Shoulder pain can cause significant pain, discomfort and reduce the ability to perform activities of daily living. Thus, with an estimated prevalence of 16-26%, it is third most common cause of musculoskeletal consultation [1]. Shoulder pathologies include a spectrum of intraarticular and extraarticular disturbances like rotator cuff tears, labral injuries, adhesive capsulitis, impingement syndrome and instability. As it comes in the way of daily activities and significantly affecting the financial earning of the person and family, it is important to deal such cases with accurate diagnosis and treatment. Multiple imaging modalities are currently used to evaluate pathologic conditions of the shoulder like conventional radiography, fluoroscopy, sonography, nuclear medicine and MRI (Magnectic Resonance Imaging).
Arthroscopy is the current gold standard in diagnosing shoulder pathologies. Arthroscopy provides a 20-power magnification, which enhances the direct visualization of the shoulder joint [2]. Despite being the gold standard investigation, arthroscopy does have its disadvantages [3]. The flaccidity of the capsule can be difficult to determine due to the process of the arthroscopic examination itself altering the laxity of the joint. The procedure is invasive and thus carries small risks of complications such as infection, damage to adjacent structures (e.g. musculocutaneous nerve or articular cartilage) and fluid extravasation. Complications may also arise from the anaesthetic [3].
MRI has revolutionized the diagnosis of shoulder pathologies. MRI is a proved sensitive, accurate, cost-effective and a non-invasive tool in investigating shoulder pathology [4]. MRI also provides information on areas not seen in arthroscopy, like the internal structure of the rotator cuff. MRI is helpful in diagnosing an acute/painful shoulder. It is also valuable in assessing the injury status and the severity when many structures are involved where clinical examination becomes difficult. However, false and misleading results are equally reported in the literature. Jonas et al., Torstensen et al., and Green et al., in their studies comparing accuracy of MRI and arthroscopy did not find MRI to be an accurate and effective tool for assessing shoulder pathologic conditions, especially in patients in whom the clinical picture is not clear [5–7]. Disadvantage of MRI is that it is contraindicated in patients who have a cardiac pacemaker, ferromagnetic foreign bodies (particularly in the orbit), and some cochlear implants. Also, some patients are extremely claustrophobic in high-field-strength MRI scanners.
To compare the efficacy of MRI in diagnosing shoulder pathologies in comparison to arthroscopy, considering arthroscopy as the gold standard and to determine the benefits of performing preliminary diagnostic arthroscopy.
Materials and Methods
This is a prospective, comparative study of 11 months duration. Thirty nine consecutive patients, between 18-80 years of age, presenting with chronic shoulder pain or instability of more than 6 weeks, or with clinical signs of impingement or tear were included in the study. The sample size was determined by the statistician who was provided with relevant data. Patients with active infection and with osteoarthritis of shoulder joint were excluded from the study. After fulfilling the selection criteria and giving an informed consent, MRI of the shoulder joint was done. Informed and written consent was given by the patients, who were then subjected to shoulder arthroscopy after required investigations and fitness. All the patients were duly informed about the study. MRI diagnosis was placed into one of the four categories after arthroscopic evaluation:
True positive (TP): MRI diagnosis of tear, confirmed on arthroscopic evaluation.
True negative (TN): MRI diagnosis of no tear was confirmed on arthroscopy.
False positive (FP): MRI showed a tear but arthroscopy was negative.
False negative (FN): If MRI images were negative but arthroscopy showed a tear.
Collected data was presented in the form of tables and diagrams. We calculated true positive, true negative, false positive and false negatives values. The accuracy, sensitivity, specificity, negative predictive value (NPV), and positive predictive value (PPV) were calculated. All the calculations were done using R programming language. Data was analysed for the significant correlation between MRI of shoulder and arthroscopic findings by kappa statistics.
