizabeth Mathew Iype1, Vijay Jagad2, Santhosh Kumar Nochikattil3, Bipin T. Varghese4, Paul Sebastian5
1 Additional Professor, Department of Surgical Oncology, Regional Cancer Centre, Trivandrum, Kerala, India.
2 MCh trainee, Department of Surgical Oncology, Regional Cancer Centre, Trivandrum, Kerala, India.
3 Fellow in Head and Neck Surgical Oncology, Department of Surgical Oncology, Regional Cancer Centre, Trivandrum, Kerala, India.
4 Additional Professor, Department of Surgical Oncology, Regional Cancer Centre, Trivandrum, Kerala, India.
5 Director, Regional Cancer Centre, Trivandrum, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Santhosh Kumar Nochikattil, Fellow in Head and Neck Surgical Oncology, Department of Surgical Oncology, Regional Cancer Centre, Trivandrum, Kerala- 695011, India.
E-mail: dr.santhosh82@gmail.com
Introduction
Intraoperative management of thyroid gland in laryngeal and hypopharyngeal cancer is controversial.
Aim
The objectives of this study were to determine the incidence of thyroid gland invasion in patients undergoing surgery for laryngeal or hypopharyngeal carcinoma, to assess predictive factors and to assess the prognosis in patients with and without thyroid gland invasion.
Materials and Methods
One hundred and thirty-three patients who underwent surgery for carcinoma larynx and hypopharynx from 2006 to 2010 were reviewed retrospectively. Surgical specimens were examined to determine the incidence of thyroid gland invasion and predictive factors were analysed. The recurrence rate and the survival in patients with and without thyroid gland invasion were also analysed.
Results
Out of the 133 patients with carcinoma larynx and hypopharynx who underwent surgery, histological thyroid gland invasion was observed in 28/133 (21%) patients. Significant relationship was found between histological thyroid gland invasion and preoperative evidence of thyroid cartilage erosion by CT scan and also when gross thyroid gland involvement observed during surgery. There is significant association between thyroid gland invasion when there is upper oesophageal or subglottic involvement.
Conclusion
After analysing the retrospective data from our study, we would like to suggest that thyroid gland need not be removed routinely in all laryngectomies, unless there is advanced disease with thyroid cartilage erosion and gross thyroid gland involvement or disease with significant subglottic or oesophageal involvement.
Carcinoma, Infiltration, Thyroidectomy
Introduction
Intraoperative management of thyroid gland in laryngeal and hypopharyngeal cancer is controversial. The incidence of thyroid gland involvement in laryngopharyngeal cancer ranges from 0 to 23% [1,2]. Thyroidectomy in conjunction with a total laryngectomy or laryngopharyngectomy often results in hypothyroidism requiring life-long thyroid hormone replacement. Hemithyroidectomy causes hypothyroidism in 63% of patients, and if combined with radiotherapy, the incidence goes upto 89% of patients [1]. Ipsilateral hemithyroidectomy and isthmusectomy are routinely performed with total laryngectomy in many clinics. But there is no uniform consensus about the need for thyroid surgery in laryngopharyngeal surgery for cancer.
Aim
The aim of this study was to determine the incidence of thyroid gland invasion in patients undergoing surgery for laryngeal or hypopharyngeal carcinoma, to assess predictive factors and to assess the prognosis in patients with and without thyroid gland invasion.
Materials and Methods
This is a retrospective analysis of patients with laryngeal and hypopharyngeal cancer who underwent surgery in the Surgical Oncology Department in Regional Cancer Centre Trivandrum, India. One hundred and thirty-three patients who underwent surgery for carcinoma larynx and hypopharynx from 2006 to 2010 were reviewed. Thyroidectomy either in the form of hemi or total thyroidectomy was performed in T3 and T4 disease or disease with subglottic extension. The histopathological reports were re-analysed to determine the incidence of thyroid gland invasion. The site and extent of disease, the clinical stage and the histological findings were analysed to find out the predictive factors for thyroid gland invasion. The recurrence rate and the survival in patients with and without thyroid gland invasion were also analysed.
