Stewart Treves Syndrome in a Woman with Mastectomy
Sevil Alan1, Habibullah Aktas2, Ömer, Faik Ersoy3, Alpay Aktümen4, Harun Erol5
1 Assistant Professor, Department of Dermatology and Venereology, Akdeniz University School of Medicine, Turkey.
2 Assistant Professor, Department of Dermatology and Venereology, Karabük Education and Research Hospital, Turkey.
3 Assistant Professor, Department of Dermatology and Venereology, Karabük Education and Research Hospital, Turkey.
4 Assistant Professor, Department of Pathology, Karabük Education and Research Hospital, Turkey.
5 Assistant Professor, Department of Pathology, Karabük Education and Research Hospital, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sevil Alan, Akdeniz Üniversitesi Hastanesi, 07070, Antalya, Turkey.
E-mail: alan_sevil@yahoo.com
Stewart Treves Syndrome is an angiosarcoma generally seen long time after radical mastectomy in breast carcinoma patients in chronic lymphoedema area. It’s an angiosarcoma developed on a long standing lymphoedema, following a radical mastectomy. An 86-year-old woman was referred to our Dermatology outpatient clinic which developed a giant erythematous, oedematous, purplish lobulated plaque on her right forearm anteromedially with a few satellite erythematous papulonodules on her arm. The pathology revealed spindle-shaped tumour cells invading dermis with vascular differentiation into the subcutaneus tissue which are compatible with a diagnosis of angiosarcoma.
Angiosarcoma, Breast cancer, Lymphoedema
Case Report
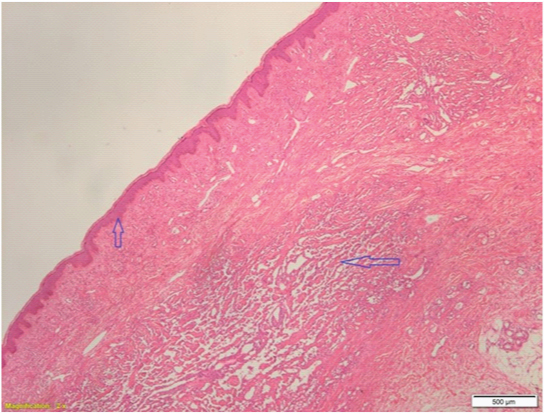
A 86-year-old woman presented to our department complaining about a giant erythematous, oedematous, purplish lobulated plaque on her right forearm anteromedially with a few satellite erythematous papulonodules on her arm [Table/Fig-1]. In history, a small nodule appeared 6 months ago on the forearm and it has grown rapidly within months. The patient had undergone a radical mastectomy operation 15 years ago due to right breast carcinoma and she has a diagnosis of chronic lymphoedema on her right arm for approximately 10 years. An insicional biopsy was done to establish the diagnosis. The pathology revealed spindle-shaped tumour cells invading dermis with vascular differentiation into the subcutaneus tissue which are compatible with a diagnosis of angiosarcoma [Table/Fig-2]. Immunohistochemical study revealed a diffuse expression of CD34, CD31 and vimentin confirming the diagnosis of epithelioid angiosarcoma. CT was requested to screen distant metastasis. No metastasis were found elsewhere. The patient was oriented to the oncology center who was already in its follow-up. Paliative amputation was performed of right forearm.
Oedematous, lobulated, erythematous purplish plaque covering almost all anteromedial aspect of right arm with satellite nodules around.

Up arrow indicate epidermis and horizontal arrow indicate tumour.
