The incidence of surgical emergency in a neonate ranges from 1 to 4 per 100 births [3]. Intestinal obstruction is the most common surgical emergency in neonatal period [3]. Neonatal intestinal obstruction occurs 1 in 1500 live births [4]. Common aetiologies are intestinal atresia, meconium ileus, Hirschsprung disease and malrotation of gut with or without volvulus. Goeller is credited for the first description of an ileal atresia in 1684. The first clinical description of congenital megacolon was presented at the Berlin Society of Paediatrics in 1886 by Hirschsprung. In most recent reports Hirschsprung’s disease accounts for a major proportion of cases of neonatal obstruction. Meconium ileus was first described by Landsteiner in 1905. Not until 1942 was there a single case report in which a patient with severe obstruction from this cause survived [2].
Neonatal intestinal obstruction often manifests itself with a number of cardinal signs including maternal polyhydramnios, bilious emesis, abdominal distention and failure to pass meconium in 24 hours of life. Although, none of these observations are pathognomic of obstruction, all are consistent with an obstructive phenomenon and should be carefully evaluated [2,5]. Jejunal atresia is associated with maternal polyhydramnios in 24% of cases. The prenatal ultrasound examination has identified small bowel obstruction associated with atresia, volvulus and meconium peritonitis [2]. The lesions can then be anticipated and an organised management plan developed for delivery and treatment of neonate.
An accurate history and physical examination corroborated by simple radiological studies usually leads the physician to correct diagnosis. Usually, a plain abdominal radiograph is all that is necessary to make a diagnosis, since gas pattern is distinctive and often will give a clue to site of obstruction. Early diagnosis and treatment leads to better outcome. Failure to recognize neonatal bowel obstruction can result in aspiration of vomit, sepsis, midgut infarction or enterocolitis [6]. Delay in carrying out surgery may result in the loss of large amounts of bowel.
Some factors attributing to the high mortality in developing countries include prematurity, late presentation, associated severe congenital anomalies and complications of surgery as well as lack of intensive care facilities [3,7,8].
The aim of this study was to detect pattern of neonatal intestinal obstruction and to find out problem and outcome of surgical treatment in the Paediatric Surgery Department of a tertiary care centre.
Materials and Methods
This retospective study was conducted at paediatric surgery department in Pt. Bhagwat Dayal Sharma PGIMS, Rohtak over a period of 15 years from June 2000 to May 2015. All the newborns who underwent surgery for neonatal intestinal obstruction were included in the study. Patients who were inoperable due to septic shock, pneumonia, very low birth weight and extreme prematurity were excluded from the study. Anorectal malformation including anal atresia and Congenital hypertrophic pyloric stenosis were also excluded from the study. Data were collected from patients’ hospital records and analysed for age at presentation, sex, gestational age, clinical presentation, diagnosis, surgical procedure performed and their outcome.
A total of 298 neonates with neonatal intestinal obstruction were operated in our department during the study period. All patients were put on intravenous fluids, antibiotics and nasogastric decompression was done. After dehydration and electrolyte imbalance was corrected, all of them had blood investigations, abdominal X-ray, ultrasound and in some cases contrast studies were done. Exploratory laparotomy was done in all the cases and type of surgical intervention was carried as per the cause i.e. resection and anatamosis in jejunoileal atresia, end colostomy in Hirschsprung disease and Ladds procedure in malrotation gut etc. For type 1 duodenal and ileal atresia, duodenoplasty and enteroplasty was done. For Vitellointestinal duct and duplication cyst, resection and end to end anastamosis was done. In postoperative period, patients were managed by nasogastric aspiration, fluids and antibiotics and were discharged after 7-10 days. Histopathologically diagnosis was confirmed. In this study only initial surgical procedure and its outcome was included.
Results
Out of 298 patients, 193 were males and 105 were females. Male female ratio was 1.8:1. Gestational age was variable from 32 to 42 weeks (mean = 37.5 weeks) and birth weight from 1.4 to 3.5 kg (mean =2.25 kg).