Results
Pain was the most common complaint in shoulder, followed by reduced shoulder movements, instability and apprehension. Males (56%) were affected more than females (44%). Right shoulder (69.23%) was affected more than the left side (30.77%). An 82% patients were above 40 years of age with majority of patients (56%) were in the age group of 40-60 years. Rotator cuff tear was the most common pathology [Table/Fig-1].
Pathology affecting the shoulder joint.
| Pathology | MRI | Arthroscopy | % MRI | % Arthroscopy |
|---|
| Rotator Cuff Tear | 31 | 34 | 79.49 | 87.18 |
| SLAP lesion | 3 | 13 | 7.69 | 33.33 |
| Bamkart’s tear | 12 | 15 | 30.77 | 38.46 |
| Osteochondral Defect | 7 | 7 | 17.95 | 17.95 |
MRI showed excellent sensitivity in the diagnosis of rotator cuff tears (0.91) and osteochondral defects [1]. MRI showed very good sensitivity for Bankart’s lesion (0.8) and had poor sensitivity to detect SLAP tear (0.15). MRI was highly specific in detecting all shoulder pathologies [Table/Fig-2].
Interpretation of the statistical findings.
| TP | FN | TN | FP | Sensitivity | Specificity | PPV | NPV | Kappa | Accuracy | p-value |
|---|
| Rotator Cuff tear | 31 | 3 | 5 | 0 | 0.91 | 1 | 1.00 | 0.63 | 0.73 | 0.9 | 0.146 |
| Superior LabrumAnterior Posterior (SLAP)lesion | 2 | 11 | 25 | 1 | 0.15 | 0.96 | 0.67 | 0.69 | 0.14 | 0.7 | 0.13 |
| Bankart’s tear | 12 | 3 | 24 | 0 | 0.8 | 1.00 | 1.00 | 0.89 | 0.83 | 0.9 | 0.092 |
| Osteochondral defect | 7 | 0 | 32 | 0 | 1 | 1 | 1.00 | 1.00 | 1.00 | 1.0 | 0 |
(TP-True positive, FN-false negative, TN-true negative, FP-false positive, PPV-positive predictive value, NPV-negative predictive value).
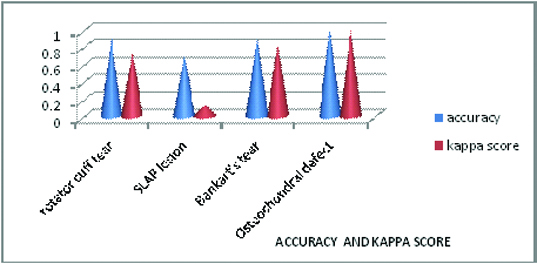
MRI detected rotator cuff tears with kappa score of 0.73 suggestive of substantial correlation. MRI detected Bankart’s tear and osteochondral defects with kappa score of 0.83 and 1.0 respectively suggestive of almost perfect correlation, whereas MRI detected SLAP lesion with kappa score of 0.14 suggestive of only slight correlation.
The accuracy of MRI was highest in diagnosing osteochondral defects (1.0), followed by rotator cuff tear (0.9), Bankart’s tear (0.9) and accuracy was least in diagnosing SLAP lesion (0.7). There were more false negative results than false positive results in our study [Table/Fig-3].
Graph showing accuracy and kappa score.
The positive predictive value of MRI was 1(100%) in detecting rotator cuff tears, Bankart’s tear and osteochondral defects. Hence MRI is useful modality for confirming the clinical diagnosis of these lesions, whereas positive predictive value of MRI is 0.67 (67%) in detecting SLAP lesion, which suggests that MRI is not useful to confirm the clinical diagnosis of SLAP lesion.
The negative predictive value of MRI was highest in detecting osteochondral defects 1 (100%), followed by Bankart’s tear 0.89 (89%), SLAP lesion 0.69 (69%) and rotator cuff tear 0.63 (63%). Hence, MRI is useful in ruling out osteochondral defects and Bankart’s tear, but not very useful in ruling out SLAP lesion and rotator cuff tear.
