Introduction
Wheezing is a very common respiratory symptom during childhood. Epidemiological studies have reported that almost one-third of all children wheeze at least once in the first three years of life, with nearly 50% of all children having at least one wheezing episode by the age of 6 years [1–3]. However, early childhood wheezing is a heterogeneous condition, which has several phenotypic expressions and a complex relationship with the development of asthma later in life [4]. Wheeze is defined as continuous high pitched sound with musical quality emitting from the chest during expiration which lasts for more than 250 msec [5].
Low serum 25-hydroxy vitamin D levels have been associated with increased risk of lower respiratory tract infections in young children as has been shown by various epidemiologic studies [6,7]. Adding on, evidence is there suggesting enhanced risk of childhood wheezing associated with low levels of maternal intake of vitamin D during pregnancy and umbilical cord blood 25(OH)D [6,8]. Various interventional trials support these associations by establishing lowered respiratory tract infections in children having vitamin D supplementation [9,10].
Recurrent wheeze is defined as three or more episodes of parentally reported wheeze in the past 12 months of life [1]. The prevalence of wheeze is 6.2% in India [11]. Studies suggest reasons for newborns with low serum vitamin D including low sun exposure, no food fortification of Vitamin D, month of being born, history of asthma and young maternal age [12]. Evidence suggest lower the amount of Vitamin D, the higher the risk for wheezing [13].
Differential Diagnosis of Wheezing includes long list including infections, asthma, anatomic abnormalities like TEF, vascular ring, Broncho-pulmonary dysplasia, Aspiration syndromes, Interstitial lung disease, often making it hard to pin point the reason [14]. Although there are many risk factors for development of recurrent wheezing [15,16] an emerging risk factor of particular interests is Vitamin D status [17]. The evidence for the possible link between vitamin D and respiratory disease comes from multiple studies [18–21]. Role of maternal vitamin D uptake and its relation to wheezing in early childhood also has been probed [22]. In the Childhood Asthma Management Program (CAMP) [23] those with low baseline 25(OH) Vitamin D levels (< 75nmol/L) were more likely to have a severe asthma exacerbation over a 4 months period [24].
Vitamin D present in various forms including 1α, 25(OH2) D3 and its role in humans has been studied in detail, its role has been well established in the demineralization process of bone, mediated by intricate balance of serum calcium, phosphorus and Vitamin D as a hormone and its defeciency leading to rickets among children and osteomalacia in Adults [25]. Its role in gene mediated expression of Bronchial smooth muscle cell following 1α, 25(OH2) D stimulation also has been probed [26]. Studies have shown the role of Vitamin D in genetic related cell movement important for airway remodeling. Its other form 1α, 25(OH2) D3 induces genes in Ca related pathways leading to bronchial smooth muscle contraction [27–31].
Contrary to the belief, the data available in published literature suggests Vitamin D deficiency is very common in India in all the age groups and both the sexes across the country [32–35].
In our hospital setup, we have found that large number of wheezy children was presenting with florid rickets and signs of Vitamin D deficiency but no other causes of wheeze were found on investigation. Our study has been proposed to find out the association between Vitamin D deficiency and recurrent wheeze in children less than 3 years of age.
Aim
To determine the severity of Vitamin D deficiency and its association with recurrent wheeze in children less than 3 years of age.
Materials and Methods
To study the serum levels of Vitamin D in recurrent wheezy children less than 3 years of age and their age matched controls.
Study Hypothesis: “Vitamin D deficiency is associated with recurrent wheezing in children below 3 years of age and its levels are significantly lower in these children.”
Setting: This study was a Hospital based case control study conducted in the Department of Paediatrics, Lokmanya Tilak Municipal Medical College & General hospital, a tertiary care hospital in Mumbai. From June 2013 to May 2014. Consecutive type of non-probability sampling was followed for selection of study subjects, with a case sample size of 61 and similar number of controls fulfilling inclusion and exclusion criteria who gave informed consent to participate in study were enrolled with a total sample size of 122 (61 cases and 61 controls). Exclusive Breast Feeding remains the mainstay of infant feed, and we in our study also took history of breast feeding and tried to explore its impact on Vitamin D levels. Breastfeeding was categorized as exclusive breastfeeding for 1st 6 months of life and after six month on complementary feed i.e. on breast milk and other feed. Clearance from Ethical committee in College was taken.
