Diabetes mellitus (DM) is a growing public health problem worldwide with high levels of morbidity and mortality. Indians lead the world with the greatest number of diabetics (42 million) and it is estimated that this number will swell to 69.9 million by the year 2025 [1]. Uttarakhand is a geographically diverse state comprising of plains as well as hills. Hilly regions are mainly divided into kumaon and Garhwal. Srinagar is the largest city in Garhwal hills. As of 2001 census, Srinagar had a population of 1,50,000. Srinagar is also educational city in Uttarakhand with an average literacy rate of 83% [2]. Srinagar medical college is the first medical college of the state and caters to the population of Srinagar as well as whole of Garhwal hills. As per MHFW-NPCDCS Survey-2010, the prevalance of diabetes was 5.7% in the state of uttarakhand [3]. The disease remains understudied in the Garhwal region of uttarakhand with paucity of literature. After the flash floods in Uttarakhand in 2013, health system was badly affected. Patients with diabetes could not travel to hospitals regularly for follow up as well as for their anti-diabetic medications which are available for free at the government hospitals. American Diabetes association recommends maintaining HbA1C ≤7.0% to prevent microvascular and macrovascular complications [4]. The morbidity and mortality of this disease mainly depend on the acute and chronic complications. These can be prevented by proper glycaemic control which in turn depends on many factors like exercise, diet and medication. Although there are several factors that affect glycaemic control among patients with diabetes, it is known to be improved by adherence to anti-diabetic medications [5]. The treatment utility depends mainly on self care by the patient and medication adherence [6–8]. Non adherence to medication in chronic diseases like diabetes mellitus not only leads to poor clinical outcome but also increase in cost of care [9]. Aim of the study was to organize disease specific (i.e. diabetes) camp in a resource poor setting to assess medication adherence pattern of diabetics to anti-diabetic medication in this region and study the impact of this camp on adherence to medication and glycaemic control in subsequent follow up visits.
Through this study the team involved in diabetic care of the patients was able to interact directly with diabetic patients and their families. The disease specific camp was also more informative for doctors in understanding the problems of diabetics of this region. The study may provide a bird’s-eye view of minimal care provision for diabetics of this region [10]. The results of this study may help in quantifying the need of a ‘diabetes clinic’ in this region and conveying to government officials will be easier with a study in hand.
Nevertheless, the study is an obvious first step in the direction of providing the data on impact of diabetes awareness camps on medication adherence which is an essential part in glycaemic control in type 2 DM, from Garhwal region of Uttarakhand.
Materials and Methods
An interventional cross-sectional study was conducted with the collaboration of the department of medicine, ophthalmology and pharmacology of Veer Chandra Singh Garhwali Government Institute of Medical Science and Research in the month of December’2014 to March’2015. The study was conducted at HNB Base Teaching Hospital, Srikot, Srinagar, Pauri Garhwal, Uttarakhand. The study received approval from the Institutional Ethics Committee, Veer Chandra Singh Garhwali Government Institute of Medical Science and Research. The first diabetes awareness camp was organized on the 2nd Sunday in the month of December 2014. The camp was organized in the hospital on public holiday as this was the only place where organized space was available along with laboratory support. The patients and their families were informed to come for the camp through the support of panchayat heads, ngos and nss students of medical college. The aim of the camp was to interact with diabetic patients and their families and educate them about the timely surveillance procedures that may help in preventing complications related to the disease [11]. During the first camp, Fifty diabetic patients fulfilling the inclusion and exclusion criteria (mentioned below), were enrolled for the study. All the patients and their family members were given an oral presentation on foot care, diet and when to screen themselves for complications and also their doubts regarding the disease were cleared during an interactive session by the physician. The pharmacologist recorded the adherence to anti-diabetic medication using the Girerd scale [12], a preformed questionnaire containing six questions [Table/Fig-1] on the first day of camp and after three months i.e. 3rd Sunday of March. During the first day of camp, emphasis was laid on explaining the importance of medication adherence to each patient individually by the pharmacologist. The patients were screened for microvascular complications like retinopathy by the ophthalmologist and for neuropathy by physician. The patients were advised to come for follow-ups on 2nd Saturday every month for two months. The blood samples were taken for measuring the HbA1C during the first day of camp and after three months i.e. 3rd Sunday of March.
Measure of medication adherence (Adapted from Girerd et al., [8]).
| S.No. | Questions | YES | NO |
|---|
| 1. | Do you sometimes forget to take your medicine? | | |
| 2. | Have you ever run out of your medicine? | | |
| 3. | Do you sometimes take your medicine late? | | |
| 4. | Do you sometimes decide not to take your medicine because someday you feel that your treatment do more harm than good? | | |
| 5. | Do you think that you have too many pills to take? | | |
| 6. | When you feel better, do you sometimes stop taking your medicine? | | |
| When “No” was answered to 6 items kappa = 0.65 (Good Adherence); When 1 or 2 “yes” were given kappa = 0.5 (Medium Adherence); when 3 or more “yes” were given kappa = 0.56 (Poor adherence) |
Inclusion criteria
Men and women having type 2 DM on oral hypoglycaemic agents.
