Metastatic Collision Tumour (Papillary Thyroid Carcinoma and Squamous Cell Carcinoma) in Cervical Lymph Nodes: An Immunohistochemical Analysis
Alshimaa Mahmoud Alhanafy1, Dalia Al-Sharaky2, Asmaa Gaber Abdou3, Rania Abdallah Abdallah4
1 Faculty of Medicine, Department of Clinical Oncology, Menoufia University, Egypt.
2 Faculty of Medicine, Department of Pathology, Menoufia University, Egypt.
3 Faculty of Medicine, Department of Pathology, Menoufia University, Egypt.
4 Faculty of Medicine, Department of Pathology, Menoufia University, Egypt.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Asmaa Gaber Abdou, Department of Pathology, Menoufiya Faculty of Medicine, Shibeen El Koom, 32817 Menoufiya Governorate, Egypt.
E-mail: asmaa_elsaidy@yahoo.com
Collision tumours are a rare entity, in this report, we describe a case of 73-year-old woman presented with a rapid enlargement of left upper cervical lymph node (LN) associated with right thyroid nodular goiter. The histopathological examination of the excised LN showed definite areas of papillary thyroid carcinoma admixed with moderately differentiated squamous cell carcinoma (SCC). Thyroglobulin immunostaining was positive in papillary carcinomatous areas confirming thyroid gland as a source of metastasis. Then the patient underwent total thyroidectomy and neck dissection, which revealed multicentric classic papillary thyroid carcinoma with an absence of squamous differentiation on extensive sampling. The patient received adjuvant radioactive iodine, but the neck swelling was rapidly progressing, ulcerated and infected. Computed tomography (CT) revealed left large cervical amalgamated LN and two metastatic lung nodules, the patient received 2 cycles of chemotherapy and was planned for external beam radiotherapy but she died within 7 months of first presentation. Collision tumours pose a diagnostic as well as therapeutic challenge and carry a rapidly progressive course and a fatal outcome. SCC is considered as a dedifferentiation of papillary thyroid carcinoma, which may appear in metastatic site rather than the primary site.
Thyroglobulin, TTF1, CK19, CK7, p63
Case Report
