With increasing trend to high speed motor vehicle accidents, the incident of compound fractures are increasing exponentially over the time. Among all compound fractures, tibial compound fracture is the most common injury encountered these days [1]. Till today management of open leg fracture is a great therapeutic problem because of subcutaneous bone and less soft tissue coverage of the tibia. These factors also make tibia to more vulnerable to non- union and infection. Both bone leg injuries also require most number of plastic surgery procedures. The achievement of union and prevention of infection in compound leg fracture had always remained a great challenge to orthopaedic surgeons. During recent past, there was great advancement in the management of open fracture of tibia. Various modalities of treatment were used in the past for the management of compound fracture of tibia and these includes application of POP cast with window for dressing, use of external fixator as definitive management till union, use of Ilizarov technique [2–5] and also use of primary interlocking [6–8] with variable results. All these modalities have some or other limitations like joint stiffness, poor patient compliance. Long term use of rigid external fixation often leads to non union. Ilizarov have poor patient compliance and not desired in cases of without bone loss. Long term fixator application leads to pin tract infection, pin loosening and secondary osteomyelitis of bone at pin side. Primary Interlocking is a good alternative for compound fracture but early interlocking in severely contaminated and compromised state is not well advised as this had shown high infection rate. To overcome these short coming of External fixator and interlocking nails, we in current study combined the benefits of both of these methods [9].
In current study we stabilized the compound fracture of leg with external fixator after thorough debridement and built the patient for definitive management by interlocking nail. Meanwhile wound management done using vacuum assisted closure method (VAC) [10,11]. The final outcome of the procedure assessed using modified Ketenjian’s Criteria [12] and results were compared with the literature.
External fixation followed by delayed unreamed interlocking nailing minimises the disadvantages of external fixation alone (bad cosmetic, frequent pin trouble, risk of fracture through the pin tract, risks of malunion, delayed union, non-union and non-compliance of patients in pin tract care affecting fixator durability. Early external fixation followed by delayed definitive fixation is a good in cases of multiple fracture cases with multisystem injury.
Materials and Methods
Present study was conducted during the period of May 2010 to Sep 2013. During that period total 228 cases of compound fracture of tibia were presented in trauma centre. Out of these 228 cases 84 cases qualify with our inclusion criteria for current study. The selection of these cases were done from cases attending the trauma centre of tertiary level 1000 bedded medical college situated at rural setup in North India. All cases of compound fracture were evaluated and selected according to the inclusion criteria set up for current study as below.
Inclusion Criteria
Compound Grade IIIA/IIIB fracture of tibia involving diaphyseal area of the bone.
Only fresh injury cases up to 1 day were included.
Age more than 18 years, no upper age limit.
Exclusion criteria
Compound grade I & II cases of tibia, as these cases were managed by primary Interlocking.
Comp grade III fracture involving metaphyseal area.
Comp Grade III fractures with segmental bone loss of more than 1 Inch.
Comp grade III fracture cases with physiological compromised state like uncontrolled diabetes, pre injury vascular compromised state like atherosclerosis and burger disease, immuno compromised cases.
All these selected cases were managed by staged procedure of external fixator application followed by definitive tibial interlocking within 2 weeks of the fixator application. Out of 84 cases 48 were of Comp grade IIIA and 36 cases were of Comp grade IIIB group. All cases were of diaphyseal tibia fracture. Out of 84 fractures 60 cases were two segment fractures with transverse or short oblique fracture pattern. 14 cases had communition at fracture site. Out of these 84 cases 58 were male and 26 were female. The age range in our study group was from 18 years to 64 years with average age was 38 years [Table/Fig-1]. The mechanism of injury in these cases were road traffic accident in 66 cases, fall from height in 8 cases and agricultural injuries in 10 cases. Out of 84 cases 8 cases were of known diabetes cases with controlled sugar level, 6 cases of hypertension controlled by drugs and 4 cases were diagnosed HBs positive during investigations. Cases with uncontrolled blood sugar level were not included in this study. Ethical clearances were taken from institutional ethical committee and written informed consent was obtained from patients and their relatives with proper explanation of the procedure and possible complications. The study design for current study was prospective study.