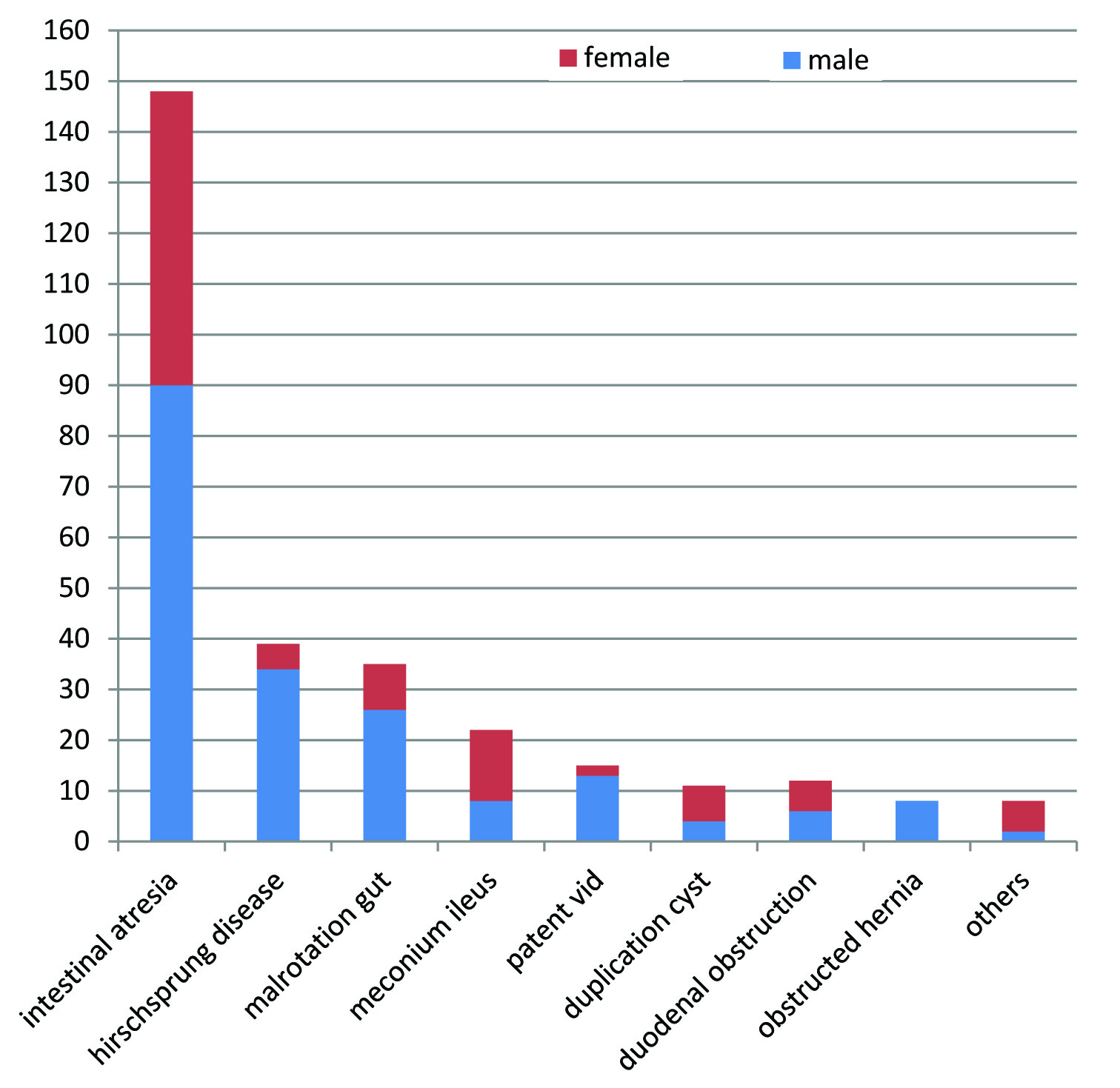
Most common cause of intestinal obstruction was Intestinal atresia followed by Hirschsprung, Malrotation gut and Meconium ileus. In others, there were some rare causes like 3 cases of Band causing obstruction, 3 of Segmental ileal dilatation and 1 case each of Congenital giant chylolymphatic cyst and exomphalos minor with rupture of ileum leading to RamHorn’s intussuception [Table/Fig-1].