Inclusion criterion: Children <3 years of age, who had 3 or more episodes of wheeze (recurrent wheezers) in the past 12 months without any obvious cause were included in study. For control group, same number of less than 3 years of age children who came to OPD/paediatric emergency for minor and nonspecific complain were included. Children whose parents were willing to participate in the study. A written informed consent was obtained from the parents for enrolling their child for the study.
Exclusion Criteria: Children with history of intake of vitamin D supplementation and children with known causes of wheezing were excluded.
A pre-formed, pre-tested, structured interview schedule was used to obtain information from all study subjects. A detailed history and clinical examination was done for each child.
Breastfeeding history was recorded. Breastfeeding was categorized as exclusive breastfeeding for 1st 6 months of life and after six month on complementary feed i.e. on breast milk and other feed.
Vitamin D Estimation: Kit used for estimation is DLD Diagnostika GMBH 25(OH) Vitamin D ELISA from Germany. Standard Definition of Vitamin D and its deficiency were used [36].
Statistical Analysis
All the collected data was entered in Microsoft Excel sheet after generation of proper template. It was then transferred to SPSS version 17 software for statistical analysis.
Results
Very severe Vitamin D deficiency (< 5ng/ml) was observed in 23% of cases while none had vitamin D levels above 30 ng/ml. Optimum levels were observed in 44.3% of controls while none had levels below 10 ng/ml. Significantly lower levels of Vitamin D were observed in cases compared to controls (p< 0.05) [Table-Fig-1].
Distribution of Subjects based on Vitamin D levels.
| Vitamin D Levels (ng/ml) | Group | Total |
|---|
| Cases | Controls |
|---|
| Very Severe deficiency (< 5) | N | 14 | 0 | 14 |
| % | 23.00% | 0.00% | 11.50% |
| Moderate deficiency (5-9.9) | N | 23 | 0 | 23 |
| % | 37.70% | 0.00% | 18.90% |
| Deficiency (10-19.9) | N | 8 | 7 | 15 |
| % | 13.10% | 11.50% | 12.30% |
| Insufficiency (20-29.9) | N | 16 | 27 | 43 |
| % | 26.20% | 44.30% | 35.20% |
| Optimal Level (≥ 30) | N | 0 | 27 | 27 |
| % | 0.00% | 44.30% | 22.10% |
| Total | N | 61 | 61 | 122 |
| % | 100.00% | 100.00% | 100.00% |
p- value < 0.05*, *Chi-Square test
On observing the distribution of various laboratory parameters, we found that controls had significantly greater mean Vitamin D (31 vs. 11.6 ng/ml) and S. calcium (9.2 vs. 8.9 mg/dl) values. The difference was statistically significant (p<0.05) Alkaline Phosphatase levels were significantly higher in cases than controls (585.4 vs. 302.1 IU/L). The difference was statistically significant (p<0.01) [Table-Fig-2].
Distribution of Subjects based on Mean Laboratory Parameters.