Demographic distribution.
| CasesTotal | Average Age | Age range | Sex | Number of cases | Comp Grade | Number of cases |
|---|
| 84 | 38 y | 18-64 y | Male | 58 | Grade III A | 30 |
| Grade III B | 28 |
| Female | 26 | Grade III A | 18 |
| Grade III B | 8 |
| Total | | | | 84 | | 84 |
Operative procedure- Cases were taken to emergency operation theatre as soon as possible after presentation in casualty. Meticulous wound debridement of wound done and all dead tissue were excised. Tourniquet were not used during debridement but kept ready for any sudden uncontrolled bleeding. This was followed by temporally stabilization of fracture site using external fixator using at least four schanz pins after proper reduction. First shot of antibiotics were given as soon as possible after patient arrival in the form of IV Ceftazidime 1 gm, Inj Amikacin 750 mg IV and Inj Metrogyl 100 ml IV. Tetanus prophylaxis was also given in all cases. Postoperatively antibiotics were given IV Inj Ceftazidime 1g + Inj Akicacin 750 mg IV twice daily + Inj Metrogyl 100ml IV for 4 days followed by Inj Ceftazidime 1g IV + Inj Amikcin 750 mg for extended period time of 15 days at least. During these postoperative days wound management were done with regular daily debridement and application of Vacuum Assisted Closure (VAC) once wound condition permits. Prime importance was given to cover any exposed bone with soft tissue as soon as possible either by lateral release incision or rotation flaps. All measures were taken to cover the wound as early as possible preferably within 2 weeks of injury.
We went for definitive procedure of tibia interlocking within 2 weeks of external fixation. In current study we didn’t wait till wound closure for conversion to interlocking, as second procedure of tibial interlocking kept time bond that is within 2 weeks of fixator application. The time interval between external fixator to tibial interlocking conversion ranges from 7 days to 14 days with average duration of 12 days in our cases. Any further soft tissue procedures if required carried out after tibial interlocking in same sitting. Haemoglobin was maintained above 10 g% before second definitive procedure. During this waiting period, general nutrition of the cases were also maintained with high protein diet.
Prior to second definitive procedure, limb was prepared along with fixator. We replaced connecting rod and universal clamp of fixator during pre operative preparation of second surgery and schanz pin were prepared and cleaned with disinfectant agents. Universal clamp and connecting rod were exchanged with autoclaved ones under aseptic condition as these are outside body and patient is going for second surgery. Fixator was removed during the procedure of tibia interlocking in a staged manner. Guide wire for tibial interlocking was passed without removing external fixator by negotiating schanz pin in most of the cases. It was possible to pass the guide wire with schanz pin in place by missing these pins. Reaming were done is all cases. Gradual increasing diameter reamer passed followed by insertion of maximum possible diameter of nail. Two proximal and two distal locking bolts inserted. Some of our cases required plastic surgery intervention like skin grafting and rotation flap during interlocking to obtain wound closure. All these procedure were done once tibial interlocking were finished and limb and fracture site stabilized again.
Postoperative IV antibiotics Inj Ceftazidime 1g + Inj Amikacin 750 mg were used for the period of 7-10 days.
Postoperative physiotherapy - Non weight bearing knee bending and quadriceps physiotherapy advised after primary external fixator and also after definitive tibial interlocking in all cases. Cases were discharged after 7-10 days of tibial interlocking.
Follow up protocol- All cases were followed every 3 weeks during initial 3 months then every 6 weeks for next 6 months and then every 8 weeks for at least 2 years. During follow up cases were assessed clinically and radio logically and following findings were evaluated.
Clinical Assessment
Wound condition/skin condition.
Fever/Pain at local site /Swelling/redness/sign of inflammation.
Any pus discharge/sinus/bone exposed/ Collection of pus if any.
Range of movement at knee and ankle.
Blood investigation- ESR and CRP.
Radiological assessment
Full length view of leg AP and Lateral view.
Evidence of callus formation.
Localised osteolysis around fracture site if any.
Locking bolt loosening/Nail loosening/Bone destruction if any/Loss of fixation.