Results
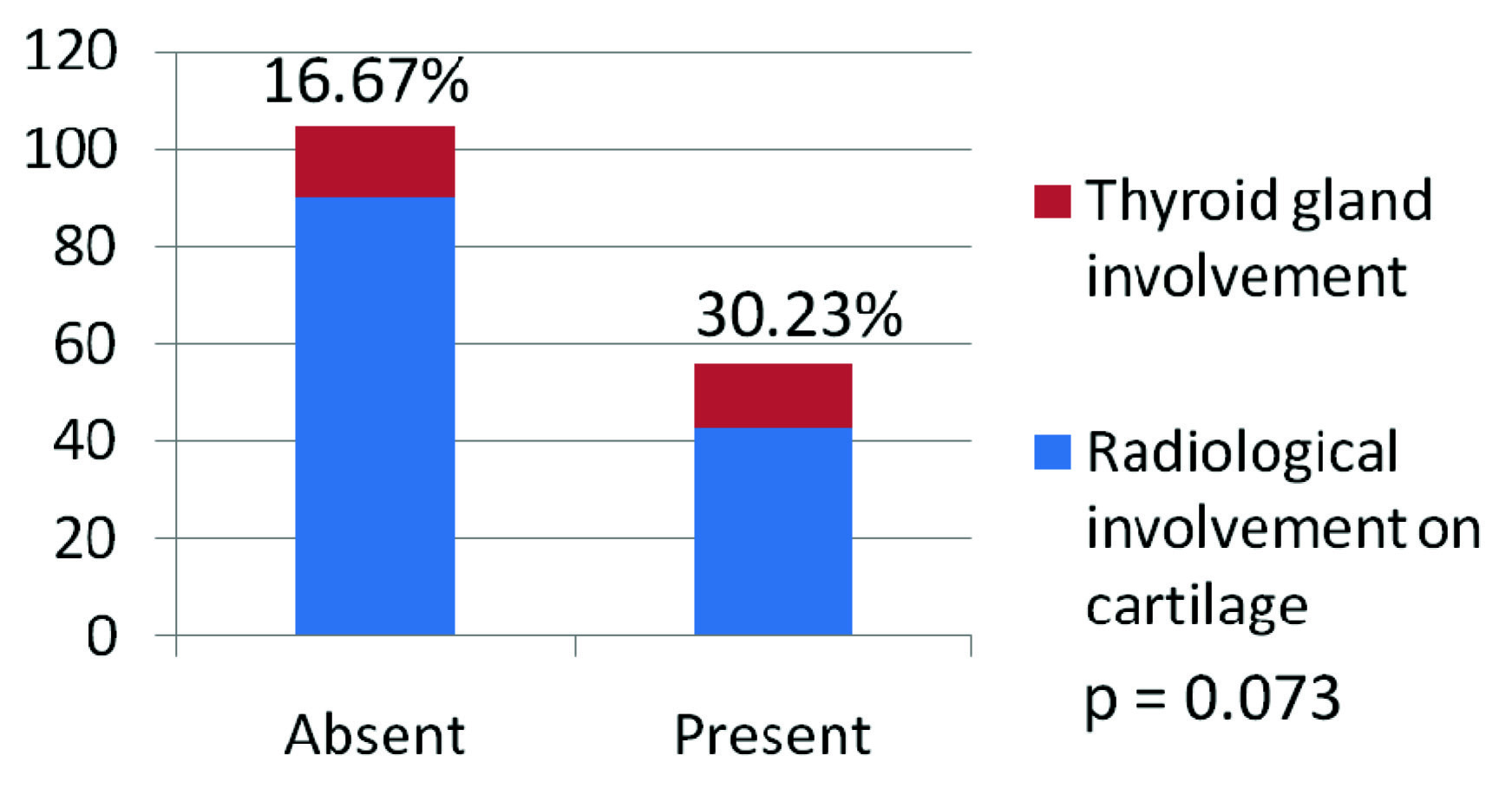
Out of the 133 patients with carcinoma larynx and hypopharynx who underwent surgery, 83 (62%) were primary surgery and 50 (38%) were salvage surgery after radiation failure. Excision of thyroid gland either as total or hemithyroidectomy along with the laryngeal surgery was done for 89(67%) patients. Histological evidence of thyroid gland invasion was observed in 28/133 (21%) patients. Significant relationship was found between histological thyroid gland invasion and preoperative finding of thyroid cartilage erosion by CT scan 13/43(30%) patients with cartilage erosion were having thyroid gland invasion compared to 15/90 (16.67%) without cartilage erosion. p= 0.07 [Table/Fig-1].