| Variables (n-122) | Group | N | Mean | Std.Deviation | p-value |
|---|
| Vitamin D (ng/ml) | Cases | 61 | 11.6 | 7.4 | < 0.05 |
| Controls | 61 | 31.0 | 8.7 |
| Calcium (mg/dl) | Cases | 61 | 8.9 | 0.7 | < 0.05 |
| Controls | 61 | 9.2 | 0.7 |
| Inorganic Phosphorus (mg/dl) | Cases | 61 | 4.2 | 1.3 | 0.34 |
| Controls | 61 | 4.5 | 1.3 |
| Alkaline Phosphatase (IU/L) | Cases | 61 | 585.4 | 447.1 | < 0.01 |
| Controls | 61 | 302.1 | 138.4 |
p- value < 0.05*, *Chi-Square test
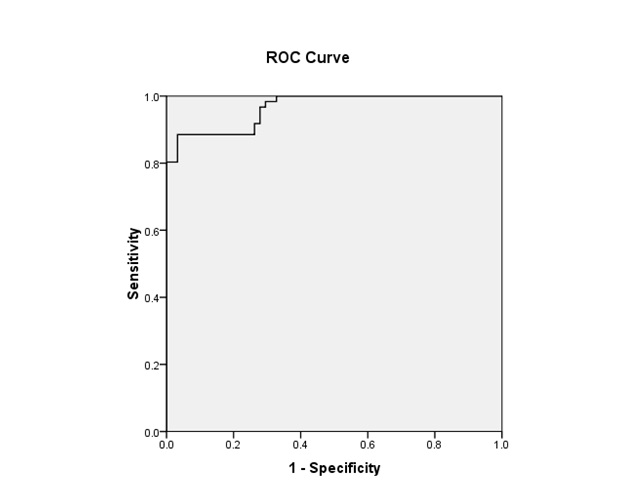
On analysing data with binary logistic regression we found that Vitamin D levels significantly predicts the occurrence of Wheezing (p < 0.05; Odds Ratio - 0.7). Each 10 ng/ml decrease in vitamin D was associated with 7.25% greater odds of current wheeze. Area under ROC curve for vitamin D levels as a test for diagnosing wheezing is 0.965.(p<0.05) Area under ROC curve for vitamin D levels as a test for diagnosing wheezing is 0.965 (p<0.05) [Table-Fig-3]. Area under ROC curve for vitamin D levels as a test for diagnosing wheezing is 0.965. (p<0.05) [Table-Fig-4].
Binary Logistic regression matrix to predict Wheezing with Vitamin D as Dependent variable.
| Binary Logistic Regression | B | S.E. | Wald | Df | p-value | Odds Ratio |
|---|
| Vitamin D Levels | -0.322 | 0.064 | 25.613 | 1 | < 0.05 | 0.725 |
| Constant | 6.955 | 1.481 | 22.048 | 1 | < 0.05 | 1048.504 |
Receiver Operating Characteristic (ROC) Curve for Vitamin D.
[Table-Fig-5] Shows that there was no significant association between severity of vitamin D deficiency levels and frequency of wheezing attacks [Table-Fig-4]. On analysing data with linear regression model, we observed that sun exposure for less than 30 minutes/ week, and delaying of complementary feeding beyond 6 months were significant [Table-Fig-6,7].
Association of Vitamin D levels and wheezing.
| No. of wheezing attacks/ year | Vitamin D levels | Total |
|---|
| < 5 | 5-9.9 | 10-19.9 | 20-29.9 |
|---|
| Three | N | 7 | 12 | 3 | 9 | 31 |
| % | 50.00% | 52.20% | 37.50% | 56.20% | 50.80% |
| Four | N | 4 | 8 | 5 | 7 | 24 |
| % | 28.60% | 34.80% | 62.50% | 43.80% | 39.30% |
| Five | N | 3 | 3 | 0 | 0 | 6 |
| % | 21.40% | 13.00% | 0.00% | 0.00% | 9.80% |
| Total | N | 14 | 23 | 8 | 16 | 61 |
| % | 100.00% | 100.00% | 100.00% | 100.00% | 100.00% |
p- value -0.35*, *Chi-Square test
Linear regression matrix to find predictors of Vitamin D deficiency.
