Congenital Atresia of Wharton’s Duct
Anne Hseu1, Premchand Anne2, Samantha Anne3
1 Associate in Otolaryngology, Instructor, Harvard Medical School, Boston Children’s Hospital, Boston, Massachusetts1, St. John Providence Children’s Hospital, Detroit, MI2 and Cleveland Clinic, Head and Neck Institute, Cleveland, Ohio3.
2 Assistant Professor, Department of Pediatrics, Wayne State School of Medicine, St John Providence, Children’s Hospital, MI2 and Cleveland Clinic, Head and Neck Institute, Cleveland, Ohio3.
3 Assistant Professor, Department of Surgery, Pediatric Otolaryngology, Cleveland Clinic, Boston Children’s Hospital, Boston, Massachusetts1, St. John Providence Children’s Hospital, Detroit, MI2 and Cleveland Clinic, Head and Neck Institute, Cleveland, Ohio3.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Samantha Anne, Desk A71, Cleveland Clinic, 9500 Euclid Avenue, Cleveland, OH 44195.
E-mail: annes@ccf.org
This is a case report of a three-month-old male who presented to clinic with a cystic lesion under the tongue. On clinical examination, a cystic lesion was observed in the, floor-of-mouth. The patient was referred to Paediatric Otorhinolaryngology service for further management. The differential diagnoses for floor-of-mouth lesions should be reviewed with primary focus on the Wharton’s duct atresia and its management. It is crucial to recognize submandibular duct atresia in the primary Paediatric clinic in order to expedite management of lesion before complications arise including infection, enlargement of cyst, and feeding and breathing difficulties.
Cystic lesions, Submandibular duct atresia
Case Report
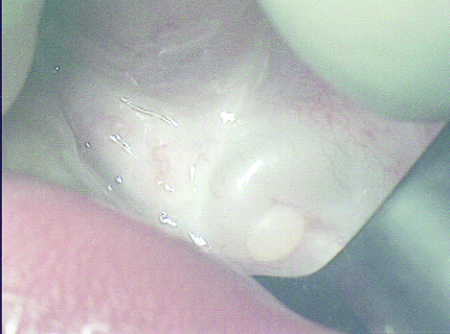
A three-month-old infant presented with left-sided floor of mouth (FOM) cyst, first noted by parents as a lesion under the tongue at two months of age. The oral mucosa did not appear dry and the child had no breathing difficulty. According to the parents, there was no associated bleeding. The child was feeding without difficulty. On clinical examination, he had a left FOM fluid-filled, 0.5 centimeter by 1 centimeter, mass, with a blind ending duct with a fibrotic plug at the oral mucosa [Table/Fig-1]. Further imaging with Computed Tomography (CT) would expose infant to radiation and Magnetic Resonance Imaging (MRI) and may require sedation. Ultrasound in this location is difficult because of intraoral location and small oral cavity. In addition, because the diagnosis was clinically apparent, decision was made to forego further imaging studies.
Plug of fibrotic tissue seen at the distal end of Wharton’s duct.
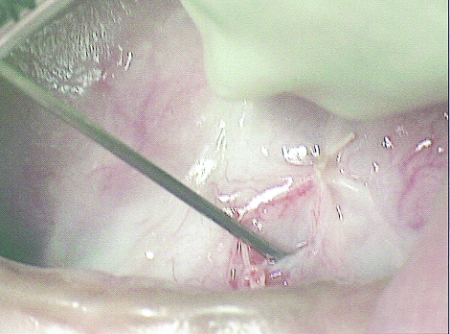
The risks of observation, including infection, further growth of lesion with feeding and breathing difficulties, and low chance of self-resolution, were discussed with parents. After consideration of risks, parents made the decision to proceed with surgery. Patient was positioned supine on the operating table. General anesthesia was instituted and patient was orally intubated successfully. A mouth gag was placed. An elliptical incision was made along the fibrotic plug at the distal end of the submandibular duct and it was excised. Lacrimal probe was then passed along the duct and the incision was extended linearly along the duct overlying the probe which insured the incision was placed overlying duct. A copious amount of white drainage was suctioned out from the lesion after incision. The edges of the mucosa of the cyst were then approximated to the lateral floor of mouth mucosa (sialodochoplasty) [Table/Fig-2]. Follow-up at 3 months revealed widely patent duct orifice with no recurrence of cyst. He had free flow of saliva through the orifice. No recurrence was noted over four-year follow-up period with his primary care physician.