Showing aetiological spectrum of Neonatal Intestinal Obstruction.
Ileal atresia (43.2%) was commonest followed by jejunal (31%), duodenal (20.9%) and colonic (4.72%) among intestinal atresia [Table/Fig-2].
Showing distribution of different types of intestinal atresia.
| Type of atresia | 1 | 2 | 3 | 4 | Total |
|---|
| Ileal atresia | 20 | 4 | 36 | 4 | 64 |
| Jejunal atresia | 9 | 2 | 20 | 15 | 46 |
| Duodenal atresia | 12 | 9 | 10 | 0 | 31 |
| Colonic atresia | 1 | 1 | 4 | 1 | 7 |
| Total | | | | | 148 |
Majority of neonates presented within 1st week of life except hirschsprung and malrotation gut in which almost 50% and obstructed hernia in which almost 60% presented later i.e. after 2nd week. Overall mean age of presentation was 6 days [Table/Fig-3,4]
Showing age of presentation in various disease.
| Disease | <7 days | 7-14 days | 14-21 days | 21-28 days | Total (%) |
|---|
| Intestinal atresia | 99 | 28 | 14 | 7 | 148(49.6%) |
| Hirschsprung disease | 12 | 8 | 6 | 13 | 39(13%) |
| Malrotation gut | 15 | 6 | 11 | 3 | 35(11.7%) |
| Meconium ileus | 15 | 3 | 3 | 1 | 22(7.3%) |
| Patent VID | 6 | 6 | 1 | 2 | 15(5%) |
| Duplication cyst | 8 | 2 | 1 | 0 | 11(3.7%) |
| Duodenal obstruction | 9 | 1 | 1 | 1 | 12(4%) |
| Obstructed hernia | 1 | 2 | 2 | 3 | 8(2.7%) |
| Others | 5 | 2 | 1 | 0 | 8(2.7%) |
| Total | 170 | 58 | 40 | 30 | 298(100%) |
Showing clinical features and their relative frequency (298).
| Symptoms | Number of patients (%) |
|---|
| Vomiting | 206 (69%) |
| Abdominal distention | 194 (65%) |
| Visible loops of intestine | 95 (32%) |
| Constipation | 33 (11%) |
All patients with atresias and malrotation gut presented with bilious vomiting except supra ampullary duodenal atresia where it was non bilious. Constipation was mainly present in Hirschsprung disease in which vomiting was a late feature. One patient may have more than one symptom at presentation. Some rare symptoms like palpable mass were seen in duplication cyst and irreducible inguinal swelling was seen in obstructed hernia. Associated anomalies like Down syndrome and cardiac defects were found in 4 cases of duodenal atresia and hydrocephalus was there in 2 cases of Hirschsprung disease.
Out of 298 patients, 249 survived and overall survival rate was 83.6%. Among 49 deaths, highest mortality was observed in intestinal atresia and lowest in Hirschsprung disease. The ultimate cause of death were septicaemia, anastamotic leak and aspiration pneumonia. Preoperative complication like perforation, volvulus and septicaemia were present among those neonates who presented late [Table/Fig-5,6].
