An Interesting Case of Non-Resolving Hepatogastric Fistula – An Unseen Cause
Vinay G Zanwar1, Sunil V Pawar2, Pravir A Gambhire3, Samit S Jain4, Pravin M Rathi5
1 Senior Resident, Department of Gastroenterology, T.N. Medical College & B.Y.L Nair Hospital, Mumbai, Maharashtra, India.
2 Senior Resident, Department of Gastroenterology, T.N. Medical College & B.Y.L Nair Hospital, Mumbai, Maharashtra, India.
3 Senior Resident, Department of Gastroenterology, T.N. Medical College & B.Y.L Nair Hospital, Mumbai, Maharashtra, India.
4 Assistant Professor, Department of Gastroenterology, T.N. Medical College & B.Y.L Nair Hospital, Mumbai, Maharashtra, India.
5 Professor and Head, Department of Gastroenterology, T.N. Medical College & B.Y.L Nair Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vinay G Zanwar, Senior Resident, Department of Gastroenterology, OPD Building, 7th Floor, T.N. Medical College & B.Y.L Nair Hospital, Mumbai Central, Mumbai-400008, India.
E-mail: drvgzanwar@gmail.com
Hepatic tuberculosis presents one of the rare forms of extra-pulmonary tuberculosis. It is usually secondary to infection in the lung or the gut. Tuberculous liver abscess is the rarer manifestation even in endemic areas of Mycobacterium tuberculosis. Hepatogastric fistula secondary to tuberculous liver abscess has never been reported in literature. We herein report a case of a disseminated tuberculous liver abscess complicated by hepatogastric fistula, which posed a considerable diagnostic challenge. It was treated successfully with anti tubercular drugs. Liver abscess with atypical features and non responsive to antibiotics should raise the suspicious of tuberculosis or fungal infections.
Disseminated tuberculosis, Extra-pulmonary, Liver abscess, Mycobacterium Tuberculosis
Case Report
A 52-year-old man presented in gastroenterology clinic with decreased appetite for four months. He also noticed Jaundice along with itching which resolved spontaneously over three weeks. However, he also had melena which lasted for 10 days. He lost 10 kg weight in last 4 months. He did not complain of cough, expectoration, haemoptysis, abdominal distension or breathlessness. He had consumed 1-2 quarters of alcohol (country Liquor) for 25 years.
On examination he had pallor and bilateral pedal oedema with tender hepatomegaly of 3 cm below right costal area with sharp margin and smooth surface. There was bronchial breathing in right apical region. Blood investigations are shown in [Table/Fig-1]. The chest X-ray showed a cavitatory lesion in right apical zone. Although sputum specimens were difficult to obtain, induced sputum examination was negative for acid-fast staining for three sets. Monteux test was negative. Blood and urine cultures were sterile. An abdominal ultrasound scan revealed 13×11×10 cm hypo echoic heterogeneous vascular lesion in left lobe of liver along with invasion into adjacent part of stomach. During hospital stay, he developed ascites which was high SAAG (serum - ascites albumin gradient). Triple phase Computed Tomography showed large peripherally enhancing and centrally necrotic lesion in left lobe of liver with fistulous communication with body of stomach with adjacent gastric wall thickening, pleural effusion and ascites [Table/Fig-2a]. The appearance was suspicious of a neoplastic lesion of liver, either hepatoma or cholangiocarcinoma with metastasis or an infective lesion. On upper GI endoscopy a fistulous opening was seen with surrounding ulcerations along the lesser curvature of stomach with bilious fluid coming out of it with oesophageal candidiasis [Table/Fig-2b]. Fistulous tract biopsy showed necrotic tissue along with colonies of Candida with no evidence of malignancy [Table/Fig-2c]. CT thorax showed Cavitatory destruction with bronchiectasis, tree in bud appearance in right lung along with nodular opacities in left upper lobe [Table/Fig-2d]. Amoebiasis Ab IgG by Enzyme Immune Assay was positive. With the possibility of amoebic abscess the patient was started on intravenous pantoprazole 40 mg BID, tab metronidazole 800 mg TID, tab fluconazole 150 mg OD, nasojejunal feeding with wide biliary sphincterotomy and plastic biliary stenting done to hasten the healing of fistula [1]. However, not getting any clinical or radiological improvement even after two weeks of treatment, ultrasound guided pus aspiration was undertaken. Pus was negative for gram, acid fast bacilli, amoebiasis and fungal staining, subsequent culture yielded no growth. Serum Alpha Fetoprotein levels were normal. Hence, we planned a liver biopsy for a definitive diagnosis. It showed Inflammation with mild ductular proliferation, anisonucleosis and focal cholestasis in hepatocytes, extensive necrosis with eosinophils, mixed inflammatory cells [Table/Fig-2e] but stained negative for acid fast bacilli, gram, periodic acid-schiff, and Gomori methenamine silver staining. Only when fistulous tract biopsy sample also grew Mycobacterium tuberculosis complex on LJ (Lowenstein Jensen) medium after three weeks of incubation and sputum was positive for Gene Xpert (Rifampicin sensitive), the final diagnosis could be made as alcoholic liver disease with disseminated tuberculosis with tuberculous hepatogastric fistula. He was then treated with four drugs anti-tubercular regime (Isoniazid 300 mg, Rifampicin 450 mg, Pyrazinamide 1500 mg and Ethambutol 800 mg), to which he responded well without side effects. On follow up at 6 weeks, he had weight gain of 7 kg with almost completely resolved liver abscess on ultrasound and healed fistula on endoscopy [Table/Fig-2f].
