Hernia repair is one of the most common surgery done by general surgeons all over the world. So the descriptions of hernia surgery date back to the Hammurabi of Babylon and Egyptian papyrus. The first surgeon who gets considerable credit for hernia repair is Edoardo Bassini [1]. 27% of men and 3% of women have the chance to undergo a hernia repair in their lifetime, which is quite high [2]. Though the frequency of surgery for hernia is high, very few surgeries have good results.
Many types of hernia repair are described, traditional methods like modified bassini’s repair, shouldice repair and lichtenstein mesh repair and now laparoscopic mesh repair [3]. Many comparative randomized trials have showed that in open hernia repair, lichtenstein tension free repair is superior to traditional tissue approximation methods [4,5].
A comparative study between LMR and MBR+LMR, to evaluate the postoperative complications, early return to work, and recurrence rate for these two techniques.
Materials and Methods
This was a comparative randomized study, which was carried out over a period of 2 years (September 2011 to September 2013), in Department of General Surgery, MNR Medical Hospital, Sangareddy, India. A 50 consecutive patients presenting with direct inguinal hernia were included in this study without bias on a serial basis. Consent has been obtained from all the participants and explained about the nature and purpose of the study in their own language.
Indirect inguinal hernias, congenital hernias, hernia’s in pregnant women, recurrent hernias and all complicated hernias were excluded.
The diagnosis was purely on clinical findings. Routine investigations, for the fitness of the patient to undergo surgery. Spinal anaesthesia was used in both groups.
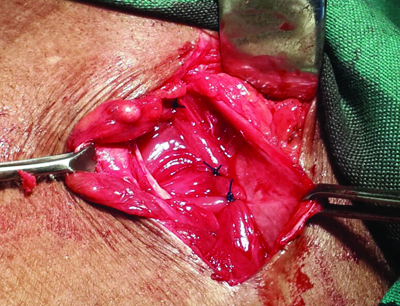
For all cases, a classical incision i.e., 2 cm above and parallel to the medial three fifths of the inguinal ligament (right or left side based on side of hernia). Modified bassin’s repair+Lichtenstein tension free mesh repair – after the above said incision, external oblique aponeurosis is identified and incised along the direction of fibres. Cord is identified and sac is separated from cord structures. Conjoint tendon was approximated to inguinal ligament and mesh was placed over it and fixed to inguinal ligament below and to the conjoint tendon above with 1-0 prolene interrupted sutures with key stitch to the periosteum of symphysis pubis [Table/Fig-1,2,3 and 4].
Interrupted sutures between conjoint tendon and inguinal ligament.
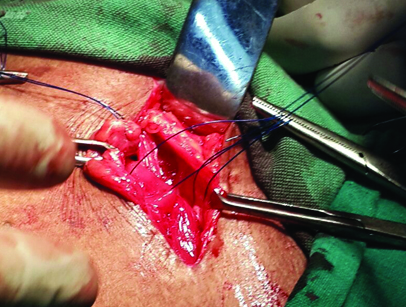
Interrupted sutures with 1-0 prolene between conjoint tendon and inguinal ligament.
Mesh placed over the posterior wall repair.
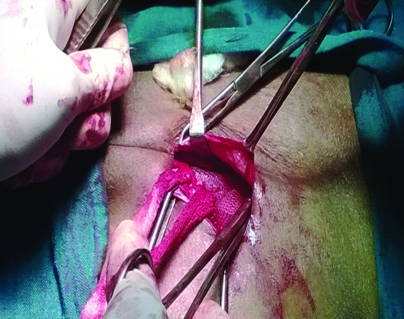
Mesh is placed over the posterior wall and the cord is repositioned.
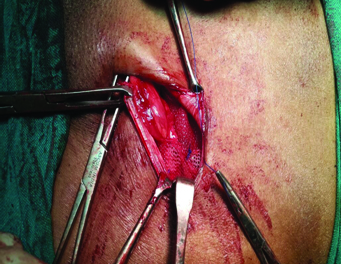
Lichtenstein repair – after dissection, the prolene mesh was placed on the defect and fixed to inguinal ligament below, to the conjoint tendon above with 1-0 prolene and key stitch to the periosteum of symphysis pubis.
In postoperative period, inj diclofenac 75mg BD was given for 48 hours to both the groups for pain relief and postoperatively patients were evaluated for pain, haematoma, seroma, infection and retention of urine. Suture removal was done on 7th postoperative day. No patients were lost on follow up. Postoperative follow-up was through periodic physical examination and through telephonic conversations when physical examinations were missed. All patients were followed up for two years postoperatively with regular follow up monthly for first three months, then once a month for a year and then followed every 6 months to see any postoperative complications. Primary end points of our study were determined to be quality of pain free life postoperatively and no evidence of recurrence.
Statistical Analysis
In this study, descriptive statistical analysis has been used. Results were presented as Mean±SD and results are presented numerically. Student’s t-test and chi-square test have been used. Randomization was done by using the SAS software.