Showing correlation between radiological involvement of thyroid cartilage and histological thyroid gland involvement.
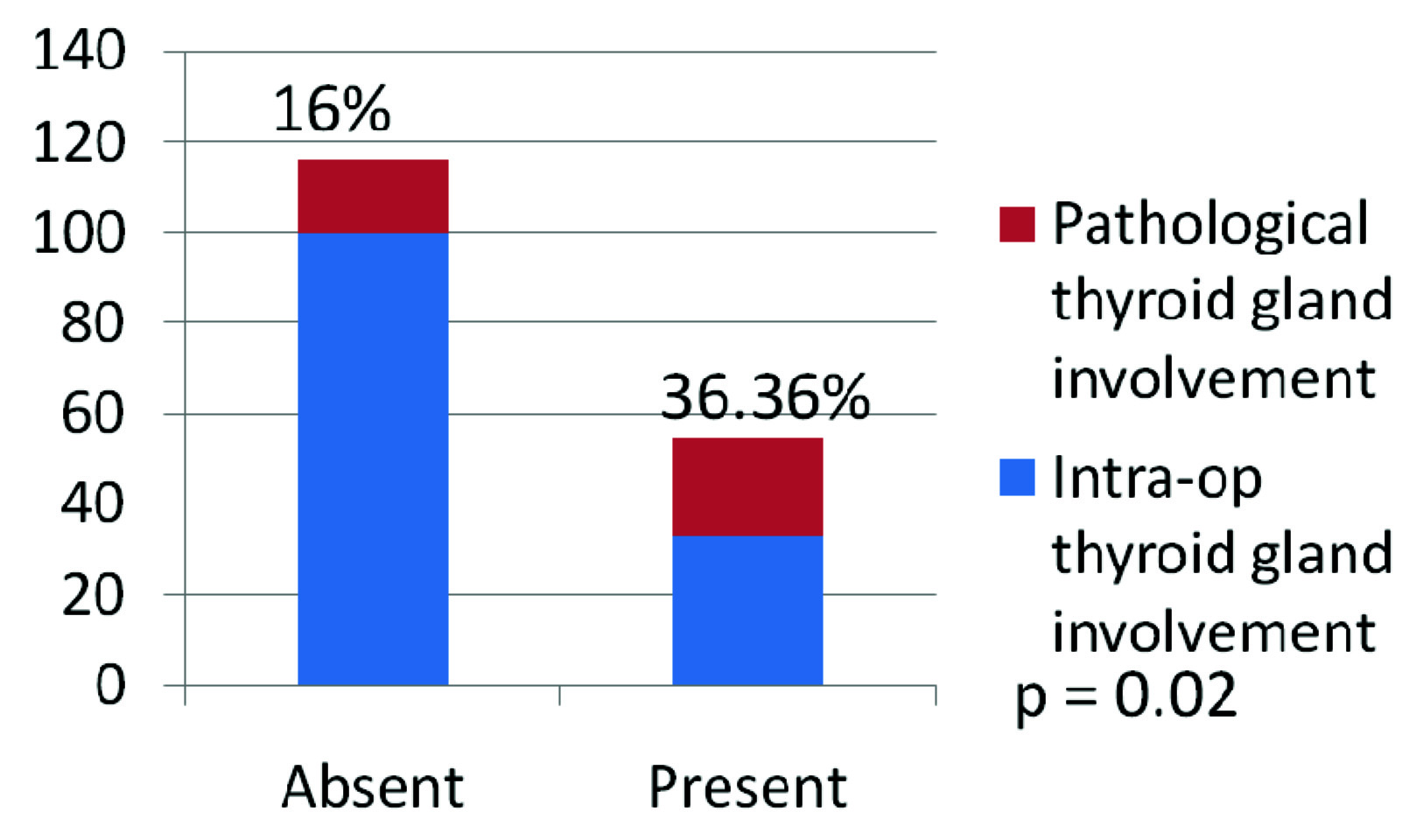
Histological thyroid gland invasion was significant when gross thyroid gland involvement observed during surgery 12/33 (36%) compared to 16/100 (16%) patients without gross glandular invasion was not there (p-value=0.02) [Table/Fig-2].