Significant blood parameters in patient.
| Blood Parameter | Patient value | Reference value |
|---|
| Haemoglobin (g/dL) | 7.2 | 12-14 |
| Total WBC count (×103/mm3) | 14.5 | 4-11 |
| Platelet count (×103/mm3) | 100 | 150 |
| ESR (mm/hour) | 52 | 0-20 |
| Total Protein/albumin (g%) | 5.4/3.2 | 5.5-7 (3.5-5.0) |
| Total Bilirubin (mg%) | 1.0 | 1.0 |
| AST/ALT (IU/L) | 62/36 | 40 |
| ALP (U/L) | 773 | 0-310 |
| HBsAg, Anti HCV, HIV | Negative | |
Triple phase CT abdomen - Large peripherally enhancing and centrally necrotic lesion in left lobe of liver (red arrow) with fistulous communication with body of stomach with adjacent gastric wall thickening (bold black arrow) and ascites.

Upper GI endoscopy - a fistulous opening seen with surrounding ulcerations along the lesser curvature of stomach.

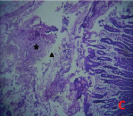
Fistulous tract biopsy – under 40X magnification showing necrotic tissue along with colonies of Candida (star mark) and giant cell (triangle).
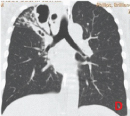
CT thorax - showing Cavitatory destruction with bronchiectasis, tree in bud appearance in Right lung along with nodular opacities in Left upper lobe.
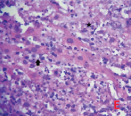
Liver biopsy - under 40X magnification showing inflammation with mild ductular proliferation (bold black arrow), extensive necrosis with eosinophils, mixed inflammatory cells (star mark).
Upper GI endoscopy - showing a healed fistulous opening after 6 weeks of anti-tubercular treatment.

Discussion
Common causes of liver abscess are Entamoeba histolytica and pyogenic organisms. Tubercular liver abscess (TLA) is a rare clinical entity. It is usually associated with a focus of infection in lungs or intestinal tract or in an immunocompromised state [2]. The diagnosis is delayed or missed in most instances owing to rarity of the disease and nonspecific findings, and can be confused with pyogenic abscess, amoebic liver abscess or hepatocellular carcinoma. In literature approximately hundred cases of TLA have been reported till now [3]. Rupture of a liver abscess is well known complication usually occurring in the peritoneal cavity, pleural cavity, pericardium and rarely retro peritoneum, kidney, inferior vena cava and rectus sheath [4]. However, hepatogastric fistula complicating tubercular liver abscess has never been reported as occurred in our case.
Isolated TLA without involvement elsewhere is even rarer occurrence [5]. In older series the prevalence of TLA is 0.34% in patients with hepatic tuberculosis [6]. In another study from India, out of 72 cases of liver abscess, 5 came out to be tubercular and alcohol was found as most consistent co-morbid association [5]. Very first of the TLA case was reported by Bristowe in 1858 [7]. Immunocompromised individuals with AIDS, diabetes mellitus, chronic renal failure and steroid therapy were highly predisposed for TLA [8]. Our patient was diabetic and chronic alcoholic. The diffuse hepatic involvement with pulmonary or miliary TB, diffuse hepatic infiltration without pulmonary involvement and focal liver abscess or tuberculomas are three forms of hepatic TB. Through haematogenous spread Tubercle bacilli reach the liver; via hepatic artery in case of miliary hepatic TB, whereas portal vein in case of focal liver TB [9]. Ultimately the granuloma formation occurs whatever may be the mode of entry.