Discussion
Stewart-Treves syndrome was first described by Fred Stewart and Norman Treves in 1948 [1]. It’s an angiosarcoma developed on a long standing lymphoedema, following a radical mastectomy [2]. They reported a series of six patients with angiosarcoma occurred where lymphoedema existed after a latency period of 5 to 11 years after radical mastectomy [1]. Furthermore, the Stewart-Treves syndrome has not only been developed in post mastectomy, it can occur congenital, post radiotherapy, post trauma or post burn [1]. Radiation therapy and chronic lymphoedema are both associated as major aetiological factors in this entity [3]. The appearance of the lesion occurs within 10 years in average ranging 1 to 26 years [2]. The frequency is estimated at approximately 0.45% in patients who survive longer than five years after a mastectomy [3]. It definetely indicates a poor prognosis and only 10% of patients can survive for 5 years [4]. Radical surgery is the best treatment to date for this rare disease [5]. Although the disease is mostly seen in upper limbs particularly ipsilateral to breast tumour, it also involve lower limb [6]. It almost indicates a poor prognosis that patients are lost within months after the diagnosis [7]. The series of Woodward et al., recording 162 cases of lymphangiosarcomas after mastectomy, supported to better describe their natural history [8]. The fundamental pathophysiology of this disease is still debated [6]. It is hypothesized that lymphatic blockage encourages the growth of lymphatic vessels through growth factors and cytokines [4]. This is verified by the fact that there is lymphatic vessel proliferation in unaffected areas of the limb [4]. The relation of adjuvant breast irradiation maintains unclear in the pathogenesis of Stewart-Treves syndrome after mastectomy [1]. Nevertheless, the practice of axillary irradiation after an axillary lymph node dissection is well-known to increase the risk of post-treatment lymphoedema [4].
Immunohistochemical study shows usually positive staining for endothelial cell markers such as laminin, antibodies against factor VIII, type IV collagen and CD31 [5]. High level gene amplification of MYC is also a disparate finding of cutaneous secondary angiosarcomas, which develop after chronic lymphoedema or irradiation [6]. This is in contrast to primary angiosarcomas, which may disposed to be present deep in soft tissue and do not have high MYC gene amplification [6].
Treatment possibilities have limited success. Some authors recommend large resection even an amputation or disarticulation preceding or following by radiation therapy. Systemic or local mono or polichemotherapy are choices for advanced tumours [8]. In early stages, angiosarcomas often confused with benign vascular proliferation or traumatic ecchymosis. The differential diagnosis includes Kaposi’s sarcoma and metastasis [9].
Conclusion
We suggest that regular follow-up for every post mastectomy lymphoedema and recommend skin biopsy in every doubtful lesion, so radical surgery can be possible at the time of diagnosis.
[1]. Stewart FW, Treves N, Lymphangiosarcoma in postmastectomy lymphoedema; a report of six cases in elephantiasis chirurgicaCancer 1948 1(1):64-81. [Google Scholar]
[2]. Benmansour A, Laanaz S, Bougtab A, Stewart-Treves syndrome: a case reportPan Afr Med J 2014 1(19):2doi: 10.11604/pamj.2014.19.2.4178 [Google Scholar]
[3]. Da Veiga RR, do Nascimento BA, Carvalho AH, de Brito AC, Bittencourt Mde J, Stewart-Treves syndrome of the lower extremityAn Bras Dermatol 2015 90(3 Suppl 1):232-34.doi: 10.1590/abd1806-4841.20153926 [Google Scholar]
[4]. Sharma A, Schwartz RA, Stewart-Treves syndrome: pathogenesis and managementJ Am Acad Dermatol 2012 67(6):1342-48. [Google Scholar]
[5]. Harrison WD, Chandrasekar CR, Stewart-Treves syndrome following idiopathic leg lymphoedema: remember sarcomaJ Wound Care 2015 24(6 Suppl):5-7.doi: 10.12968/jowc.2015.24.Sup6.S5 [Google Scholar]
[6]. McKeown DG, Boland PJ, Stewart-Treves syndrome: a case reportAnn R Coll Surg Engl 2013 95(5):80-82. [Google Scholar]
[7]. di Meo N, Drabeni M, Gatti A, Trevisan G, A Stewart-Treves syndrome of the lower limbDermatol Online J 2012 18(6):14 [Google Scholar]
[8]. Woodward AH, Ivins JC, Soule EH, Lymphangiosarcoma arising in chronic lymphoedematous extremitiesCancer 1972 30:562-72. [Google Scholar]
[9]. Noguchi M, Hasegawa H, Tajiri K, Stewart-Treves syndrome. A report of two cases with a review of Japanese LiteratureJpn J Surg 1987 17:407-12. [Google Scholar]