Japanese Encephalitis (JE), caused by Japanese encephalitis virus (JEV), a flavi-virus, is the most significant aetiology of arboviral encephalitis worldwide. It has resulted in epidemics of encephalitis in the Indian subcontinent. Here, we report a case of 36-year-old female who presented with a short history of fever and headache followed by altered sensorium. Funduscopic examination revealed Papilloedema. Pyogenic or viral meningoencephalitis along with complicated malaria were kept as initial differential diagnosis. Magnetic Resonance Imaging (MRI) of brain revealed involvement of posterior limb of internal capsule and bilateral thalami in the form of haemorrhagic encephalitis along with obstructive hydrocephalus. Cerebro Spinal Fluid (CSF) serology (IgM ELISA) showed JE as the causative agent. Despite extensive literature search, we could not find a case of JE reported with hydrocephalus as a complication. This case highlights the typical and atypical features of JE including imaging findings and exemplifies the way, how diversely JE can present and would thus help in preparing management paradigms accordingly.
Culex, Elevated intracranial pressure, Flavivirus, Haemorrhagic encephalitis, Herniation syndromes
Case Report
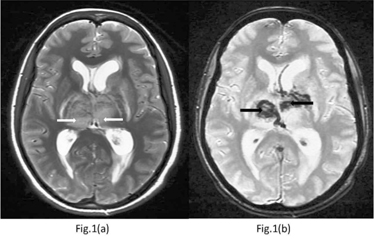
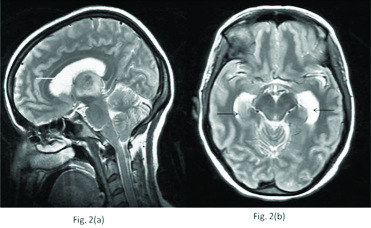
A 36-year-old female patient presented to the medicine emergency with chief complaints of low grade fever (99° F) with headache since 7 days followed by projectile vomiting with impaired consciousness since 5 days. There was no history of seizures, ear discharge or head trauma. There was no history of tuberculosis, intravenous drug abuse, sexual promiscuity or any other contributory illness in the past. On examination, she had impaired consciousness with score on Glasgow coma scale (GCS) being (9/15). Her axillary temperature was recorded to be 99.8° F. However, pulse and blood pressure were normal. Her pupils were bilaterally normal in size and reaction. She had asymmetric cogwheel rigidity, more in the left side extremities. Plantar reflex was bilaterally equivocal and terminal neck rigidity was present. Fundus examination revealed bilateral papilloedema. Blood investigations revealed serum Haemoglobin (Hb) level to be 10.7 g% with total leukocyte count(TLC) and platelet count to be 10,200/mm3 and 2,06,000/mm3, respectively. Based on history and physical examination, patient was initially treated empirically on the lines of meningoencephalitis (pyogenic/viral) and complicated malaria. However, further investigations showed malarial antigen to be negative and Magnetic Resonance Imaging (MRI) of brain revealed diffuse swelling and altered signal intensity in bilateral thalami and posterior limb of internal capsule, appearing hypointense on T1W and hyperintense on T2W and FLAIR images with blooming on gradient echo (GRE) sequence [Table/Fig-1]. Besides, third ventricle was effaced with dilated lateral ventricles [Table/Fig-2] and periventricular ooze. Fourth ventricle appeared normal. These findings were indicative of acute obstructive hydrocephalus.
T2W sequence of MRI brain: (a) shows hyperintensities in bilateral thalami {white thick arrows} with (b) blooming on gradient echo(GRE) sequence; {black thick arrows}, thus confirming the haemorrhagic lesions.
T2W sequence of MRI brain: (a) shows effacement of third ventricle {white thin arrow} and (b) enlargement of temporal horns of lateral ventricles; {black thin arrows}.
In view of clinical and radiological clues diagnostic possibility of haemorrhagic encephalitis with acute obstructive hydrocephalus was considered. Though extensive thalamic haemorrhage is not a feature of tuberculosis, in view of hydrocephalus and with high incidence of tuberculosis in the region, tuberculous aetiology was also considered.
A guarded lumbar puncture was done after administration of intracranial pressure lowering agent and clear cerebrospinal fluid (CSF) was obtained. Serology for encephalitic viruses was ordered both in serum and CSF. CSF examination revealed a protein of 8.9 mg/dl and sugar of 78 mg/dl. A total of 10 cells/cu mm were seen out of which 90% were lymphocytes. CSF PCR for tuberculosis was negative and CSF Adenosine Deaminase (ADA) level was not raised. IgM ELISA (Enzyme linked immunosorbent assay) for JE was positive in both, serum and CSF. Patient was managed conservatively with supportive measures.