Diagnosis of TLA is often missed or delayed due to rarity of disease, and nonspecific sign, symptoms. Vague abdominal pain, low grade fever, anorexia, fatigue, night sweats and loss of weight were some of these reported clinical features.
Jaundice is uncommon and may be caused by extra or intrahepatic obstruction. Biochemical investigations are highly variable in TLA but in many instances a marginal elevation of liver aminotransferase with a disproportionate rise in alkaline phosphatase is consistent finding in various studies [5,10]. Even the radiological appearance of the TLA on USG and CT can easily be confused with amoebic or pyogenic liver abscess or hepatoma [11]. Hence the definitive diagnosis of TLA needs demonstration of AFB in pus, aspirate or biopsy. Recently PCR is also found as valuable technique in detecting Mycobacterium tuberculosis in with rapidity [11]. Mycobacterial culture remains the gold standard but has inherent limitation of low yield and availability. The diagnosis of a hepatogastric fistula rests on endoscopic or imaging evidence of a site of rupture into the gastrointestinal tract. Anti – tubercular drugs remains the cornerstone for treatment of TLA with some controversy regarding duration of chemotherapy and necessity of drainage. In the present case, the diagnosis was made after the culture grown mycobacterium tuberculosis complex. Also, in our case tubercular aetiology was never anticipated. It was only when the patient failed to respond to anti-amoebic agents and antibiotics treatment. Percutaneous drainage was not undertaken in the above case as it seemed likely that there was at least some spontaneous drainage into the stomach.
Conclusion
This particular case responded well to systemic drugs and has been reported for the rarity of its presentation and to highlight the importance of microscopic or culture in diagnosis for tuberculosis in evaluation of space occupying lesion of liver in endemic countries like India.
[1]. Sandeep SM, Banait VS, Thakur SK, Bapat MR, Rathi PM, Abraham P, Endoscopic biliary drainage in patients with amebic liver abscess and biliary communicationIndian J Gastroenterol 2006 25(3):125-27. [Google Scholar]
[2]. Akçay MN, Polat KY, Oren D, Oztürk G, Primary tuberculous liver abscess. A case report and review of literatureInt J Clin Pract 2004 58(6):625-27. [Google Scholar]
[3]. Patankar T, Prasad S, Armao D, Mukherji SK, Tuberculous abscesses of the liverAm J Roentgenol 2000 174(4):1166-67. [Google Scholar]
[4]. Kim ES, Lee SY, Yeom JO, Cho YS, Education and Imaging. Hepatobiliary and pancreatic: Liver abscess complicated by a hepatogastric fistulaJ Gastroenterol Hepatol 2013 28(1):206 [Google Scholar]
[5]. Sharma S, Gupta HK, Chopra KK, Mahajan RK, Sharma BB, Puri M, Tubercular liver abscess: a distinct entity not to be missed Tubercular liver abscess: a distinct entity not to be missedThe Indian Journal of Tuberculosis 2014 61(3):236-41. [Google Scholar]
[6]. Kubota H, Ageta M, Kubo H, Wada S, Nagamachi S, Yamanaka T, Tuberculous liver abscess treated by percutaneous infusion of antituberculous agentsIntern Med 1994 33:351 [Google Scholar]
[7]. Gracey L, Tuberculous abscess of liverBr J Surg 1965 52:442-43. [Google Scholar]
[8]. Koksal D, Koksal AS, Koklu S, Cicek B, Altiparmak E, Sahin B, Primary tuberculous liver abscess: a case report and review of the literatureSouthern Med J 2006 99:393-95. [Google Scholar]
[9]. Purl AS, Nayyar AK, Vij JC, Hepatic tuberculosisInd J Tub 1994 41:131 [Google Scholar]
[10]. Oliva A, Duarte B, Jonasson O, Nadimpalli V, The nodular form of local hepatictuberculosis. A reviewJ Clin Gastroenterol 1990 12(2):166-73. [Google Scholar]
[11]. Hassani KIM, Ousadden A, Ankouz A, Mazaz K, Taleb KA, Isolated liver tuberculosis abscess in a patient without immunodeficiency: a case reportWorld J Hepatol 2010 2:354 [Google Scholar]