Results
Site of Hernia
Out of 50 direct hernia patient, 20 cases (40%) were of right side, 18 cases (36%) of left side and 12 cases (24%) were of bilateral with distribution of groups being similar [Table/Fig-5].
| Right/Left/Bilateral | LMR (n=25) | LMR+MBR (n=25) | TOTAL (n=50) |
|---|
| Right | 11 (22%) | 9 (18%) | 20 (40%) |
| Left | 9 (18%) | 9 (18%) | 18 (36%) |
| Bilateral | 5 (10%) | 7 (14%) | 12 (24%) |
Duration of Surgery
The mean duration of surgery is more for LMR+MBR, compared to LMR [Table/Fig-6]. The duration of surgery was significantly longer in LMR+MBR by approximately 10-15 minutes (p-value <0.0001). In the initial period of LMR+MBR surgeries, the duration was about 55-60 min, but after 15 surgeries, the duration of surgery was about 40-45 min. The duration of surgery was decreased as the learning curve is improved.
| Duration of surgery (min) | Group LMR (n=25) | Group LMR+MBR (n=25) | Total (n=50) |
|---|
| Min - Max | 24 - 54 | 38 - 64 | 24 - 64 |
| Mean±S.D | 34.56 ± 9.631 | 47.56±9.747 | 41.06±11.622 |
Comparison of Post Operative Complications
Pain
A Visual Analogue Scale was used, to quantify the pain. This scale consists a horizontal line marked with whole numbers marked from 0 to 10 and we have asked the patient to mark on it [6,7]. We have taken the mean of pain scores on the day of surgery (evening, after the effect of spinal anaesthesia faded), postoperative days 0, 1, 7 and 30th day were considered for comparison between the two groups. Pain was more in LMR+MBR group than LMR group [Table/Fig-7]. However, the difference in pain levels was not statistically significant.
| Postoperative pain (day) | Group LMR (n=25) (mean±SD) | Group LMR+MBR (n=25) (mean±SD) | Total (n=50) | p-value |
|---|
| POD 0 | 5.56±0.916 | 5.96±0.734 | 5.76±0.825 | 0.0949 |
| POD 1 | 4.48±0.918 | 4.84±0.746 | 4.66±0.832 | 0.1346 |
| POD 7 | 2.44±0.96 | 2.48±0.82 | 2.46±0.89 | 0.8748 |
| POD 30 | 0.48±0.50 | 0.416±0.50 | 0.448±0.50 | 0.6529 |
Haematoma
In our study, a total of 2 patients (1 each from both the study groups) developed haematoma postoperatively [Table/Fig-8].
Incidence of haematoma according to the type of repair.
| Technique of repair | Number of patients in group | Number of patients with haematoma | % |
|---|
| LMR | 25 | 1 | 2 |
| LMR+MBR | 25 | 1 | 2 |
| Total | 50 | 2 | 4 |
p-value is 1.00, statistically not significant
Seroma
In this study 18% of patients suffered with seroma collection, of which 8% in LMR & 10% in LMR+MBR group [Table/Fig-9].
Incidence of seroma according to the type of repair.
| Technique of repair | Number of patients in group | Number of patients with seroma | % |
|---|
| LMR | 25 | 4 | 8 |
| LMR+MBR | 25 | 5 | 10 |
| Total | 50 | 9 | 18 |
p-value is 0.7196, statistically not significant
Infection
In this study, mesh was infected in only 1 patient from LMR group and none from LMR+MBR group [Table/Fig-10].
Incidence of Infection according to the type of repair.
| Technique of repair | Number of patients in group | Number of patients with infection | % |
|---|
| LMR | 25 | 1 | 2 |
| LMR+MBR | 25 | 0 | 0 |
| Total | 50 | 1 | 2 |
p-value is 0.3223, statistically not significant
Recurrence
In this study, we have only 1 recurrence, from the LMR group. In our study, there was no recurrence in LMR+MBR group [Table/Fig-11].
Incidence of recurrence according to the type of repair.
| Technique of repair | Number of patients in group | Number of patients with recurrence | % |
|---|
| LMR | 25 | 1 | 2 |
| LMR+MBR | 25 | 0 | 0 |
| Total | 50 | 1 | 2 |
p-value is 0.3223, statistically not significant
Other Postoperative Complications
In this study, retention of urine is seen in total 3 patients, out of which 2 patients are from LMR group and 1 were from LMR+MBR group. Minor complications like painful scar, ischemic orchitis, osteitis pubis, scrotal ecchymosis were not seen [Table/Fig-12].
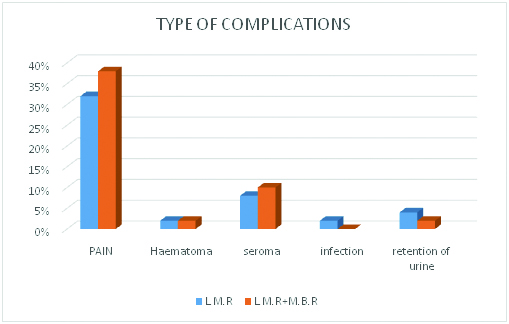
Comparison of postoperative complication between the two types of repairs.