| Variable | Code |
|---|
| Sun Exposure (> 30 minutes/ week) | Yes | 1 |
| No | 0 |
| Exclusive Breast Feeding till 6 months | Yes | 1 |
| No | 0 |
| Complementary Feeding started at 6 months | Yes | 1 |
| No | 0 |
| Variables | Unstandardized Coefficients | Standardized Coefficients | t | p-value |
|---|
| B | Std. Error | Beta |
|---|
| Sun Exposure (> 30 minutes) | 11.791 | 3.125 | 0.468 | 3.773 | < 0.001 |
| Exclusive Breast Feeding till 6 months | 0.601 | 2.84 | 0.024 | 0.212 | 0.833 |
| Complementary Feeding started at 6 months | 9.221 | 3.046 | 0.366 | 3.028 | 0.003 |
a. Dependent Variable: Vitamin D
Discussion
In recent years, vitamin D has been a focus of growing interest in public health nutrition. Studies suggesting prevalence of Vitamin D deficiency in India in Epidemic proportions [35]. The most possible solution seems to be food fortification in Wheat, Curd, Flour ghee etc. Vitamin D deficiency is associated with increased risk of recurrent Wheezing, Vitamin D can significantly predict the occurrence of recurrent wheezing. Each 10ng/ml decrease in Vitamin D level is associated with 7.25% greater odds of wheezing. Considering the deficiency of vitamin D, among cases and controls as per our study, vitamin D supplementation may be considered even in healthy children because children may not have any classical clinical feature of rickets. Sun exposure less than 30 minutes/week is significant predictor of Vitamin D deficiency and is indirectly associated with increased risk of recurrent wheezing.
Laboratory research suggests several potential mechanisms for how vitamin D can affect risk of asthma. Many recent studies of genetic association [18,19,37–39] suggest about relation of polymorphisms of VDR gene to obstructive pulmonary disease.
Very severe Vitamin D deficiency (< 5ng/ml) was observed in 23% of cases while none had vitamin D levels above 30 ng/ml [Table/Fig-1]. Data was statistically significant (p<0.05). Optimum levels were observed in 44.3% of controls while none had levels below 10 ng/ml. [Table/Fig-1]. Mean Vitamin D level was significantly lower in cases compared to controls (11.6 vs. 31 ng/ml). On analysing data with binary logistic regression we also found that Vitamin D levels can significantly predicts the occurrence of Wheezing in children (Odds Ratio - 0.7, AROC – 0.96) [Table/Fig-3&5] & [Table/Fig-4] ROC. Each 10 ng/ml decrease in vitamin D was associated with 7.25% greater odds of current wheeze.
In studies [9,23] higher maternal intake of Vitamin D was linked to a reduced frequency of wheezing in early childhood. Elsewhere it was concluded that cord-blood levels of 25 (OH) vitamin D had inverse associations with risk of respiratory infection and childhood wheezing [6]
Similarly Keet et al., concluded, each 10 ng/mL decrease in vitamin D was associated with a 26% greater odds (OR: 1.26 {95% CI: 1.09–1.46}) of current wheeze [40].
In a study Graham D et al., selected subjects from a birth cohort recruited in utero with the primary objective of identifying associations between maternal diet during pregnancy and asthma and allergies in children. They concluded that increasing maternal vitamin D intakes during pregnancy may decrease the risk of wheeze symptoms in early childhood [22].
S. Calcium levels in cases and controls were 8.9 and 9.2 mg/dl (p< 0.05) [Table/Fig-2]. Alkaline Phosphate levels were significantly higher in cases than controls (585.4 vs. 302.1 IU/L) (p<0.01). [Table/Fig-2]. The results can be explained on the basis of various studies showing direct positive co-relation of vitamin D levels with Calcium [41–43] and its negative co-relation with alkaline phosphatase levels [44–46].
In [Table/Fig-6,7], we also observed that sun exposure for less than 30 minutes/week, and delaying of complementary feeding beyond 6 months were significant predictors of vitamin D deficiency (p< 0.01).
Limitations
Small sample size and no IgE level estimation.
Recommendations
Massive health education campaigns are needed to guide women about importance of proper nutrition during pregnancy and adequate sunlight exposure. Measurement of Vitamin D level should be included in the workup of recurrent wheezing children. But a larger study is needed for more confirmation as the test is very costly. There is also need to develop recommendations for vitamin D supplementation for pregnant and lactating women also; this is another possible strategy for improving vitamin D status.