Discussion
In present study of 39 patients, their age groups were in range of 18 to 80 years. An 82% of patient population was above 40 years of age, with maximum number of patients between 40-60 (56.41%) age group. In the studies done by Van der Windt et al., and Luime JJ et al., on prevalence and incidence of shoulder pain in the general population also had majority of patients with shoulder pathology above 45 years of age [8,9].
The number of male patients (22) was more than female patients (17). Right side (69.23%) was affected more as compared to left side (30.77%). However, Angela Cadogan et al., in their prospective study found little difference with respect to gender of the patient and the side affected [10]. De Mulder K et al., in their study found that rotator cuff tear was the most common cause of shoulder pain [11]. In this study too we had similar findings with 34 arthroscopically diagnosed rotator cuff tears of patients presenting with shoulder pain.
Rotator Cuff Tears
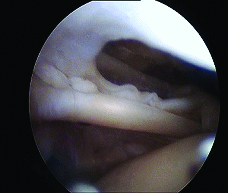
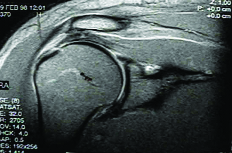
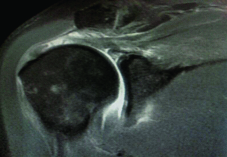
Although the sensitivity and accuracy of MRI [Table/Fig-4,5] in our study in detecting rotator cuff tears was similar to other studies, exception being the study done by KM Muthami et al., that showed a sensitivity of 0.46 [12], but MRI was found to be highly specific in our study as compared to other studies [13–17] [Table/Fig-1,6]. There were 3 rotator cuff tears missed on MRI and diagnosed on arthroscopy. The reasons that these lesions may be missed can be due to the mechanical limitations of detecting undersurface tears and particularly delaminating tears [18–20] and the supraspinatus tendon being oriented obliquely to the imaging plane [20].
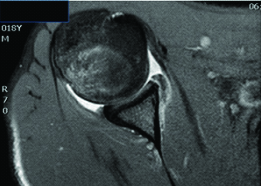
Arthroscopic finding showing Rotator cuff tear
MRI shoulder T1 sagittal cut showing Rotator cuff tear
Arthroscopic finding showing SLAP lesion
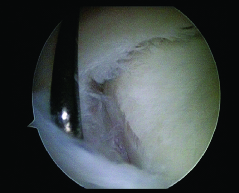
Slap Lesion
Our study found a low sensitivity of MRI in detecting SLAP lesion [Table/Fig-6,7]. Although the MRI sensitivity of detection of superior labral tears in general has mostly been reported to be high [21], some reports document low to moderate sensitivity [13,22–26]. In our study MRI showed high false negatives, with accuracy of 0.7. If MRI is used as the only form of pre-operative screening for this condition, then there may well be many missed SLAP lesions. The probable reasons that the SLAP lesions were either missed or mischaracterized may be because the abnormalities are very small, therefore, inadequate spatial resolution may cause them to go undetected [24], and the course of the glenoid labrum is curved along the glenoid surface, and coronal oblique images are typically not oriented along the long axis of the glenoid, which can lead to partial volume averaging with adjacent fluid and tissues, limiting accuracy [18–20].
MRI shoulder T2 sagittal cut showing SLAP lesion
Bankart’s Tear
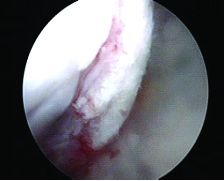
In our study, we found MRI to be highly sensitive and specific in detecting Bankart’s tear [Table/Fig-8,9]. Although sensitivity of MRI was very good, but MRI was more specific than sensitive in detecting Bankart’s tear. There were no false positive results but 3 Bankart’s tear were missed on MRI and diagnosed on arthroscopy in our study. Iannotti JP et al., UP Joshi et al., and CS Lee et al., in their study too had similar findings [27–29], however Eric T Torstensen and Robert M Hollinshead in their study found that MRI identified labral injuries with accuracy of 62% [6], sensitivity 73%, and specificity 58%, that was less as compared to our study. OR Momenzadeh also found MRI to have poor sensitivity and moderate specificity in detecting Bankart’s tear [13].