A 73-year-old woman presented with a rapidly enlarged hard non tender left upper cervical lymph node. Clinical examination and endoscopy ruled out any other abnormalities of the upper aerodigestive tract. Imaging of the neck and paranasal sinuses showed left upper cervical lymph node measuring 4x3 cm and right thyroid nodular goiter. Chest x-ray and pelvi-abdominal US were free from metastatic disease.
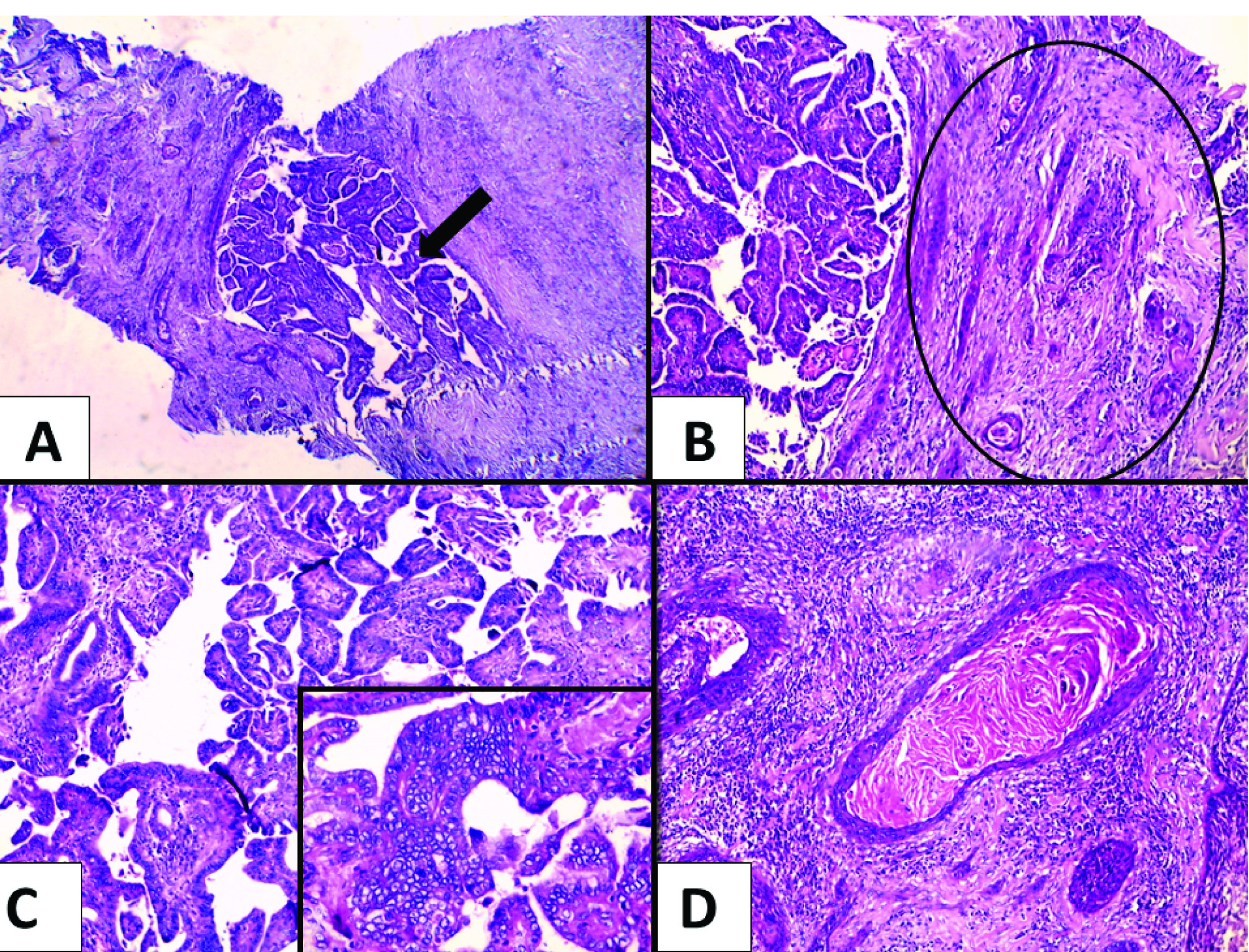
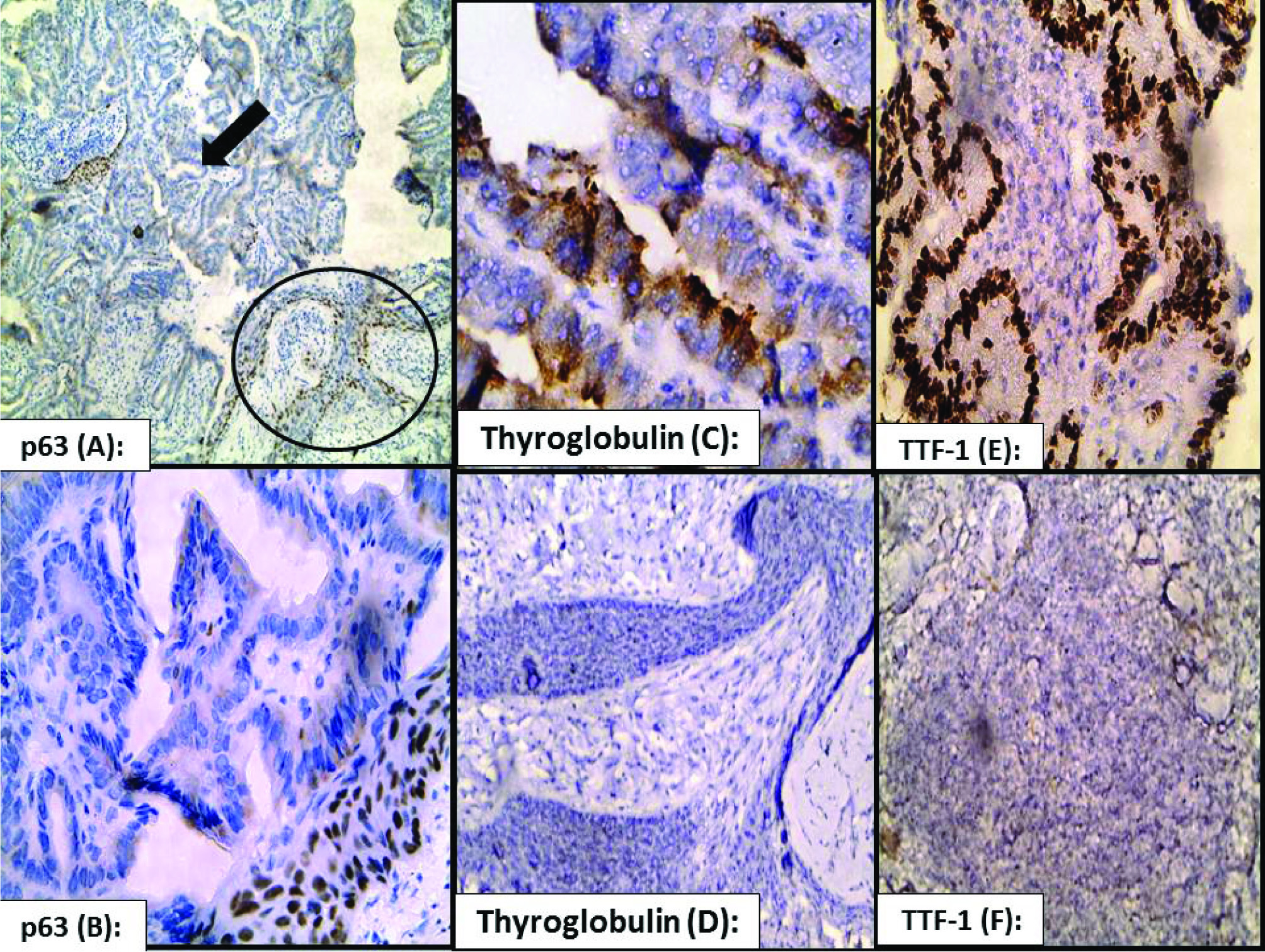
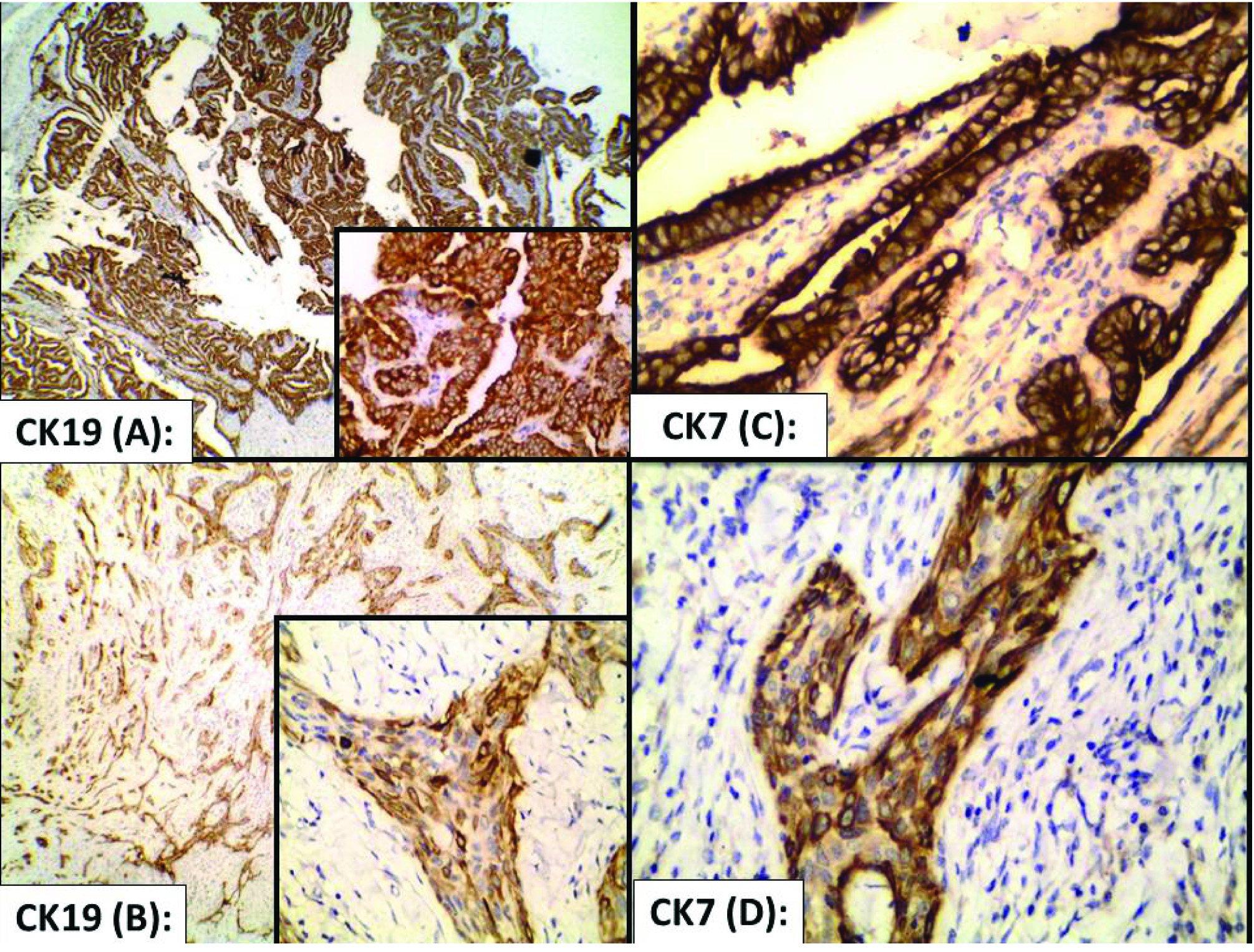
The patient underwent surgical excisional biopsy of this lymph node. Grossly, the received lymph node measured 4x3x1cm with a grayish white cut section. Histopathological examination revealed replacement of lymph nodal tissue by two distinct neoplasms, papillary thyroid carcinoma and moderately differentiated squamous cell carcinoma [Table/Fig-1]. Immunohistochemical staining was performed using thyroglobulin, thyroid transcription factor-1 (TTF-1), p63, cytokeratin 7 (CK7) and cytokeratin 19 (CK19). Cytoplasmic and nuclear staining for thyroglobulin and TTF-1 [Table/Fig-2] were seen in papillary carcinomatous areas, respectively, while nuclear staining for p63 [Table/Fig-2] was seen in squamous areas. On the other hand, immunoreactivity for CK7 and CK19 [Table/Fig-3] was seen diffusely in both the papillary and squamous areas.
Metastatic collision tumour in cervical lymph node: a) two malignant neoplasm can be appreciated, one is clearly arranged in a papillary pattern (arrow) (H&E x40) and the other; b) in sheets and nests of SCC (black circle) (H&E x40); c) higher power of the papillary thyroid carcinoma classic type, with clear diagnostic nuclear features (H&E x100 and inset x400); d) higher power of the SCC with central keratinization (H&E x400).
p63, thyroglobulin, TTF-1 in collision tumour: a) nuclear p63 stain is seen in the SCC (black circle) while absent in the papillary thyroid carcinoma (black arrow) (immunoperoxidase x200); b) moderate to strong nuclear p63 stain is evident in the SCC (immunoperoxidase x400); c) Moderate to strong cytoplasmic thyroglobulin stain is evident in papillary thyroid carcinoma (immunoperoxidase, x400); d) complete absence of the thyroglobulin in the SCC (immunoperoxidase x400); e) strong nuclear stain of TTF-1 in the papillary thyroid carcinoma (immunoperoxidase x400); f) absence of TTF-1 nuclear stains in the SCC (immunoperoxidase x400).