Conclusion
We conclude that exclusive breast feeding and delaying of complementary feeding beyond 6 months of age are significant predictors of Vitamin D deficiency and have indirect association with increased incidence of wheezing in children.
Funding Agency: Grants from ICMR were used and Facilities in terms of equipment’s etc. were available at the institution.
p- value < 0.05*, *Chi-Square test
p- value < 0.05*, *Chi-Square test
p- value -0.35*, *Chi-Square test
a. Dependent Variable: Vitamin D
[1]. Martinez FD, Wright AL, Taussig LM, Holberg CJ, Halonen M, Morgan WJ, Asthma and wheezing in the first six years of life. The Group Health Medical AssociatesThe New England journal of medicine 1995 332(3):133-38. [Google Scholar]
[2]. Bisgaard H, Szefler S, Prevalence of asthma-like symptoms in young childrenPaediatric pulmonology 2007 42(8):723-28. [Google Scholar]
[3]. Taussig LM, Wright AL, Holberg CJ, Halonen M, Morgan WJ, Martinez FD, Tucson Children’s Respiratory Study: 1980 to presentThe Journal of allergy and clinical immunology 2003 111(4):661-75.quiz 76 [Google Scholar]
[4]. Chipps BE, Bacharier LB, Harder JM, Phenotypic expressions of childhood wheezing and asthma: implications for therapyThe Journal of paediatrics 2011 158(6):878-84 e1. [Google Scholar]
[5]. Elphick HE, Sherlock P, Foxall G, Simpson EJ, Shiell NA, Primhak RA, Survey of respiratory sounds in infantsArchives of disease in childhood 2001 84(1):35-39. [Google Scholar]
[6]. Camargo CA, Jr, Ingham T, Wickens K, Thadhani R, Silvers KM, Epton MJ, Cord-blood 25-hydroxyvitamin D levels and risk of respiratory infection, wheezing, and asthmaPaediatrics 2011 127(1):e180-87. [Google Scholar]
[7]. Wayse V, Yousafzai A, Mogale K, Filteau S, Association of subclinical vitamin D deficiency with severe acute lower respiratory infection in Indian children under 5 yEur J Clin Nutr 2004 58(4):563-67. [Google Scholar]
[8]. Camargo CA, Jr, Rifas-Shiman SL, Litonjua AA, Rich-Edwards JW, Weiss ST, Gold DR, Maternal intake of vitamin D during pregnancy and risk of recurrent wheeze in children at 3 y of ageThe American journal of clinical nutrition 2007 85(3):788-95. [Google Scholar]
[9]. Linday LA, Shindledecker RD, Tapia-Mendoza J, Dolitsky JN, Effect of daily cod liver oil and a multivitamin-mineral supplement with selenium on upper respiratory tract paediatric visits by young, inner-city, Latino children: randomized paediatric sitesThe Annals of otology, rhinology, and laryngology 2004 113(11):891-901. [Google Scholar]
[10]. Urashima M, Segawa T, Okazaki M, Kurihara M, Wada Y, Ida H, Randomized trial of vitamin D supplementation to prevent seasonal influenza A in school childrenThe American journal of clinical nutrition 2010 91(5):1255-60. [Google Scholar]
[11]. Awasthi S, Kalra E, Roy S, Awasthi S, Prevalence and risk factors of asthma and wheeze in school-going children in Lucknow, North IndiaIndian paediatrics 2004 41(12):1205-10. [Google Scholar]
[12]. Burris HH, Marter LJ, McElrath TF, Vitamin D status among preterm and full-term infants at birthPaediatr Res 2013 75:75-80. [Google Scholar]
[13]. Camargo CA, Jr, Ingham T, Wickens K, Thadhani RI, Silvers KM, Epton MJ, Vitamin D status of newborns in New ZealandThe British journal of nutrition 2010 104(7):1051-57. [Google Scholar]
[14]. Kimberly DW, Denise MG, Wheezing in Infants: Bronchiolitis. In: Kliegman RM, Stanton BF, Geme JW, Schor NF, Behrman RE, editorsNelson Textbook of Paediatrics 2011 219 edPhiladelphiaElsvier:1456-57. [Google Scholar]