Lacrimal probe passed through new ductal opening.
Discussion
Infants often present to Paediatricians with cystic lesions in the floor of mouth. Very often, these lesions are benign and secondary to plugged or ruptured minor salivary gland ducts and develop into small mucoceles or mucus retention cysts. These lesions often undergo self-resolution. However, concern arises when these cystic lesions persist or enlarge in size. The differential diagnoses include dermoid cysts, teratomas, ranulas, lymphatic malformations, and branchial anomalies [1].
Congenital atresia of the Wharton’s (submandibular) duct is a rare entity with less than 30 cases reported in literature since the 1950s [2,3] and can present as a floor of mouth cystic lesion in an infant. One of the earliest reported cases of atresia was in 1955 [4]. Since then, there have been several other reports of both unilateral and bilateral cases of duct atresia [5,6]. A literature review done by Rosow et al., revealed total of 28 cases with 2 more cases reported since that study was published [2]. In this review, mean age of patients at treatment was 4.4 months (excluding an outlier patient at 15 years) and there was male preponderance. These patients underwent observation to complete excision of cyst with no recurrences. The authors recommend simple sialodochostomy as a management option for these patients. The submandibular gland forms between weeks ten and twelve in an embryo. Development begins as a thickening of epithelium that protrudes into underlying mesenchyme. As the epithelium invaginates, the main salivary duct is formed which links the epithelial bud to the oral surface. The bud goes on to produce further branches and buds to create a multi-lobed gland. The solid epithelium then undergoes cavitation for duct production. This allows proper flow between the saliva-producing acini and the oral cavity [3]. Although the aetiology of submandibular duct atresia is presently unknown, it likely can be attributed to failure of the epithelium to properly canalize. The lesion is often under-recognized and under-diagnosed. These lesions are usually benign; however, as they grow gradually, they can pose problems with feeding in infants due to tongue displacement posteriorly, making it difficult to breathe and/or swallow. In addition, if untreated, the lesions can cause sialoadenitis from salivary retention and gland atrophy from chronic disuse. It is crucial to differentiate these cysts, which require surgical procedures with attendant increased morbidity, from mucoceles or mucus retention cysts that often resolve with observation. With the correct diagnosis, surgery can be limited to sialodochoplasty or sialodochostomy as options resulting in little morbidity and rapid recovery. This case report highlights the need to recognize and distinguish the lesions from simple mucoceles or mucus retention cysts. With early diagnosis and prompt surgery, infant in this case report had unremarkable recovery and growth on follow up.
Conclusion
Congenital atresia of the submandibular duct is a rare entity. Diagnosis should be considered when a baby presents with FOM cystic lesion. Simple sialodochoplasty or sialodochostomy is often curative.
[1]. Chapter 1, Developmental Defects of the Oral and Maxillofacial Region, Pages 30-35, in Oral and Maxillofacial Pathology. Brad W. Neville, Angela C. Chi, Douglas D. Damm, Carl M. Allen, Elsevier Health Sciences, May 13, 2015 [Google Scholar]
[2]. Rosow DE, Ward RF, April MF, Sialodochostomy as treatment for imperforate submandibular duct: A systematic literature review and report of two casesInternational Journal of Paediatric Otorhinolaryngology 2009 73:1613-15. [Google Scholar]
[3]. Calzada GG, Hanna EY, Benign neoplasms of salivary glands. In: Flint PW, Haughey BH, et la., edsCummings Otolaryngology Head & Neck Surgery87PhiladelphiaMosby Elsevier:1162-1177. [Google Scholar]
[4]. Scher LB, Scher I, Case of imperforate submandibular ducts in an infantBr Dent J 1955 98:324 [Google Scholar]
[5]. Aronovich S, Edwards SP, A Case of Imperforate Wharton DuctJournal of Oral and Maxillofacial Surgery 2014 72(4):744-47. [Google Scholar]
[6]. Pownell PH, Brown OE, Pransky SM, Manning S, Congenital abnormalities of the submandibular ductInternational Journal of Paediatric Otorhinolaryngology 1992 24(2):161-69. [Google Scholar]