Acute or chronic headache is one of the common presenting complaints in patients attending the out patient’s department or emergency care of any hospital or general practitioner however, only about 10% of patients with recurrent headache have secondary cause [1]. It has been contended that most of the patients suffering from primary headache can be managed with primary care and no need of neuroimaging in most of the cases [2].
Because some potential aetiologies of headache may be life threatening or can badly affect neurological functions so careful assessment of a patient is very important to diagnose potentially morbid but treatable causes. Headache cause understandable concern not only on the part of the patient but also health care professional [3]. Few serious brain pathology presents with secondary headache for example a brain tumour or space occupying lesion (SOL) is a secondary cause of headache and CT/MRI is best tool for the diagnosis and treatment follow up which is essential for optimal management of secondary headache however brain tumours accounts less than 0.1% in the lifetime prevalence as a cause of headache [4]. So many times it is so difficult to discriminate between primary and secondary type of headache and it presents diagnostic dilemma before clinician. Since by definition, primary headache does not require any neuroimaging because no such underlying disease process exists which can be picked up by neuroimaging. Primary headache, which include migraine, tension headache and cluster headache are benign in nature. These types of headache are usually recurrent in nature and have no underlying organic disease in their root. Secondary headache is always caused by underlying organic diseases ranging from extra cranial benign condition such as sinusitis or mastoiditis to life threatening intracranial pathology like sub arachnoid haemorrhage or brain tumours. In general, clinical practice, it is well accepted that the so called red flags of headache needs search for secondary headache. Red flag signs and symptoms include [5]: Early morning headache, new persistent and unexplained headache in a patient aged over 50-year-old, headache associated with changes in posture or vomiting, change in personality, cognition or conscious level, headache with seizure, new onset neurological deficit, headache precipitated by coughing, sneezing or exercise, associated with visual disturbance (papilloedema) or jaw claudication (giant cell arteritis), immunosuppressed or history of malignancy, atypical aura, headache with sign and symptoms of glaucoma, headache associated with signs of systemic illness e.g. neck rigidity, rash, fever and headache subsequent to head injury.
A detailed and dedicated clinical history and thorough neurological and physical examination almost always helps in deciding which headache patient needs CT or MRI scan of brain to find out any underlying brain pathology. At times despite the absence of red flags or CWC sign, a CT or MRI scan of brain is advised by clinician to allay the anxiety of the patient and relatives. If CT is advised for neuroimaging in young children and females of child bearing age group, the issue of radiation dose will be raised. CT scanners are responsible for 40% of total medical diagnostic radiation but accounts only 4% in radiology examinations [6]. So the use of CT imaging for brain has to be balanced against the radiation dose. Computed tomography is a highly useful tool to find out root of the problems, but no one should allow it to replace the proper history taking and clinical examinations to make a diagnosis. Limited studies have been conducted in this region so present study designed to evaluate the findings of CT and MRI among patients with chief complaint of headache and to compare the findings of CT and MRI between group A (having red flag or CWC sign) and Group B (no red flag or CWC sign).
Materials and Methods
Study Design
This retrospective observational study was carried out among 500 selected patients of 10 to 70 year age, who underwent CT or MRI scan of head in Peoples College of Medical Sciences and Research Centre, Bhopal, MP during the period of 2 year in between Jan 2013 to Dec 2014. Ethical clearance was obtained from Institutional ethical committee.
Inclusion Criterion
Patient with chief complaint of headache otherwise healthy individual and having complete CT or MRI study with good quality images.
Exclusion Criterion
Patient of acute head injury or history of neurosurgery (Pts having VP shunt, aneurysm clips or coil).
Subjects were divided in to two groups A and B based on red flag and CWC sign. CT/MRI findings were evaluated for any intra and extra cranial pathology.
Statistical analysis was done using Statistical Package of Social Science (SPSS Version 19; Chicago Inc., USA). Data comparison was done by applying specific statistical tests i.e. Chi-Square test to find out the statistical significance of the comparisons. Qualitative variables were compared using proportions. Significance level was fixed at p < 0.05.
Equipment
Siemens Somatom sensations 40 slice MDCT scanner and Siemens magnetom 1.5T MRI scanner.