Age group- 25-80 years.
All patients who could understand Hindi.
All patients who were available for follow-up for 3 months, in Base Hospital, Srinagar, Uttarakhand.
Exclusion criteria
Patients with type 1 DM.
Patients using insulin.
Patients not being able to come for successive follow-ups.
Clinical evaluation
Patients’ weight and height were measured and used to calculate the Body Mass Index (BMI) as a ratio of weight in kilograms/height in meters squared [13]. Peripheral neuropathy was assessed by 5.07/10g- Semmens Weinstein monofilament testing and classified as either significant neuropathy or normal perception [14]. Participant’s mean blood pressure was recorded during evaluation and hypertension defined according to Joint National Committee (JNC 7) [15]. The survey included the Girerd scale 6-item adherence measure [12] designed to evaluate medication adherence in patients with hypertension, which has been validated and found to be reliable in a variety of medication-adherence studies. HbA1C levels were estimated on the first Sunday of the first and third month of diabetes camps, recorded under the heading of pre and post camp HbA1C respectively. The effect of diabetes camp on adherence to anti-diabetics and HbA1C levels was assessed.
Statistical Analysis
The effect of diabetes camp on adherence to anti-diabetics and HbA1C levels was assessed through the data collected on excel sheet over three months and was analysed by SPSS version 16. The observation was analysed by using paired t-test where the value of p < 0.05 was considered significant.
Informed consent: All the details of the nature and purpose of the study were described in the local language to the patient. An individual who voluntarily gave the informed consent was enrolled in the study.
Results
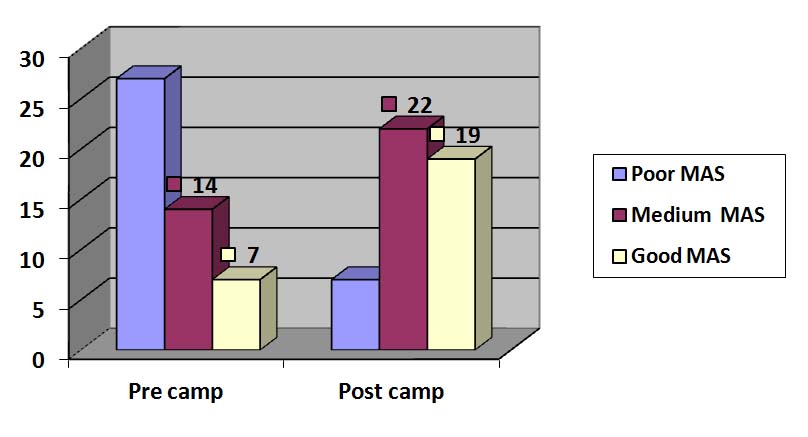
The study included a total of 50 diabetic patients, among them 2 were lost to follow up. The mean age of the patients was 57.43 years. Among these 52.1% were males and 47.9% were females. Among the participants, 54.16% were literate and 45.83% were illiterate’s. The average duration of diabetes amongst the patients was 7.02 years and half of the patients (52.08%, n=48) were hypertensive (Blood pressure >140/90mmHg), the mean systolic and diastolic blood pressure of the study participants was 139.4 and 82.9 respectively [Table/Fig-2]. A total of 47.92% participants were found to have chronic complications of diabetes, among these, the highest 34.7% had triopathy i.e. retinopathy, nephropathy and neuropathy, and 13.3% were detected to have diabetic retinopathy. Poor medication adherence score was recorded in 27 participants and only 7 participants had good adherence to medication before the camp. After the camp, 19 participants had good adherence and 7 had poor medication adherence scores [Table/Fig-3]. Poor glycaemic control (HbA1C≥7%) was observed in 26 participants who had low medication adherence scores recorded before the camp while good glycaemic control (HbA1C ≤ 7%) was observed in 12 participants with high medication adherence scores [Table/Fig-4]. Average decrease in HbA1C comparing Pre & Post blood HbA1C levels was 0.53 units as depicted in [Table/Fig-2].