Showing outcome of surgical treatment.
| Aetiology | Survived (%) | Died (%) | Total (%) |
|---|
| Intestinal atresia | 116 (78.4%) | 32 (21.6%) | 148(100%) |
| Hirschsprung | 39 (100%) | 0(0%) | 39 (100%) |
| Malrotation gut | 29 (82.9%) | 6 (17.1%) | 35 (100%) |
| Meconium ileus | 18 (81.8%) | 4 (18.2%) | 22 (100%) |
| Patent VID | 14 (93.4%) | 1 (6.6%) | 15 (100%) |
| Duplication cyst | 10 (90.9%) | 1 (9.1%) | 11 (100%) |
| Duodenal obstruction | 10 (83.3%) | 2 (16.66%) | 12 (100%) |
| Obstructed inguinal hernia | 7 (87.5%) | 1(12.5%) | 8 (100%) |
| Others | 6 (75%) | 2 (25%) | 8 (100%) |
| Total | 249 (83.6%) | 49 (16.3%) | 298 (100%) |
Showing distribution of post operative complications.
| Complications | Number (%) |
|---|
| Septicaemia | 107(36%) |
| Anastamotic leakage | 33(11%) |
| Wound dehiscence | 15(5%) |
| Aspiration pneumonia | 27(9%) |
| Others | 15(5%) |
In our study population, 11% of neonates (33) were premature. Among them, jejunal atresia was commonest (11) followed by duodenal atresia (9), malrotation gut (8), meconium ileus (3) and ileal atresia (2). Mortality in preterm was much higher than in term newborns with intestinal obstruction. On statistical analysis, p-value came out to be < 0.05, hence statistically significant [Table/Fig-7].
Showing comparison between preterm and term newborns.
| Died | Survived | Total |
|---|
| Preterm | 10 | 23 | 33 |
| Term | 39 | 226 | 265 |
| Total | 49 | 249 | 298 |
Discussion
Intestinal atresias are the most common cause of neonatal intestinal obstruction [2]. Atresia are due to failure of recanalisation or due to intrauterine vascular catastrophy due to volvulus, duplication and intrauterine intussuception resulting in atresia of different types. Forty to fifty percent of patients in a large series had evidence of either intrauterine bowel necrosis or peritonitis. Duodenal atresia results from congenital failure of recanalization that normally occurs during 9-11 weeks of gestational age. It is frequently associated with other congenital anomalies, such as additional intestinal atresias, congenital heart disease, or as a part of VACTERL association; most often mentioned anomaly is mongolian idiocy. Antenatally atresia can be diagnosed by polyhydramnios and ultrasonography. Atresia of the colon is much less frequent than of small bowel. The mortality from atresia of the ileum is much higher than from atresia of the duodenum, owing to greater incidence of early perforation [2].
In our study, atresia came out to be the most common cause. This finding was similar to a study conducted in Bhopal where intestinal atresia was the most common cause of neonatal intestinal obstruction followed by Hirschsprung disease [3]. A study conducted in PGIMER Chandigarh [9] showed, a similar aetiological prevelance with atresia comprising 22.4% of intestinal obstruction among neonates. Our incidence of 49.6% was much higher than seen in other studies like Saha et al., (22%) in Bangladesh, Ameya et al., (21%) and Ademuyiwa et al., (29.6%) in Nigeria (21%) [7,10,11]. Among all cases of intestinal atresias, jejunoileal atresia predominate (74.3%) which was concordant with study in Zaria, Nigeria (80%) [7]. In intestinal atresia, male female ratio was 1.5: 1 in our study whereas, equal incidence in both sexes has been reported in literature [2,12–14]. Presentation of atresia is usually early i.e. within 7 days. Early onset of symptom and rapid deterioration of patient’s condition in intestinal atresia and meconium ileus was the probable cause of early presentation. Gestational age and birth weight which are also an important determinant in neonatal surgical outcome, were also comparable to that in other studies [3,8,11].