CK 19 and CK7 in collision tumour: a) Cytoplasmic CK 19 stain in papillary thyroid carcinoma (immunoperoxidase x40 and inset x400); b) in SCC (immunoperoxidase x 100 and inset x 400); c) Cytoplasmic CK7 stain in papillary thyroid carcinoma (immunoperoxidase x400); and d) in SCC (immunoperoxidase x400).
After 2 weeks, the patient underwent total thyroidectomy and neck dissection, histopathology revealed multicentric classic papillary thyroid carcinoma, stage T2 (tumour >2 cm), N1 (1/35 lymph nodes), the positively involved lymph node showed classic papillary thyroid carcinoma. Extensive sampling of the available thyroid tissue revealed no squamous differentiation. During recovery after surgery, an enlarging left upper neck swelling and thickening at operative bed was detected. The patient received antibiotics and anti-inflammatory drugs. The patient’s thyroid function tests including T3 and T4 were within normal, while thyroid stimulating hormone (TSH) was high.
The patient received adjuvant radioactive iodine, but the neck swelling was rapidly progressing within one month and became locally invasive and unresectable. Postoperative CT neck revealed left cervical amalgamated lymph node (LN) (8x7 cm), while CT chest, abdomen and pelvis revealed two small peripheral bilateral lung nodules. Bone scan and brain magnetic resonance imaging (MRI) were free.
During so, the mass became larger (14x8 cm) raising the ear, ulcerated, infected and oozing pus, patient had frequent hospital admission with attacks of stridor, dyspnea, hoarseness and dysphagia. The patient was planned for palliative external beam radiotherapy; she had partial response with significant toxicity in the form of anorexia, weight loss and deterioration of her performance status. The ulcerated LNs decreased in size to 10X5 cm but still infected, multiple culture and sensitivity were done and proper antibiotics were received. The patient received 2 cycles of chemotherapy (cisplatin/adriamycin) with poor tolerance and finally died of septicemia due to uncontrolled infection of ulcerated neck nodes with short overall survival of about 7 months.
Discussion
Collision tumour represents a rare entity that shows co-existence of histologically different neoplasms of distinct origin in a single site. Detailed histopathological and immunohistochemical studies should confirm the diagnosis and may give an idea about the origin of these tumours.
Collision tumours development can be explained by several theories including a chance of accidental meeting of two primary tumours or the alteration of microenvironment by one tumour facilitating the development of the other. Moreover, the two tumours may have common single stem cells [1].
Thyroid gland is a very rare location for collision tumours, which included mixed histologies of follicular or papillary and medullary carcinomas, while the co-existence of papillary carcinoma and squamous cell carcinoma (SCC) is very special [1]. SCC of thyroid could arise from the embryonic remnants such as thyroglossal duct, thymic epithelium and ultimobranchial body [2]. Squamous metaplasia induced by environmental stimuli such as inflammation and Hashimoto’s thyroiditis may predispose to SCC of thyroid [3]. Lastly, SCC could be the dedifferentiation stage of previously existing papillary, follicular, medullary and anaplastic thyroid carcinomas [4,5].
Papillary thyroid carcinoma is the most common thyroid malignancy with an excellent prognosis whereas primary SCC of the thyroid gland is very rare accounting for less than 1% of all thyroid malignancies with poor prognosis [6,7]. SCC of the thyroid could be presented with a rapidly enlarging neck mass associated with pain, dysphagia, dyspnea, and hoarseness, local invasion of adjacent structures and early metastatic spread [6]. The case presented in the current study also showed aggressive features manifested by early lymph node metastasis and lung metastasis together with short survival (7 months). Primary SCC of the thyroid whether pure or in association with papillary carcinoma is more common in patients in their 5th and 6th decades [7]. This old age at presentation could be due to the long time required for squamous metaplastic foci of papillary thyroid carcinoma to undergo malignant transformation to SCC [8].