Arthroscopic finding showing Bankart’s tear

MRI shoulder axial cut showing Bankart’s tear
Joshua M Polster attributed the low sensitivity of MRI in detecting Bankart’s tear to [30]:
Wide variation in the type and position of a Bankarts lesion.
Close proximity and abutment of labrum to capsule and cortical bone which have same signal intensity makes it difficult to distinguish them from one another.
Osteochondral Defect
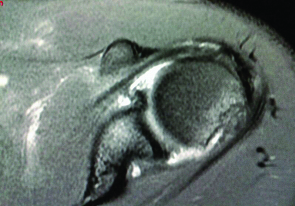
All osteochondral defects were humeral, no glenoid defects were seen. MRI was highly sensitive 100% and specific 100% in diagnosing osteochondral defects [Table/Fig-10,11]. Although the specificity was similar to our study, the sensitivity and accuracy were more than that observed in other studies [13,31–33]. Both positive and negative predictive values of MRI were 1 (100%) in detecting osteochondral defects. MRI proved to be an excellent modality for diagnosing osteochondral defect in our study. [Table/Fig-12] shows a comparative overview of various studies in diagnosing shoulder pathologies.
Arthroscopic finding showing Osteochondral defect
MRI shoulder axial cut showing Osteochondral defect
Comparison of various studies in diagnosing shoulder pathologies
| Rotator cuff tears | SS | SP | PPV | NPV | ACC |
| OR Momenzadeh et al., [13] | 0.91 | 0.92 | 0.93 | 0.89 | - |
| KM Muthami et al., [12] | 0.46 | 0.88 | 0.71 | 0.72 | - |
| GA Naqvi et al., [14] | 0.91 | 0.84 | 0.92 | 0.84 | 0.89 |
| Present study | 0.91 | 1.0 | 1.0 | 0.63 | 0.9 |
| Bankart’s tear | SS | SP | PPV | NPV | ACC |
| UP Joshi et al., [28] | 0.91 | 0.86 | 0.95 | 0.75 | 0.90 |
| OR Momenzadeh et al., [13] | 0.50 | 0.84 | 0.77 | 0.60 | - |
| Lee CS et al., [20] | 0.86 | 0.99 | 0.86 | 0.99 | - |
| Present study | 0.80 | 1.0 | 1.0 | 0.89 | 0.9 |
| SLAP lesion | SS | SP | PPV | NPV | ACC |
| OR Momenzadeh et al., [13] | 0.74 | 0.80 | 0.78 | 0.76 | - |
| Herold et al., [22] | 0.73 | 0.85 | - | - | 0.77 |
| Iqbal HJ et al., [21] | 0.95 | 0.85 | 0.84 | 0.96 | |
| Present study | 0.15 | 0.96 | 0.67 | 0.69 | 0.7 |
| Osteochondral defects | SS | SP | PPV | NPV | ACC |
| Workman TL et al., [33] | 0.97 | 0.91 | - | - | 0.94 |
| OR Momenzadeh et al., [13] | 0.91 | 0.91 | 0.66 | 0.98 | - |
| Denti M et al., [32] | 0.87 | 1.0 | - | - | 0.60 |
| Present study | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
SS-sensitivity, SP-specificity, PPV-positive predictive value, NPV-negetive predictive value, ACC-accuracy
In present study, the sensitivity of MRI in detecting shoulder pathologies varied from poor (0.15) for SLAP lesion to very good (0.8) for Bankart’s tear to excellent for Rotator cuff tears (0.91) and Osteochondral defects (1.0). Although sensitivity of MRI was variable for different shoulder pathologies, MRI was found to be highly specific in detecting all shoulder pathologies. The number of false negative results was more than false positive results. In present study we had only one false positive result in detecting SLAP lesion. The number of false negative results was very high for were not high for rotator cuff injuries and Bankart’s lesion but still the risk of missing these injuries if MRI is considered as the only diagnostic modality prevails.