Postoperative Stay
In our study, we have also compared the length of the stay in hospital. The length of the hospital stay is more in LMR+MBR than LMR, but statistically not significant [Table/Fig-13].
Postoperative hospital stay.
| Postoperative stay | LMR (n=25) | LMR+MBR (n=25) | Total (n=50) |
|---|
| 1-2 days | 3 | 2 | 5 |
| 3-4 days | 12 | 10 | 22 |
| 5-7 | 7 | 9 | 16 |
| >7 days | 3 | 4 | 7 |
| Mean±S.D | 4.68±2.115 | 5.16±2.211 | 4.92±2.163 |
p-value is 0.4367, statistically not significant
Discussion
For hernia, many surgical procedures have been described. Because of the recurrence of hernia, there is no standard treatment for hernia till now. In review of literature, there were recurrences even with the use of mesh. The recurrence rate for inguinal hernias after doing primary repair is about 0.5% - 10% [8–10]. There are many publications claiming that mesh repair is the best procedure, but non-mesh repair still continues and we are in search of best surgical technique [11]. In present era the indication for Bassini’s repair is the conditions where mesh is contraindicated like infection.
In our study, we have selected direct inguinal hernias because abdomen muscle is lax and have poor abdominal muscle tone. As people, grow old, the tone of the abdominal muscle becomes lax and weak, which is a major contributing factor for the recurrence. For this reason a proper strengthening of posterior wall of the inguinal canal is atmost importance, especially in big direct hernias.
This is the first study, where we compared MBR+LMR v/s LMR. In this study, we made an attempt to give highest possible strength by combining modified bassini’s+lichtenstein mesh repair. Generally direct hernia defects in old age are large and in open method, it is not easy to cover the large defect with mesh. So this method was used to cover the defect by modified bassini’s repair and reinforced by lichtenstein mesh repair. Mesh will give additional protection to abdominal muscle. In our study all surgeries were performed by a single surgeon, so that there would not be any difference in the outcome of study.
Recurrence rate is considered to be the essential factor in assessing the efficacy of the surgical procedure in hernia repair. The recurrence rate for bassini repair is around 10-40% [12,13]. So many modifications are done to bassini’s procedure; popular among them are shouldice repair and cooper’s ligament repair. The recurrence rate for shouldice repair is about 1-7% [14,15]. In Lichtenstein mesh repair, the recurrence rate is around 0.5-4% [16–19]. The idea of deciding the best surgical technique for hernia repair using the recurrence rate as a factor is controversial [12,20].
Other factors consider for the efficacy of hernia repair are the postoperative complications. Aasvang and Kehlet study showed that incidence of chronic pain after inguinal herniorrhaphy was 12% [21]. O’Dwyer and colleagues study had found severe or very severe chronic post herniorrhaphy pain in 3% of patients, which had severe effect on patient’s capacity to do work [22]. The wound infection rates are around 1-7% [23]. In a study by MM Harjai study, it was 4.08% for LMR and 6.78% for MBR [5]. In a study conducted by Finley RK Jr, the urinary retention is around 0.2% to 13% based on anaesthesia [24]. Injury to vas deferens is 0.3% in adults and 0.8-2% in children [25]. Atrophy of testis is seen in 0.5% of primary hernia repair and 5% in recurrent hernia repair [25].
There are many variations in the incidence of complications, mainly due to age, gender, co-morbid illness, experience of a surgeon, duration of surgery, method of repair, and mode of anaesthesia. So, the choice of surgery should be based on the above factors. Compared with other studies our study shown no recurrence and less postoperative complications [Table/Fig-14]. The above table describes, hernia repair by MBR+LMR is superior to LMR.
Comparison of outcome of different techniques used for repair of hernia. open hernia Abbreviation: LMR – Lichenstein Mesh Repair, MBR – Modified Bassini’s repair
| Studies | Technique | Recurrence | Painful scar | Infection | Haematoma |
|---|
| Current study | LMR+MBR | 0% | 0% | 2% | 2% |
| 2014, Kai Xiong Cheong [4] | LMR | 3.84% | 1.15% | 0.57% | 4.80% |
| 2012, Berrevoet et al., [16] | LMR | 2.86% | - | - | - |
| 2013, L. Timisescu et al., [17] | LMR | 1.09% | 0% | 5.49% | 9.89% |
| Anuradha Anand et al., [18] | LMR | 0.82% | 2.25% | 0.20% | - |
| 2011, Konrad Pielacinski et al., [19] | LMR | 3.39% | - | - | 10.17% |
Conclusion
This is the first study, which compared MBR+LMR v/s LMR, where MBR+LMR is superior to LMR alone for inguinal hernia in patients with large defect, because of low recurrence rate (0%) and low post operative complications though the length of the operation is more in our study (p-value <0.0001). We want to conclude that in all direct inguinal hernias with large posterior wall defects can undergo MBR+LMR, which helps in approximating the posterior wall and reinforcing with the mesh, which prevents recurrence. With this study we made an attempt to find the best procedure for large direct inguinal hernias. In future further similar studies on larger scale to find accurate results are needed.