She regained consciousness after 10 days of hospital stay and was discharged in a stable condition after 28 days. She had mild asymmetric cogwheel rigidity persisting in left side extremities at the time of discharge, as the only neurological deficit.
Discussion
JE occurs in nearly all countries of Asia. Annually, approximately 50,000 cases of JE are reported from Asian countries principally from China, South East Asia and India [1]. In most areas transmission is endemic with annual fluctuations in the number of cases depending on environmental factors. As with other flavivirus infections, a high subclinical to clinical infection ratio is usual, values often ranging from 25:1 to 1,000:1 [2]. Exposure to JE virus occurs in childhood and antibody prevalence rates approach 80% by early adulthood. A vietnamese study of patients hospitalized with ‘acute encephalitis syndrome’ showed that only 6% of adults against 67% of pediatric patients had JE [3]. In developed countries, where there are long-standing, high-quality childhood vaccination programmes, JE is usually a rare disease of non-immune adults, especially the elderly [4].
Besides, in most areas, a slight excess of male cases (1.5:1) has been observed [5]. The age-related risk for acquiring JE is bimodal with highest age-specific risk occurring in children and in the elderly, though in our case the patient was a middle aged (35-year-old) female. Transmission is usually by the bites of infected culicine mosquitoes (mostly by culex tritaeniorhynchus) that use ground pools and especially rice paddies for their larval stages in the late summer [6].
Pathological changes are distributed principally in the thalamus, brainstem, substantia nigra, hippocampus, temporal cortex, cerebellum and spinal cord. Histopathological changes involve focal neuronal degeneration, diffuse and focal microglial proliferation and perivascular cuffing [7,8].
A prodromal illness of fever, headache, letharginess, nausea, and vomiting lasting several days precedes the onset of neurological signs. The central feature is an altered state of consciousness, ranging from mild mental clouding to drowsiness and stupor with or without signs of meningeal irritation. Some children exhibit personality changes, slurred speech and mutism [9]. Patients frequently have rigidity, tremors and involuntary movements as manifestations of extrapyramidal involvement. Assymetric extrapyramidal involvement along with altered sensorium was evident in this case. Disconjugate gaze with facial and other cranial nerve palsies are found in about one-third of patients. Papilloedema is seen in fewer than 10% of patients and rarely, is associated with hypertension and other physiological reflexes reflecting elevated intracranial pressure [10].
The serum sodium level often is depressed due to inappropriate Antidiuretic Hormone (ADH) secretion. The CSF typically is clear, under normal pressure and with normal or mildly elevated protein and normal glucose concentrations, as was seen in this case. A pleocytosis of 10 to several hundred white cells is typical in the first week of illness and the cell count may remain elevated until the third week. The MR imaging findings of JE have been described as bilateral thalamic, substantia nigra, basal ganglia, brainstem, cerebellum, cerebral cortical and white matter lesions [11–13].
Bilateral T2 hyperintense and T1 hypointense to isointense thalamic lesions especially haemorrhagic, have been described as characteristic of the disease in an appropriate clinical setting [12]. In this case, there were extensive haemorrhagic lesions of thalamus compressing the adjacent third ventricle and hence creating acute obstructive hydrocephalus, thus resulting in dilatation of lateral ventricles and periventricular ooze. Obstructive hydrocephalus has been reported previously in viral encephalitis, especially in HSV encephalitis. Tyagi et al., reported the case of a child who presented with obstructive hydrocephalus due to aqueductal obstruction following neonatal herpes simplex virus type 1 encephalitis and was treated by repeated third ventriculostomy [14]. Heppner et al., reported another case of a 34-year-old woman who presented with hydrocephalus secondary to isolated HSV type II meningitis who was managed conservatively [15]. Although increased intracranial pressure and brainstem signs compatible with herniation syndromes has been described earlier in JE [16], however, after extensive search of literature it was found that hydrocephalus has not been reported with these typical findings of JE previously.
The standard laboratory diagnostic method is serology by IgM capture ELISA, which has a sensitivity approaching 100% when both CSF and serum samples are tested and samples obtained 1 to 2 weeks after onset are used [17].
CSF is the preferred sample for diagnosis of JE because if anti JE IgM is detected in the CSF, this confirms infection of the central nervous system with JEV, however in our case it was positive in both CSF and serum.
No specific antiviral therapy is currently available and patients are kept only on supportive measures and symptomatic management. Acute obstructive hydrocephalus, as seen in our case, may sometimes be life threatening and should be managed by measures to reduce intracranial pressure including medical and surgical management, as necessary. Development of acute obstructive hydrocephalus should be taken as a red flag sign and the treating physicians should remain vigilant for potential complications that may arise due to obstructive hydrocephalus, like brainstem herniation. Patient should be kept under intensive neurocritical monitoring, so that timely management of complications can be ensured.