Showing correlation intra-op thyroid gland involvement and pathological thyroid gland involvement.
There is also significant pathological gland invasion in advanced clinical T stages (stage III and stage IV) of the disease 26/108 (24%) compared to 2/25 (8%) in early stage disease (Stages I and II). There is also significant association between thyroid gland invasions when there is upper oesophageal involvement 5/5 (100%). There was increased proportion of thyroid gland involvement when the growth was involving the subglottis (28.57%) and glottis (22.37%) [Table/Fig-3].
Showing percentage of thyroid gland involvement in accordance to sub-site.
| Site of tumour | No of cases | Thyroid gland involvement | Percentage | p-value |
|---|
| Supraglottic | 18 | 3 | 16.67% | 0.811 |
| Glottic | 76 | 17 | 22.37% | 0.783 |
| Subglottic | 7 | 2 | 28.57% | 0.616 |
| Pyriformfossa tumour | 31 | 6 | 19.35% | 1 |
| Postcricoid region | 1 | 0 | 0 | |
But there was no significant association with age, gender, nodal stage subglottic involvement or degree of differentiation of the tumour. In addition, no significant relationship was found between the presence of thyroid gland invasion and recurrent disease after radiotherapy. There was no significant difference in the disease free survival between patients with or without thyroid gland invasion.
Discussion
Tumours of larynx and hypopharyx can involve the thyroid gland by direct infiltration which is the major route or by lymphatic embolisation [3]. Hematogenous metastasis to the thyroid gland is rare. Hence, it is possible to predict the involvement of thyroid gland pre-operatively in cases of carcinoma larynx and hypopharynx if the factors were known to the treating surgeon. This will avoid unnecessary thyroid surgeries and thereafter the sequel following it.
Risk of hypothyroidism is greatest laryngeal cancer among all the non thyroid head and neck cancer. In a prospective study by Sinard RJ et al., overall risk of hypothyroidism after treatment of head and neck malignancy was 15% and among them the group undergoing total laryngectomy (with thyroid lobectomy) and radiotherapy had 61% [4]. Also, the risk of hypothyroidism increases with succeeding years. In a study by Chung-Wai Ho reported that overall rate of hypothyroidism after treatment for laryngeal carcinoma was 44%. During follow up 19.9% were hypothyroid at 3 years, 38.6% at six years and at ten years of followup 93.3% were rendered hypothyroid. This mandates monitoring of hypothyroidism life long for all patients who have undergone treatment for advanced laryngo-pharyngeal malignanacy [5].
Thyroid gland involvement was seen in 28.57% cases of subglottic carcinoma and 22.37% of carcinoma glottis. There were no statistically significant difference between different subsites of carcinoma larynx and hypopharynx and the involvement of thyroid cartilage.
It has been shown that preoperative assessment of vocal cord mobility and extent of subglottic extension are significant correlates of thyroid gland invasion by carcinoma of the glottis. Distinct patterns of laryngeal spread are associated with thyroid gland invasion. Prophylactic hemithyroidectomy with isthmusectomy is indicated for glottis carcinoma in the preoperative setting of a fixed vocal cord and subglottic extension greater than 15 mm [3]. Sparano et al., and Gurunathal et al., recommended that hemithyroidectomy and isthmusectomy during total laryngectomy only in cases with subglottic extensions more than 1 cm or thyroid cartilage invasion with tumour [3,6]. In this study though the majority of percentage of thyroid gland involvement was seen with the sublottic site of the tumour this did not reached statistical significance probably due to less number of cases seven out of 133. The best laryngeal cancer thyroid tumour invasion predictor is the evidence of extralaryngeal extension [7]. Total thyroidectomy with bilateral paratracheal and pretracheal lymph node dissection is indicated when squamous cell carcinoma of the larynx involves the thyroid gland. Prophylactic ipsilateral thyroid lobectomy and isthmusectomy is warranted for large laryngeal cancers (T3, T4) that involve the anterior commissure, the subglottic area, or extend transglottically [8–12]. Transcartilagenous spread of tumour is also a predictor thyroid gland involvement which necessitates thyroid surgery in laryngeal cancer [13].