Hirschsprung disease was a major cause in other studies [7,10,11] whereas in our study incidence of Hirschsprung was less than intestinal atresia. Study conducted in Dhaka by Saha et al., showed 35.3% incidence which was higher than intestinal atresia (22%) [10] whereas, in Zaria, Nigeria [7] incidence was almost equal with Hirschsprung (23.4%) leading over atresia (21%). In Hirschsprung disease, male female ratio of 7:1 is concordant with the literature. Median age in Hirschsprung disease was late i.e. 10 days in our study which was later than median age of 6 days in similar study in Nigeria [7]. Presentation was delayed in Hirschsprung disease and malrotation because of variability in onset of symptom and lack of specificity. Early presentation leading to early detection is an important determinant in better outcome of surgery but in Hirschsprung disease prognosis was good even in late presenters as decompression was done repeatedly by doing enema at peripheral centres.
Among other causes, malrotation gut came out to be 3rd important (11.7%) cause of neonatal intestinal obstruction. It is caused by a failure of normal bowel rotation. Incidence in our study was higher than study in Dhaka [10] (9.8%). This can cause obstruction and sometimes of the small and large bowel, known as volvulus. Among rare causes there were patent VID, obstructed hernia and duplication cysts which were noticed.
Meconium ileus (28%) was one of the commonest cause of obstruction as mentioned by Saha et al., in his study whereas cases of meconium ileus were quite less i.e. 7.3% in our study. Even among these, 7 cases were associated with jejunoileal atresia and 3 cases with volvulus. Associated anomalies contribute to bad prognosis in meconium ileus.
The mortality associated with neonatal intestinal obstruction ranges between 21% and 45% in developing countries, unlike less than 15% in Europe [15,16]. Postoperative mortality in our study was 16.4% which was in between reported international publications. Hanif et al., in their experience in DMCH [14] observed a postoperative mortality of 15.4% and Islam et al., reported 20.8% mortality in RMCH which is close to our series [16]. In our study we have excluded moribund patients who were inoperable leading to better survival in our set up than other developing countries and this is also the limitation of our study.
In our study most common cause of mortality was sepsis followed by anastamotic leakage. Sepsis was mainly due to late presentation leading to perforation or in cases of meconium ileus leading to peritonitis [17]. Preterm babies are especially prone to get sepsis and other complications such as anastamotic leakage, apnoea and electrolyte imbalance.
Sepsis contributed significantly to mortality in this report, as in other reports [17]. Prevention of postoperative sepsis and complications like anastamotic dehiscence and burst abdomen which require a repeat surgery, are necessary for improved survival. With advanced surgical techniques, better paediatric anaesthesia support and improved neonatal intensive care, survival of newborns after surgery has increased tremendously in the recent years.
As our hospital is a rural based hospital, where peripheral services are not so equipped to detect intestinal obstruction at an early stage so some patients were present late which may lead to poor outcome as a result of failure to gain weight, repeated vomitings and electrolyte imbalance. Moreover, antenatally very few cases were detected as a result of ignorance and non availability of proper antenatal services in the periphery. An Indian study proved that prolonged neonatal transport (>1 hour) was found to increase the mortality among transported neonates [18].
Patients who were having some risk factor like prematurity, low birth weight, late presentation, associated severe congenital anomalies were more prone to have bad prognosis even after surgery. Not much can be done about prematurity and associated anomalies; but delay in diagnosis and treatment, which is a considerable factor is subject to correction. The type of surgical condition as well as the surgery performed also affects the outcome of patients in an institute. Last but not the least there are some important unresolved, non-countable and concealed issues like motivation for surgical treatment, socioeconomic condition, better infrastructure etc. which are difficult to report and record.
Conclusion
Our retrospective study shows intestinal atresia as the most common cause of neonatal intestinal obstruction. Antenatal diagnosis with early referral, improved surgical skills and technologies, adequate staff and post operative care can be made possible by collaborative efforts of paediatricians as well as paediatric surgeons along with investments in neonatal surgery subspeciality are all required to reduce mortality and ensure better outcome in newborns with intestinal obstruction in developing countries.