Malignant Proliferative Trichilemmal Tumour of The Nape of The Neck – A Case Report
Alagar Raja Durairaj1, Surya Rao Rao Venkata Mahipathy2, Thanga Thirupathi Rajan Vivakaran3, Volga Harikrishnan4, Muthuvel Esakki5
1 Associate Professor, Department of Plastic Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
2 Associate Professor, Department of Plastic Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
3 Associate Professor, Department of Neurosurgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
4 Assistant Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
5 Associate Professor, Department of Pathology, Saveetha Medical College & Hospital, Thandalam, Kanchipuram, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Surya Rao Rao Venkata Mahipathy, Associate Professor, Department of Plastic & Reconstructive Surgery, Saveetha Medical College & Hospital, Thandalam, Kanchipuram Dist - 602105, Tamil Nadu, India.
E-mail: surya_3@hotmail.com
Proliferating trichilemmal tumours are benign but locally aggressive tumours arising from the hair follicle. They are biologically benign lesions, but may be locally aggressive. They are generally solitary lesion and commonly occurring in the scalp of elderly women. Malignant transformation has been known to occur but very rarely. Here we report a rare case of a recurrent malignant trichilemmal tumour of the scalp in a middle aged male which was surgically excised.
Hair follicle, Rare, Recurrent, Surgical excision
Case Report
A 32-year-old male presented to us with swelling over the nape of the neck for around 7 years. It started as a small swelling and has gradually progressed to the present size [Table/Fig-1]. He also complains of dull pain over the swelling. There is no history of ulceration or bleeding. The patient gives a history of a similar swelling in the same region 11 years ago for which a probable excision biopsy was done elsewhere (details not available). There was no history of involvement of respiratory, abdominal or central nervous systems.
Clinical photograph showing the lesion

On examination, a swelling measuring approximately 12 x 8 cm was present in nape of neck, extending from the occipital protuberance to seventh cervical vertebra, non-tender, firm to hard in consistency, partially fixed in the nape of the neck, skin over swelling was stretched shiny and not pinchable with multiple bilateral cervical lymphadenopathy. Neurosurgeon was consulted and a probable diagnosis of a recurrent soft tissue sarcoma was made.
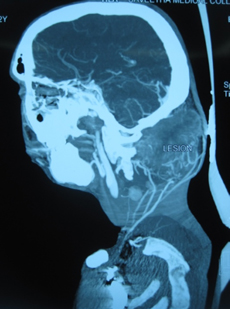
CT Neck Angiography revealed a large lobulated subcutaneous, inter and intramuscular moderately heterogeneous enhancing lesion of size 9.14 x 7.5 x 7.5 cm seen in the posterior aspect of lower occipital and upper neck region extending from occipital protuberance to C3 spinous process with loss of fat planes with posterior paraspinal muscles and no significant cervical lymphadenopathy. There is no evidence of cervical vertebrae erosion/intraspinal extension. Lesion is supplied by both external carotid arteries (occipital & posterior auricular) and proximal subclavian artery branches (thyrocervical trunk) [Table/Fig-2].
CT Neck Angiography showing the vascular lesion with loss of fat planes
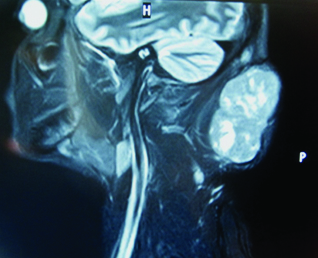
MRI showed a similar picture with heamorrhagic foci in the lesion and largest cervical lymph node measuring 8 mm [Table/Fig-3].
MRI showing a large lobulated subcutaneous, inter and intra muscular moderately heterogeneous mixed signal intensity lesion extending from occipital protuberance to C3 spinous process with loss of fat planes with posterior paraspinal muscles
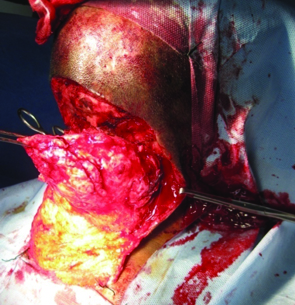
Cervical lymph node biopsy under general anaesthesia was done 10 days prior to the elective surgery, which revealed reactive lymphoid hyperplasia with sinus histiocytosis. We proceeded with wide local excision of the lesion. Under GA and in prone position (head in a horse-shoe), an incision was made along the upper margin of the lesion and a skin flap raised inferiorly. A well vascularised lobulated fibrofatty lesion was seen extending from occipital protuberance to C2 spine. The lesion was excised in toto with the help of neurosurgeon and sent for histopathological examination [Table/Fig-4].
Intra operative picture showing the lesion being excised
Haemostasis was secured and skin flap was sutured to cut scalp margin with 2-0 polyamide (nylon) sutures over a suction drain and compression dressing applied [Table/Fig-5].