[15]. Heymann PW, Carper HT, Murphy DD, Platts-Mills TA, Patrie J, McLaughlin AP, Viral infections in relation to age, atopy, and season of admission among children hospitalized for wheezingThe Journal of allergy and clinical immunology 2004 114(2):239-47. [Google Scholar]
[16]. Carroll KN, Wu P, Gebretsadik T, Griffin MR, Dupont WD, Mitchel EF, The severity dependent relationship of infant bronchiolitis on the risk and morbidity of early childhood asthmaThe Journal of allergy and clinical immunology 2009 123(5):1055-61.:61 e1 [Google Scholar]
[17]. Mansbach JM, Camargo CA, Bronchiolitis: lingering questions about its definition and the potential role of vitamin DPaediatrics 2008 122(1):177-79. [Google Scholar]
[18]. Poon AH, Laprise C, Lemire M, Montpetit A, Sinnett D, Schurr E, Association of vitamin D receptor genetic variants with susceptibility to asthma and atopyAmerican journal of respiratory and critical care medicine 2004 170(9):967-73. [Google Scholar]
[19]. Raby BA, Lazarus R, Silverman EK, Lake S, Lange C, Wjst M, Association of vitamin D receptor gene polymorphisms with childhood and adult asthmaAmerican journal of respiratory and critical care medicine 2004 170(10):1057-65. [Google Scholar]
[20]. Burns J, Dockery D, FE. S, Low levels of dietary vitamin D intake and pulmonary function in adolescentsProceedings American Thoracic Society 2006 :526-27. [Google Scholar]
[21]. Black PN, Scragg R, Relationship between serum 25-hydroxyvitamin d and pulmonary function in the third national health and nutrition examination surveyChest 2005 128(6):3792-98. [Google Scholar]
[22]. Devereux G, Litonjua AA, Turner SW, Craig LC, McNeill G, Martindale S, Maternal vitamin D intake during pregnancy and early childhood wheezingThe American journal of clinical nutrition 2007 85(3):853-59. [Google Scholar]
[23]. Long-term effects of budesonide or nedocromil in children with asthma. The Childhood Asthma Management Program Research GroupThe New England journal of medicine 2000 343(15):1054-63. [Google Scholar]
[24]. Litonjua AA, Weiss ST, Is vitamin D deficiency to blame for the asthma epidemic?The Journal of allergy and clinical immunology 2007 120(5):1031-35. [Google Scholar]
[25]. Underwood JL, DeLuca HF, Vitamin D is not directly necessary for bone growth and mineralizationThe American journal of physiology 1984 246(6 Pt 1):E493-98. [Google Scholar]
[26]. Chiba Y, Misawa M, The role of RhoA-mediated Ca2+ sensitization of bronchial smooth muscle contraction in airway hyperresponsivenessJournal of smooth muscle research = Nihon Heikatsukin Gakkai kikanshi 2004 40(4-5):155-67. [Google Scholar]
[27]. Lee CG, Link H, Baluk P, Homer RJ, Chapoval S, Bhandari V, Vascular endothelial growth factor (VEGF) induces remodeling and enhances TH2-mediated sensitization and inflammation in the lungNature medicine 2004 10(10):1095-103. [Google Scholar]
[28]. Kuhn C, 3rd, Homer RJ, Zhu Z, Ward N, Flavell RA, Geba GP, Airway hyperresponsiveness and airway obstruction in transgenic mice. Morphologic correlates in mice overexpressing interleukin (IL)-11 and IL-6 in the lungAmerican journal of respiratory cell and molecular biology 2000 22(3):289-95. [Google Scholar]
[29]. Sakai T, Larsen M, Yamada KM, Fibronectin requirement in branching morphogenesisNature 2003 423(6942):876-81. [Google Scholar]