Weight bearing protocol
Non weight bearing for first 6 weeks after Interlocking.
Partial weight bearing allowed only when radio logically stable fixation without any sign of clinical and radiological infection.
Guarded weight bearing continue till radiological sign of union seen.
Full weight bearing allowed only when bony union seen radio logically.
Final outcome and result of the study were assessed using modified Ketenjian’s criteria [Table/Fig-2] at the end of the follow up. Results were evaluated and compared with the literature.
Modified Ketenjian’s Criteria [12].
| Results | Clinical Finding |
|---|
| Excellent | • No Notable abnormality |
| Good | • Occasional pain with prolonged use |
| • Joint motion 75% of normal |
| • Trivial swelling |
| • Normal gait |
| Fair | • Pain with ordinary activity |
| • Joint motion 50% of normal |
| • Small amount of sewlling |
| • Slight limp |
| Poor | • Constant pain |
| • Joint motion 50% of normal |
| • Visible deformity |
| • Limp, gait on cane or crutches |
We operated 84 cases of compound grade IIIA/IIIB fracture of both bone leg using staged procedure of external fixation followed by early conversion to tibial interlocking. Follow up duration in this study range from 20 weeks to 48 weeks with average duration of 30 weeks [Table/Fig-3]. All cases were followed up to end of the study. No cases were lost during follow up in our study. The time interval between external fixator to tibial interlocking conversion ranges from 7 days to 14 days with average duration of 12 days in our cases. Average per operative duration taken for external fixation procedure was 45 minutes and range from 30 to 60 minutes. Per operative duration taken for tibial interlocking was range from 50 to 70 minute with average of 65 minutes. Tourniquet was not used in either of these surgical procedures. Need of blood requirement depends on post trauma blood loss and haemoglobin of the cases. Both of these surgeries were blood less and blood was not needed due to loss during surgical procedure itself.
Results of the staged procedure.
| Total cases | Comp Grade | No | Average Interval btw Ex Fix to IMN | Flap Rotation | Skin grafting | Average Union Duration | Union Rate | Excellent to Good Result | Fair to poor Result | Deep Infection |
|---|
| 84 | Comp Grade III A | 48 | 10 days | None | None | 20 weeks | 47(98%) | 46(95.8%) | 2(4.2%) | 2(2.3%) |
| Comp Grade IIIB | 36 | 12 days | 12 | 6 | 24 weeks | 33(92%) | 31(86%) | 5(14%) | 4(4.7%) |
| Total /Average | | 84 | 11 days | 12 | 6 | 21 wks | 80(95%) | 77(91.8%) | 7(8.2%) | 6 (7%) |
Out of 84 cases operated 18 cases required plastic surgery procedures as flap rotation and delayed skin grafting and all these 18 cases were of comp grade IIIB cases to start with. Rest of these cases wound healed by regular dressing and application of vacuum assisted closure. Vacuum assisted closer (VAC) drastically reduced the need of plastic surgery procedures. Sixteen cases shown sign of infection during postoperative period and most of these were superficial infections and healed without any serious consequences. Six cases had shown signs of deep infection in the form of pus discharge with other systemic features like fever and malaise. These cases were further managed by serial irrigation, repeated culture and sensitivity and then culture specific long term antibiotics for 6 weeks with retention of same implant. Three of these cases achieved union with retention of infected implant with suppressive antibiotic coverage. Rest 3 cases gone in to non-union as there were loss of reduction due to loosing of implant. These three cases required removal of implant to control infection and further managed by ring fixator and antibiotic beads.
Out of 84 cases union were achieved in 80(95%) of our comp grade III cases that is a high percentage rate. Duration taken for union in comp grade III A cases in our series range from 12 weeks to 40 weeks and average duration were 20 weeks [Table/Fig-4,5]. Duration taken for union in comp grade III B cases in our series range from 14 weeks to 48 weeks and average duration were 24 weeks In three cases union were not achieved, these cases were further managed by external fixators like rail and ring fixator with antibiotics beads.