The positive predictive value of MRI in our study was 1(100%) in detecting rotator cuff tears, Bankart’s lesion and Osteo-chondral defects. Hence MRI was found to be useful in confirming clinical diagnosis of these pathologies. The positive predictive value for SLAP tear was 0.67 (67%), which shows that MRI should not be routinely used to confirm clinical diagnosis of SLAP tear. There was a low negative predicitive value of MRI in our study, that was 0.63 (63%) and 0.69 (69%) for rotator cuff tears and SLAP tears respectively, that shows that MRI should not be routinely used to rule out these shoulder pathologies. Whereas, negative predictive value of MRI was 0.89(89%) and 1(100%) for Bankart’s tear and osteochondral defects respectively, that shows that MRI could be helpful to rule out the above two pathologies.
Ostör AJ et al., studied validation of clinical tests versus magnetic resonance imaging (MRI) in the diagnosis of rotator cuff tear with respect to arthroscopy and found a high sensitivity of clinical tests in detection of shoulder pathology with a low specificity as compared to MRI [34].
In our study, a thorough clinical assessment of each patient preceeded MRI and arthroscopy. The radiologist’s interpretation is an important factor in providing an accurate MRI diagnosis. The clinical findings and provisional diagnosis were discussed with the radiologist in each case, which probably was one of the reasons for high accuracy of MRI in our study. So, a proper clinical assessment and providing detailed clinical findings to the radiologist could improve the accuracy of MRI in the diagnosis of shoulder pathology.
De Mulder K et al., in their study opined that a thorough knowledge of the anatomy, disorders, arthroscopic variations and pathological findings is essential to successfully perform shoulder arthroscopy [11]. Although there is a long learning curve, shoulder arthroscopy is safe, accurate and cost effective when compared to MR imaging [35].
In most of the studies comparing arthroscopy with MRI as well as in our study, the base of reference is arthroscopy presuming that arthroscopy is 100% accurate. Ireland J et al., in their study opined that overall accuracy of arthroscopy varies between 70–100%, depending on the surgeons’ experience [36]. However, In our study, with just 1 false positive result (SLAP tear), assuming that there was a SLAP tear that was missed on arthroscopy, still arthroscopy was found to be highly accurate. Hence, taking arthroscopy as a standard in comparing the accuracy of MRI in diagnosis of shoulder pathology is justified.
Conclusion
The present study supports that MRI is effective in diagnosing rotator cuff tears, Bankart’s tear and ostechondral defects but was not found to be helpful in diagnosing SLAP lesions. Taking into account that with MRI false or misleading results can be as high as 30 percent in specific shoulder pathologies, it is concluded that arthroscopy still remains the gold standard in diagnosing the shoulder lesions. Arthroscopic diagnosis of shoulder pathologies without preliminary MRI is a feasible option when there is a high clinical suspicion and when operative intervention is anticipated, whereas patients in whom a conservative management is indicated can benefit from undergoing a MRI scan first, and not having to undergo an arthroscopy.
Therefore both MRI and arthroscopy have complimentary roles in the diagnosis of shoulder pathology. The skill is knowing which investigation to use and when. An accurate and careful clinical examination still remains the first and essential modality in diagnosing shoulder pathology.
(TP-True positive, FN-false negative, TN-true negative, FP-false positive, PPV-positive predictive value, NPV-negative predictive value).
SS-sensitivity, SP-specificity, PPV-positive predictive value, NPV-negetive predictive value, ACC-accuracy