Before designating the case as primary SCC of thyroid, metastasis should be excluded. Diagnostic workup was performed in the present case to rule out extrathyroid primary SCC as an origin for the metastaic lymph node. Clinical examination, panendoscopy and a CT scan did not reveal any possible site as the origin for the SCC. However, histopathological assessment of the total thyroidectomy specimen revealed the presence of multicentric papillary thyroid carcinoma only without any evidence of SCC. Immunohistochemical staining was done to confirm the cell of origin, SCC stained positively for p63 and papillary thyroid carcinoma stained positively for thyroglobulin and TTF-1. However, these results were not conclusive regarding the tissue of origin of the SCC, if it originates from thyroid or not. Therefore, it was mandatory to stain the SCC element with CK7 and CK19 [6,7,9]. A diffuse cytoplasmic staining of the SCC elements with CK7 and CK19, confirmed thyroid as a primary site of these SCC elements.
The treatment of SCC of the thyroid is challenging and usually involves several modalities [6]. Our patient was submitted to surgery in the form of total thyroidectomy and neck dissection followed by radioiodine treatment, two cycles of chemotherapy and external beam radiotherapy. The addition of external beam radiotherapy was suggested because the patient suffered from rapidly enlarging nodes and pulmonary metastasis beside the role of radioiodine is questionable in treating SCC of the thyroid.
Conclusion
Collision tumours pose a diagnostic as well as therapeutic challenge and carry a rapidly progressive course and a fatal outcome. Squamous cell carcinoma is considered as a dedifferentiation of papillary thyroid carcinoma, which may appear in metastatic site rather than the primary site.
[1]. Brandwein-Gensier M, Urken M, Wang B, Collision tumour of the thyroid: a case report of metastatic liposarcoma plus papillary thyroid carcinomaHead & Neck 2004 26:637-41. [Google Scholar]
[2]. Goldberg HM, Harrey P, Squamous cell cysts of the thyroid with special reference to the etiology of squamous epithelium in the human thyroidBr J Surg 1956 43:565-69. [Google Scholar]
[3]. Chaudhary RK, Barnes EL, Myers EN, Squamous cell carcinoma arising in Hashimoto’s thyroiditisHead Neck 1994 16:582-85. [Google Scholar]
[4]. Bronner MP, LiVolsi VA, Spindle cell squamous carcinoma of the thyroid: an unusual anaplastic tumour associated with tall cell papillary carcinomaMod Pathol 1991 4:630-43. [Google Scholar]
[5]. Kebapci N, Efe B, Kabukcuoglu S, Akalin A, Kebapci M, Diffuse sclerosing variant of papillary thyroid carcinoma with papillary squamous cell carcinomaJ Endocr Invest 2002 25:730-34. [Google Scholar]
[6]. Booya F, Sebo T J, Kasperbauer JL, Fatourechi V, Primary squamous cell carcinoma of the thyroid: report of ten casesThyroid 2006 16:89-93. [Google Scholar]
[7]. Lam KY, Lo CY, Liu MC, Primary squamous cell carcinoma of the thyroid gland: an entity with aggressive clinical behavior and distinctive cytokeratin expression profilesHistopathol 2001 39:279-86. [Google Scholar]
[8]. Warman M, Lipschitz N, Ikher S, Halperin D, Collision tumour of the thyroid gland: primary squamous cell and papillary thyroid CarcinomaISRN Otolaryngology 2011 582374:1-2. [Google Scholar]
[9]. Sutak J, Armstrong JS, Rusby JE, Squamous cell carcinoma arising in a tall cell papillary carcinoma of the thyroidJ Clin Pathol 2005 58:662-64. [Google Scholar]