In the present series histological evidence of thyroid gland invasion was observed in 21% patients. Significant relationship was found between histological thyroid gland invasion and preoperative CT scan finding of thyroid cartilage erosion (30%) and also when gross thyroid gland involvement observed intraoperatively (36%). There is also significant pathological gland invasion in advanced clinical T stages (T3 and T4) of the disease (24%) compared to (8%) in early stage disease (T1 and T2). There is significant association between thyroid gland invasions when there is upper oesophageal involvement by the tumour.
Conclusion
After analysing the retrospective data from our study, we would like to suggest that thyroid gland need not be removed routinely in all laryngectomies, unless there is advanced disease with thyroid cartilage erosion and gross thyroid gland involvement or disease with significant subglottic or oesophageal involvement. There is no indication for thyroidectomy when the disease is confined to glottis or subglottis.
Declaration
The paper was presented as a poster in IFNOS, 2014, held at Newyork.
[1]. Kim JW, Han GS, Byun SS, Management of thyroid gland invasion in laryngopharyngeal cancerAuris Nasus Larynx 2008 2(35):209-12. [Google Scholar]
[2]. Croce A, Moretti A, Bianchedi M, Thyroid galnd involvement in carcinoma larynxActa otorhinolaryngol Ital 1991 11(4):429-35. [Google Scholar]
[3]. Sparano A, Chernock R, Laccourreye O, Weinstein G, Predictors of thyroid gland invasion in glottic squamous cell carcinomaLaryngoscope 2005 115(7):1247-50. [Google Scholar]
[4]. Sinard RJ, Tobin EJ, Mazzaferri EL, Hodgson SE, Young DC, Kunz AL, Hypothyroidism after treatment of nonthyroid head and neck cancerArch Otolarygology Head Neck Surg 2000 126(5):652-57. [Google Scholar]
[5]. Wai Ho AC, Ho WK, Yip Lam PK, Yeun AP, Wei WI, Thyroid dysfunction in laryngectomies – 10 years after treatmentHead Neck 2008 30:336-40. [Google Scholar]
[6]. Gurunathan RK, Panda NK, Das A Thyroid gland in carcinoma of the larynx and hypopharynx: analysis of factors indicating thyroidectomyJ Otolaryngol Head Neck Surg 2008 37(3):435-39. [Google Scholar]
[7]. Dadas B, Uslu B, Cakir B, Ozdoğan HC, Caliş AB, Turgut S, Intraoperative management of the thyroid gland in laryngeal cancer surgeryJ Otolaryngol 2001 30(3):179-83. [Google Scholar]
[8]. Brennan JA, Meyers AD, Jafek BW, The intraoperative management of the thyroid gland during laryngectomyLaryngoscope 1991 101(9):929-34. [Google Scholar]
[9]. Hernández JG, Muñoz MG, Thyroidectomy associated with laryngectomy in laryngeal cancer treatment. Is it. routinely necessary?Cir 2005 73(1):3-6. [Google Scholar]
[10]. Mendelson AA, Al-Khatib TA, Julien M, Payne RJ, Black MJ, Hier MP, Thyroid gland management in total laryngectomy: Meta-analysis and surgical recommendationsOtolaryngology–Head and Neck Surgery 2009 140:298-305. [Google Scholar]
[11]. Gilbert RW, Cullen RJ, Peter van, Nostrand AW, Bryce DP, Harwood AR, Prognostic significance of thyroid gland involvement in laryngeal carcinomaArch Otolaryngol Head Neck Surg 1986 112(8):856-59. [Google Scholar]
[12]. Hilly O, Raz R, Vaisbuch Y, Strenov Y, Segal K, Koren R, Thyroid gland involvement in advanced laryngeal cancer: Association with clinical and pathologic characteristicsHead neck 2012 34:1586-90. [Google Scholar]
[13]. Biel MA, Maisel RH, Indications of performing hemithyroidectomy for tumours requiring total thyroidectomyThe American Journal of Surgery 1985 150(4):435-39. [Google Scholar]