Descriptive Statistics of Study Population.
| Variable | N | Mean | Std Deviation |
|---|
| Statistics | Std Error |
|---|
| Age (y) | 48 | 57.4375 | 1.53502 | 10.63496 |
| DODMa (y) | 48 | 7.0125 | .71364 | 4.94427 |
| Systolic BP | 48 | 139.4 | 3.24389 | 22.47433 |
| Diastolic BP | 48 | 82.9167 | 1.52399 | 10.55852 |
| Pre-camp BMI | 48 | 24.2308 | .41420 | 2.86963 |
| Post-camp BMI | 48 | 24.0542 | .35101 | 2.43188 |
| Pre-camp HbA1C | 48 | 8.3979 | .21873 | 1.51538 |
| Post-camp HbA1C | 48 | 7.8687 | .21205 | 1.46914 |
aDODM (Duration of Diabetes mellitus)
Number of patients scoring Pre and post camp medication adherence category based on MAS (Medication adherence score).
The relationship between adherence categories and glycaemic control groups.
| Glycaemic group | Poor Adherence | Medium Adherence | Good Adherence |
|---|
| Good control HbA1C <= 7% | PRE CAMP | 1 | 3 | 4 |
| POST CAMP | 0 | 15 | 12 |
| Poor control HbA1C > 7% | PRE CAMP | 26 | 11 | 3 |
| POST CAMP | 7 | 7 | 7 |
On applying paired t-test, statistically significant (p=0.000) correlation was found between pre and post camp HbA1C values [Table/Fig-5]. Pearson correlation showed statistically significant (p=0.001) correlation between pre camp and post camp HbA1C and BMI of the participants [Table/Fig-6,7]. However there was no significant correlation found between education status and SMBG as shown in [Table/Fig-8].
Paired samples correlations on comparing pre and post camp mean HbA1C using paired t-test., *p<0.05
| N | Correlation | Sig. |
|---|
| Pair 1 Pre Camp HBA1C & Post Camp HBA1C | 48 | .964 | .000* |
Correlations between Pre Camp HbA1C and BMI.
| | PRE CAMP HBA1C | PRE CAMP BMI |
|---|
| PRE CAMP HBA1C | Pearson Correlation | 1 | .462** |
| Sig. (2-tailed) | | .001 |
| N | 48 | 48 |
| PRE CAMP BMI | Pearson Correlation | .462** | 1 |
| Sig. (2-tailed) | .001 | |
| N | 48 | 48 |
Correlations between Post Camp HbA1C and BMI.
| | POST CAMP HBA1C | POST CAMP BMI |
|---|
| POST CAMP HBA1C | Pearson Correlation | 1 | .477** |
| Sig. (2-tailed) | | .001 |
| N | 48 | 48 |
| POST CAMP BMI | Pearson Correlation | .477** | 1 |
| Sig. (2-tailed) | .001 | |
| N | 48 | 48 |
**. Correlation is significant at the 0.01 level (2-tailed).
Cross tabulation showing education status with SMBG.
| Education Status | SMBG* | Total |
|---|
| No | Yes |
|---|
| Illiterate | 23 | 1 | 24 |
| Literate | 20 | 4 | 24 |
| Total | 43 | 5 | 48 |
*SMBG (Self Monitoring of Blood Glucose)
Discussion
The organization of diabetes camps had significant impact over medication adherence and glycaemic control. Mean HbA1C values recorded during the first camp and three months latter in the second camp were 8.39 and 7.86 respectively.
During the first camp, 83% of participants had poor glycaemic control (HbA1C>7) and during the second camp, 43.75% participants had poor control and 56.2% had good glycaemic control. The study by Lawrence et al., stated that only 33% of those treated for type 2 diabetes achieved a HbA1C value of less than 7% [16], whereas Indian study gives a higher value of 50-60% patients with diabetes are unable to achieve HbA1C below 7% [17]. Thus, increase in participants with good glycaemic control suggests that interventions like a diabetes awareness camp can play an important role in glycaemic control. The results may be improved further by increasing the frequency of the camps.
Medication adherence score in our study on the 1st camp had Overall 27 participants with poor score which came down to 7 after 2nd camp and regular follow-ups. A similar study was conducted in Tanzania in 2013, on the adherence to diabetes mellitus treatment regimens among Type 2 diabetes patients which showed the prevalence of anti-diabetic drug adherence to be suboptimal [18]. Suboptimal rates of medication adherence have also been reported in studies done in India (a study conducted in the year 1999) [19], Jamaica [20], Uganda [21] and France [22]. The study by Shobhna et al., stressed the need for constant motivation of the patients and education at frequent intervals to improve medication adherence [23]. This makes the utility of awareness camps even more significant which in our study helped in increasing the medication adherence score to optimal levels.
In our study, patients who had good glycaemic control had better adherence to anti-diabetic drugs compared to those who had poor glycaemic control, however, this was not statistically significant. The lack of association between anti-diabetic drug adherence and glycaemic control was also seen in Tanzanian study [18].