Case one: a) Postoperative Tibia Interlocking X-ray of case one with pin tract site seen; b) Postoperative X-ray at 8 weeks showing callus formation at fracture site; c) Follow up X-ray at 20 weeks showing fracture consolidation.
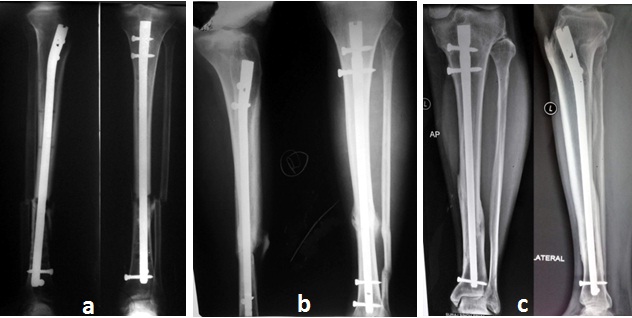
Case two: a) Postoperative follow up X Ray at 8 weeks with pin tract seen; b) Follow up X ray at 16 weeks callus formation at fracture site; c) Follow up X ray at 20 weeks showing fracture consolidation.
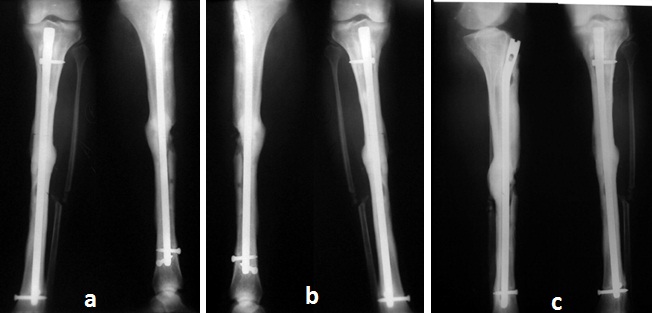
Out of total 84 cases of our follow up 80(95%) cases achieved union. 14 cases required some secondary procedures to attain bony union. Six cases required dynamization alone by removing locking bolts from far side of fracture side. Seven cases required fibulectomy with dynamization to achieve union and one case required debridement with repeat skin coverage procedure. The overall final functional outcome of all cases were evaluated according to modified Ketenjian’s criteria and overall results were excellent in 31(37%) cases, Good in 46 (54.8%) cases, Fair in 4 (4.7%) cases and poor result seen in 3(3.5%) cases [Table/Fig-6,7].
Postoperative clinical image showing compound fracture with Fixator in place.
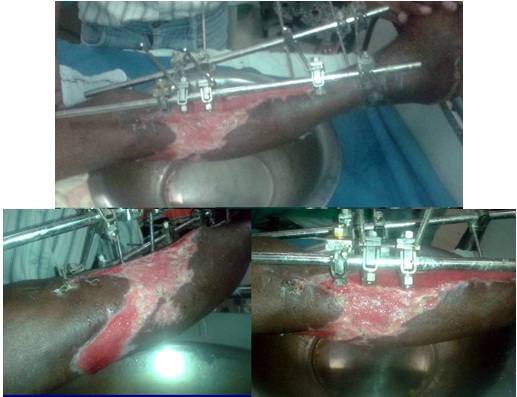
Clinical image of the case after 10 day of fixator and VAC application.

Discussion
Management of compound fracture of tibia had evolved greatly. Previously compound fractures of the leg were managed by casting with a window for wound care. The introduction of external fixator revolutionized the management of open fracture as it provided fracture stability with advantage of wound management. External fixator and intramedullary nail is currently the method of choice in the treatment of open tibial fractures. Combined use of these two methods in the treatment of compound leg fractures were advocated by many surgeons. Advantages of external fixation for the management of soft tissue problems with the advantages of intramedullary nailing in avoidance of malunion, reduced incidence of delayed union and early rehabilitation were added up. We in our study had gone one step further with addition of Vacuum Assisted Closure (VAC) to the open wound after application of the external fixation [Table/Fig-8]. This VAC leads to very early closure of the wound and decreases the time interval required for conversion to definitive interlocking. We noted the reduction of infection rate to only 7% in compound fracture using this method.