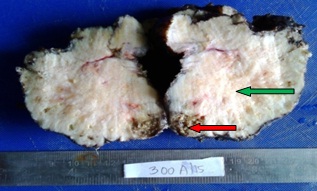
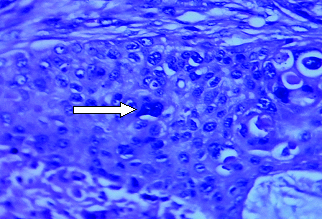
On gross examination, an encapsulated mass with nodules seen externally [Table/Fig-6] with cut surface showing solid, gray white with foci of necrosis and haemorrhage [Table/Fig-7]. Histopathology showed a malignant neoplasm composed of nests, cords, trabeculae and sheets of highly pleomorphic cells [Table/Fig-8] having hyperchromatic nuclei with prominent nucleoli and moderate eosinophilic cytoplasm [Table/Fig-9]. Few nests have pilar type keratinisation and perineural invasion, vascular emboli and skeletal muscle infiltration is seen giving an inmpression of a malignant proliferating trchilemmal tumour.
Gross image-An encapsulated mass with nodular external view

Gross image-Cut surface of the mass is solid, gray white with foci of necrosis (red arrow) and haemorrhage (green arrow)
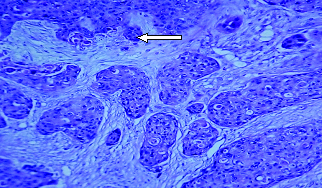
H&E (10x) Section shows nests of tumour cells infiltrating the stroma. (white arrow)
H&E (40x) The cells are pleomorphic with hyperchromatic to vesicular nuclei. Some show vacuolated cytoplasm. (white arrow)
There was marginal necrosis of the skin flap which was debrided and was healing well after which time the patient was lost to follow-up after 10 days as he went against medical advice due to personal reasons.
Discussion
Trichilemmal cysts and tumours are cutaneous lesions which arise from the outer root sheath of hair follicles, showing trichilemmal keratinisation [1]. The lesion was initially described by Wilson-Jones [2] in 1966 as a proliferating epidermoid cyst but later they were distinguished from trichilemmal tumours in 1995 [3].
Malignant proliferating trichilemmal cysts and tumours are extremely rare with very few documented cases been published in the literature [4]. The term malignant proliferating trichilemmal tumour was initially named by Saida et al., as tumour that showed the classical features of malignancy [5]. They which are wrongly diagnosed as squamous cell carcinoma, therefore it is important to differentiate from it as both share many common features. Most of proliferating trichilemmal tumours occur in the head and neck region but can involve any part of the body [1,6], commonly seen in females (84%) around the sixth and seventh decades of life [7].
Malignant change is suspected when there is a rapid increase in size with cells showing altered nuclear cytoplasmic ratio [1,8].
Magnetic resonance imaging shows a poorly marginated, ovoid, soft-tissue mass, the mass showing isointense signal on T1-weighted images and hyperintense signal on T2-weighted images relative to muscle, while contrast-enhanced CT scans showed a large, well-encapsulated, cystic mass in the subcutaneous fat, in a study done by Kim et al., [9]. The treatment in malignant proliferating trichilemmal cyst is similar to other malignant skin lesions. Surgical excision with a 1cm conservative margin remains the mainstay of treatment. Adjuvant chemotherapy is not superior to adequate surgery alone [1]. There should be careful follow-up in the postoperative period for metastasis.
Conclusion
Malignant proliferating trichilemmal tumours are rare and cause difficulty in diagnosis for the surgeon and the pathologist as there is a high risk of recurrence and metastasis. Good clinical examination with appropriate investigative modalities and wide surgical excision is the definitive treatment while alternative therapies are still under consideration.
[1]. Markal N, Kurtay A, Velidedeoglu H, Hucumenoglu S, Malignant transformation of a giant proliferating trichilemmal tumour of the scalp: Patient report and literature reviewAnn Plast Surg 1998 41:314-16. [Google Scholar]
[2]. Wilson-Jones E, Proliferating epidermoid cystsArch Dermatol 1966 94:11 [Google Scholar]
[3]. Sau P, Graham JH, Helwig EB, Proliferating epithelial cysts: Clinicopathological analysis of 96 casesJ Cutan Pathol 1995 22:394-406. [Google Scholar]
[4]. Garg PK, Dangi A, Khurana N, Hadke NS, Malignant proliferating trichilemmal cyst: A case report with review of literatureMalaysian J Pathol 2009 31:71-76. [Google Scholar]
[5]. Saida T, Oohara K, Hori Y, Tsuchiya S, Development of a malignant proliferating trichilemmal cyst in a patient with multiple trichilemmal cystsDermatologica 1983 166:203-08. [Google Scholar]
[6]. Brownstein MH, Arluk DJ, Proliferating trichilemmal cyst: A simulant of squamous cell carcinomaCancer 1981 48:1207-14. [Google Scholar]
[7]. Mori O, Hachisuka H, Sasai Y, Proliferating trichilemmal cyst with spindle cell carcinomaAm J Dermatopathol 1990 12:479-84. [Google Scholar]
[8]. Weiss J, Heine M, Grimmel M, Jung EG, Malignant proliferating trichilemmal cystJ Am Acad Dermatol 1995 32:870-73. [Google Scholar]
[9]. Kim HJ, Kim TS, Lee KH, Kim YM, Suh CH, Proliferating trichilemmal tumours: CT and MR imaging findings in two cases, one with malignant transformationAJNR Am J Neuroradiol 2001 22:180-83. [Google Scholar]