On applying paired sample t-test, significant correlation was found between pre and post camp HbA1C [Table/Fig-5]. Mean BMI in our study was in the normal range according to WHO guidelines. Positive correlation was found between HbA1C and BMI both in pre-camp and post camp values [Table/Fig-6,7]. Many studies support the need of improving BMI of diabetic patients which leads to reduction in HbA1C [24]. Study by Gopinath et al., has shown that patients with higher BMI have poor glycaemic control [25]. Thus educating patients and their families about maintaining normal range BMI can help in good glycaemic control.
The awareness camp made its impact on both the age group equally viz. age group equal to 60 years and less (n=29) and age group > 60 years (n=19) which in fact showed the positive and serious approach to the medication adherence shown by the statistically significant (p=0.000) values. In our study the impact of the camp was noted in the age group of 50-60 years, where they showed good adherence to the medication following the camp and the age group 60-70, showed poor adherence. Although a similar study done in Tanzania, showed drug adherence to be better among patients older than 61 years and poorest among patients in the age group of 41-50 years [18].
Self monitoring of blood glucose in our study was not significantly associated with educational status of the patient. All the subjects who did self monitoring of blood glucose level showed good adherence to the anti-diabetic medications. Thus irrespective of their educational status, diabetics could be encouraged to practice SMBG in our population.
The impact of awareness camp showed positive effect not only on literate group (n=26) but even more in the illiterate group (n=22), thus taking the positive approach towards medication adherence which clearly showed the seriousness about the importance and role of medication adherence in improving the blood sugar control in diabetes mellitus and thus helping in reducing the complications there by prolonging the span with better quality of life. Peripheral neuropathy, Nephropathy and Retinopathy were the complications analysed against anti-diabetic medication adherence. They were found to have no significant association with medications adherence.
Both males (n=25) and females (n=23) responded very well to the medication adherence awareness camp showing the statistically significant (p=0.000) improvement in the behaviour towards medication adherence [Table/Fig-9]. A study conducted in Zimbabwe in the year 2012 showed females to be associated with low diabetes knowledge than males [26]. Thus, our study helped in creating awareness in both the genders equally.
Cross tabulation showing gender wise variation in pre and post camp medication adherence score.
| Gender | Good | Medium | Poor | Total |
|---|
| Male | PRE CAMP | 5 | 9 | 11 | 25 |
| POST CAMP | 12 | 9 | 4 |
| Female | PRE CAMP | 2 | 5 | 16 | 23 |
| POST CAMP | 7 | 13 | 3 |
Good glycaemic control was observed in 34.8% of females and 44% of males after the camp which was only 24% and 13% before the camp among males and females respectively [Table/Fig-10]. Thus males showed a better glycaemic control than female. These results will help us to frame the strategies for future camps, keeping female patients in mind and need for more counseling among females. It also encouraged us to organize more diabetic camps, screen all diabetics for complications and involve medical students in interacting with patients.
Impact of diabetes camp on glycaemic control on various genders.
| Glycaemic group | MALE (%) | FEMALE (%) |
|---|
| Good control HbA1C <= 7% | PRE CAMP | 6(24) | 3(13) |
| POST CAMP | 11(44) | 8(34.8) |
| Poor control HbA1C > 7% | PRE CAMP | 19(76) | 20(86.9) |
| POST CAMP | 14(56) | 15(65.2) |
Limitation
The limitation of this study was the limited sample size and short duration of study. Positive difference that the camp made on the clinical practice was that in a resource poor setting like ours, we can take the help of various specialists under one roof and not only screen the patients for complications, clear their doubts about the disease, but also involve their family members in the diabetic care.
Conclusion
Medication adherence and glycaemic control, are the core factors that need to be addressed in good diabetes care. As per RHS Bulletin, March 2012, M/O Health & F.W., GOI, there is severe shortfall of doctors as well as supportive healthcare staff at the health centers located in hilly regions of Garhwal. This makes the management of chronic diseases like diabetes very challenging. Monthly diabetes camps can aid in providing good and cost effective diabetes care by improving medication adherence, glycaemic control, imparting patient education and early screening of diabetes related complication. Organizing diabetic camps every month can not only help in improving medication adherence and glycaemic control but also reduce cost of care for the patient as well as the state. Through such camps we can reinforce patient education and screen the patients for complications. These camps need to focus more on diabetic’s education and counseling among female and old age diabetics. Such camps can also be a good source of learning for the medical students as well as families of the patients. In a resource poor settings of Garhwal region, where there is lack of specialists and diabetic clinics, monthly diabetic camps can be cost effective and patient friendly solution. Diabetic camps can be a good measure to prevent diabetic complications in resource poor settings till well equipped diabetic clinics become a part of health care system in Garhwal region.
Conflicts of Interest
No conflict of interest to this article was reported.
aDODM (Duration of Diabetes mellitus)
**. Correlation is significant at the 0.01 level (2-tailed).
*SMBG (Self Monitoring of Blood Glucose)