[30]. Hochscheid R, Jaques G, Wegmann B, Transfection of human insulin-like growth factor binding protein 3 gene inhibits cell growth and tumorigenicity: a cell culture model for lung cancerJ Endocrinol 2000 166(3):553-63. [Google Scholar]
[31]. Broxmeyer HE, Cooper S, Kohli L, Hangoc G, Lee Y, Mantel C, Transgenic expression of stromal cell-derived factor-1/CXC chemokine ligand 12 enhances myeloid progenitor cell survival/antiapoptosis in vitro in response to growth factor withdrawal and enhances myelopoiesis in vivoJournal of immunology 2003 170(1):421-29. [Google Scholar]
[32]. Harinarayan CV, Prevalence of vitamin D insufficiency in postmenopausal south Indian womenOsteoporos Int 2005 16(4):397-402. [Google Scholar]
[33]. Harinarayan CV, Joshi SR, Vitamin D status in India—its implications and remedial measuresThe Journal of the Association of Physicians of India 2009 57:40-48. [Google Scholar]
[34]. Marwaha RK, Sripathy G, Vitamin D & bone mineral density of healthy school children in northern IndiaThe Indian journal of medical research 2008 127(3):239-44. [Google Scholar]
[35]. Ritu G, Gupta A, Vitamin D deficiency in India: Prevalence, causalities and interventionsNutrients 2014 6:729-75. [Google Scholar]
[36]. Stroud ML, Stilgoe S, Stott VE, Alhabian O, Salman K, Vitamin D - a reviewAustralian family physician 2008 37(12):1002-05. [Google Scholar]
[37]. Afzal S, Lange P, Bojesen SE, Freiberg JJ, Nordestgaard BG, Plasma 25-hydroxyvitamin D, lung function and risk of chronic obstructive pulmonary diseaseThorax 2014 69:24-31.doi: 10.1136/thoraxjnl-2013-203682 [Google Scholar]
[38]. Persson LJ, Aanerud M, Hiemstra PS, Vitamin D, vitamin D binding protein, and longitudinal outcomes in COPDPLoS One 2015 10:e0121622 [Google Scholar]
[39]. Liu X, Nelson A, Wang X, Vitamin D modulates prostaglandin E2 synthesis and degradation in human lung fibroblastsAm J Respir Cell Mol Biol 2014 50:40-50. [Google Scholar]
[40]. Keet CA, McCormack MC, Peng RD, Matsui EC, Age- and atopy-dependent effects of vitamin D on wheeze and asthmaThe Journal of allergy and clinical immunology 2011 128(2):414-16 e5. [Google Scholar]
[41]. Tsang RC, Donovan EF, Steichen JJ, Calcium physiology and pathology in the neonatePaediatric clinics of North America 1976 23(4):611-26. [Google Scholar]
[42]. Massry SG, Friedler RM, Coburn JW, Excretion of phosphate and calcium: Physiology of their renal handling and relation to clinical medicineArchives of internal medicine 1973 131(6):828-59. [Google Scholar]
[43]. Steingrimsdottir L, Gunnarsson O, Indridason OS, Franzson L, Sigurdsson G, Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intakeJAMA 2005 294(18):2336-41. [Google Scholar]
[44]. Lips P, Duong T, Oleksik A, Black D, Cummings S, Cox D, A global study of vitamin D status and parathyroid function in postmenopausal women with osteoporosis: baseline data from the multiple outcomes of raloxifene evaluation clinical trialThe Journal of clinical endocrinology and metabolism 2001 86(3):1212-21. [Google Scholar]
[45]. Haussler MR, Nagode LA, Rasmussen H, Induction of Intestinal Brush Border Alkaline Phosphatase by Vitamin D and Identity with Ca-ATPaseNature 1970 228(5277):1199-201. [Google Scholar]
[46]. Manolagas SC, Burton DW, Deftos LJ, 1,25-Dihydroxyvitamin D3 stimulates the alkaline phosphatase activity of osteoblast-like cellsThe Journal of biological chemistry 1981 256(14):7115-17. [Google Scholar]