Conclusion
The clinical manifestations of Japanese encephalitis are non-specific barring few signs which point towards the diagnosis. So, this disorder is prone to be missed initially. The positive serology for JE virus IgM antibody, and especially, increased antibody levels within a short duration, is of great significance to diagnose JE. JE may present with diverse and atypical findings on MRI brain.
We present JE with unusual association of obstructive hydrocephalus, which has not been reported previously. Hence, JE-specific IgM antibody test in the suspicious cases is necessary for early diagnosis and timely treatment of this potentially lethal condition which would thus benefit the patients infected with this disease. Clinicians should also be aware of hydrocephalus and elevated intracranial pressure as a complication in this disease, so as to address it timely to prevent mortality and significant morbidity.
[1]. Petersen L R, Barrett Alan D T, Arthropod-Borne Flaviviruses. In: Richman Douglas D, Whitley Richard J, Hayden Frederick G, editorsClinical Virology 2009 3rd edWashington, DCASM Press [Google Scholar]
[2]. Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Estimated global incidence of Japanese encephalitis: a systematic reviewBull World Health Organ 2011 89:766-74.:774A-774E. [Google Scholar]
[3]. Lowry PW, Truong DH, Hinh LD, Ladinsky JL, Karabatsos N, Cropp CB, Japanese encephalitis among hospitalized pediatric and adult patients with acute encephalitis syndrome in Hanoi, Vietnam 1995Am J Trop Med Hyg 1998 58(3):324-29. [Google Scholar]
[4]. Campbell Grant L, Estimated global incidence of Japanese encephalitis: a systematic reviewBull World Health Organ [online] 2011 89(10):766-74.ISSN 0042-9686 [Google Scholar]
[5]. Kumar R, Mathur A, Kumar A, Sharma S, Saksena PN, Chaturvedi UC, Japanese encephalitis—an important cause of acute childhood encephalopathy in Lucknow, IndiaPostgrad Med J 1988 64:18-22.doi: 10.1136/pgmj.64.747.18 [Google Scholar]
[6]. Zheng Y, Li M, Wang H, Liang G, Japanese encephalitis and Japanese encephalitis virus in mainland ChinaRev Med Virol 2012 22(5):301-22.Epub 2012 Mar 8 [Google Scholar]
[7]. Deubel V, Huerre M, Cathomas G, Drouet MT, Wuscher N, Le Guenno B, Molecular detection and characterization of yellow fever virus in blood and liver specimens of a non-vaccinated fatal human caseJ Med Virol 1997 53(3):212-17. [Google Scholar]
[8]. Johnson RT, Burke DS, Elwell M, Leake CJ, Nisalak A, Hoke CH, Lorsomrudee W, Japanese encephalitis: immunocytochemical studies of viral antigen and inflammatory cells in fatal casesAnn Neurol 1985 18(5):567-73. [Google Scholar]
[9]. Sabchareon A, Yoksan S, Japanese encephalitisAn Trop Paediatr 1998 18:S67-S71. [Google Scholar]
[10]. Mahendra H, Yogesh G, Harish L, Monika K, Kumar S, A Recent Review: Japanese EncephalitisWorld Journal of Pharmacy and Pharmaceutical Sciences 2014 3(3):545-56. [Google Scholar]
[11]. Kalita J, Misra UK, Comparison of CT scan and MRI findings in the diagnosis of Japanese encephalitisJ Neurol Sci 2000 174:3-8. [Google Scholar]
[12]. Kumar S, Misra UK, Kalita J, MRI in Japanese encephalitisNeuroradiology 1997 39:180-84. [Google Scholar]
[13]. Shoji H, Kida H, Hino H, Magnetic resonance imaging findings in Japanese encephalitis. White matter lesionsJ Neuroimaging 1994 4:206-11. [Google Scholar]
[14]. Tyagi A, Chumas P, Ferrie C, Obstructive hydrocephalus following herpes simplex virus type 1 encephalitis treated by repeated third ventriculostomyPediatr Neurosurg 2001 34(5):244-46. [Google Scholar]
[15]. Heppner PA, Schweder PM, Monteith SJ, Law AJ, Acute hydrocephalus secondary to herpes simplex type II meningitisJ Clin Neurosci 2008 15(10):1157-59. [Google Scholar]
[16]. Solomon T, Dung NM, Kneen R, Thao le TT, Gainsborough M, Nisalak A, Seizures and raised intracranial pressure in Vietnamese patients with Japanese encephalitisBrain: a journal of neurology 2002 125(Pt 5):84-93. [Google Scholar]
[17]. Burke DS, Nisalak A, Johnson DE, Scott RM, A prospective study of dengue infections in BangkokAm J Trop Med Hyg 1988 38(1):172-80. [Google Scholar]