Clinical Final Outcome of the cases with range of knee movement.

Sinha k et al., used Vacuum Assisted Closure(VAC) and shown that after 4 days, 20% cases shown no bacterial growth and on 8th day 60% cases shown no bacterial growth whereas in non VAC cases only 20% of patients had no bacterial growth on the 8th day [11]. In our current study we used this advantage of VAC system for early closure of wound and to convert external fixator to intramedullary nail as soon as possible. We were achieved early conversion duration of less than 2 weeks with the help of VAC system. Ueno M et al., that reported in their study that in Gustilo type III B open tibia fractures, conversion from external fixation to definitive nailing have very high infection rate [13]. They shown that nailing without reaming with flap coverage after external fixation is effective option for comp grade IIIB fractures. Here we adopted little different strategy and managed Comp grade III A/B cases with staged manner but used aggressive method for wound closure with VAC and early conversion to definitive nailing and achieved excellent results.
Hungria et al., reported 36 tibial open fracture managed by pin less fixator followed by intramedullary nail [14]. They reported 13-23% infection rate in their series. They reported that pin less external fixator has less complication rates. We in our study included Comp grade IIIA/B cases for staged procedure and initial soft tissue/bone temporarily stabilised with fixator and later converted to definitive nailing and achieved 91% good to excellent results. Park et al., in their study compared immediate and delayed interlocking in comp Grade IIIB fractures of tibia and concluded that delayed unreamed nailing had lower infection rate and less union time [15]. We in our study used reamed nail to accommodate maximum possible diameter of nail and able to achieve excellent to good result in 91% of cases. We in our study used this method of early conversion of fixator to nailing and achieved excellent to good results in 91% of cases. Six cases of deep infection were seen in our study and this was most import cause of poor to fair result. S Gopal et al., Shown in their study that early radical debridement with early fracture fixation followed by early soft tissue coverage procedures had given faster union time and better functional result [16].
Nowotarski PJ et al., managed 49 compound femur fractures with fixator followed by static interlocking intramedullary nail [17]. They reported infection rate of 1.7% and 11% reoperation rate. The range of motion of knee was 107 degree. In our study we converted to nailing in two weeks instead of one week as early bone coverage is possible in femur fractures or they are already covered. VAC application and wound management in tibia had taken time of two week at least in our series. We achieved good to excellent results with our protocol.
Hull PD et al., managed 459 cases of open tibia fracture and studied the relation between time delay in debridement and deep infection [18]. They reported that among grade II and Grade III fracture there were significant increase in the rate of infection i.e. 3% with per hour delay. They reported total 10% infection rate with delay of 10.6 hours. We in our series done immediate debridement and we noted 7% deep infection in our cases.
Mathews JA et al., managed Gustilo Grade III open tibial fractures by single stage procedure [19]. In their study they managed 48 cases and reported 34.6% infection rate in cases underwent definitive fixation and coverage at separate operation. While in our study deep infection rate were only 7%. With the application of vacuum assisted closure (VAC) we were able to reduce the infection rate to as low as 7% even in compound Grade IIIb fractures.
Limitations
In our current study there were some limitations. Patients required two separate surgical procedures within the short period of two weeks. Application of VAC required long hospitalization of the cases. This also increases the cost of this staged procedure.
Conclusion
Now a day increasing treads were going towards early primary interlocking of Compound grade I/II diaphyseal fractures of the tibia and also well established method of management of diaphyseal fractures without bone loss. Primary interlocking in Comp grade IIIA/B fractures are still controversial as study had shown high infection rate and high failure rate. We in our study concluded that compound Grade IIIA/B fractures of both bone leg could be well managed by delayed interlocking within 2 weeks with initial temporally External fixation. Vacuum Assisted Closure (VAC) give a good help for rapid closure of the wound and help in early conversion to definitive intramedullary nailing. Early conversion to nail within 2 weeks lessens the risk related to pin tracts infection and also shown lesser complication. Reamed nail could well be used in compound grade IIIA/B fractures without increasing the risk of infection. It gives better stability to fracture site and lessen the risk of implant failure.