Results
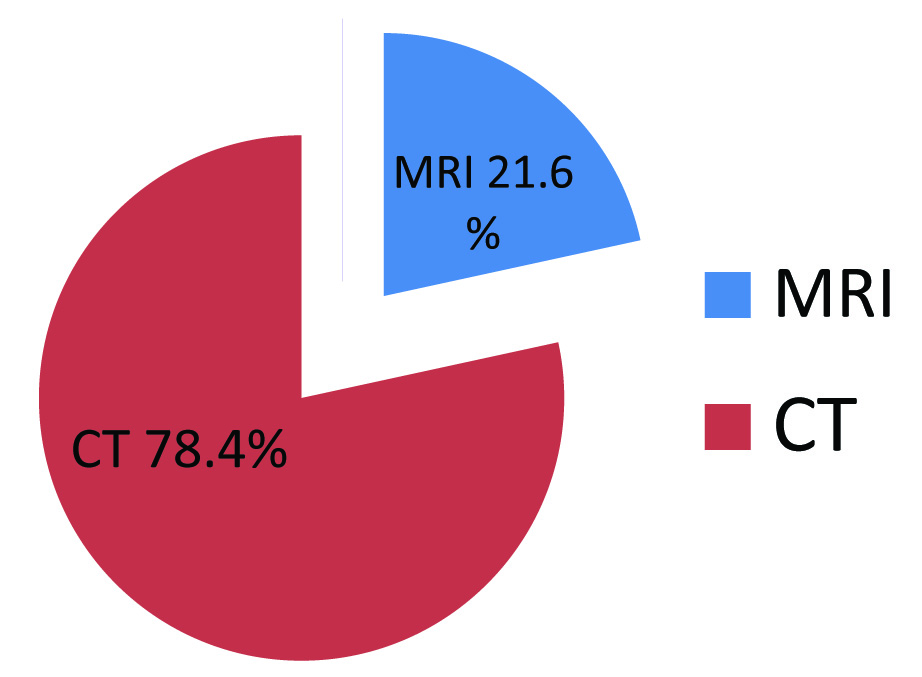
The data obtained from records of CT and MRI section of Department of Radiodiagnosis, Peoples Medical College Hospital was analysed by using SPSS program and results prepared in form of tables and figures. This retrospective observational study is conducted among 500 selected patients who underwent CT or MRI scan of head from January 2013 to December 2014. Out of 500 patients 313 (62.6%) were females and 187 (37.4%) were males; 327 (65.4%) patients belong to urban area and 173 (34.6%) belong to rural area [Table/Fig-1]. Out of 500 patients 392 (78.4%) patients underwent for CT and 108 (21.6%) for MRI [Table/Fig-1,2]. All patients were divided into two groups; group A consists of cases associated with neurological abnormality as indicated in red flag signs and CWC criterion and group B consists of cases with no red flag signs and CWC sign [Table/Fig-3]. The associations between group A and B with type of headache and positive findings were established based on chi square test. A total 56 cases among 500 cases underwent intravenous contrast administration as based on clinician’s request or when radiologist required it for better imaging and characterization of pathology.
Demographic distribution of study subjects according to modality, Locality & Gender.
| Scanning modality | MaleNo. (%) | FemaleNo. (%) | Urban | Rural | Total |
|---|
| CT | 154 (82.4%) | 238 (76.0%) | 254 (77.7%) | 138 (79.8%) | 392 (78.4%) |
| MRI | 33 (17.6%) | 75 (24.0%) | 73 (22.3%) | 35 (20.2%) | 108 (21.6%) |
| TOTAL | 187 | 313 | 327 | 173 | 500 |
| Chi Square Value | 2.76 | 0.293 | |
| Significance p-Value | 0.097 (NS) | 0.589 (NS) | |
Distribution of case according to modality.
Distribution of cases according to group.
| Group | No. ofcases | No. ofpositivecase | Normalscan | Chi-SquareValue | p-value |
|---|
| A | 48 | 29 (60.4%) | 19 (39.6%) | 34.9 | 0.001(HS) |
| B | 452 | 97 (21.5%) | 355 (78.5%) |
| Total | 500 | 126 | 374 |
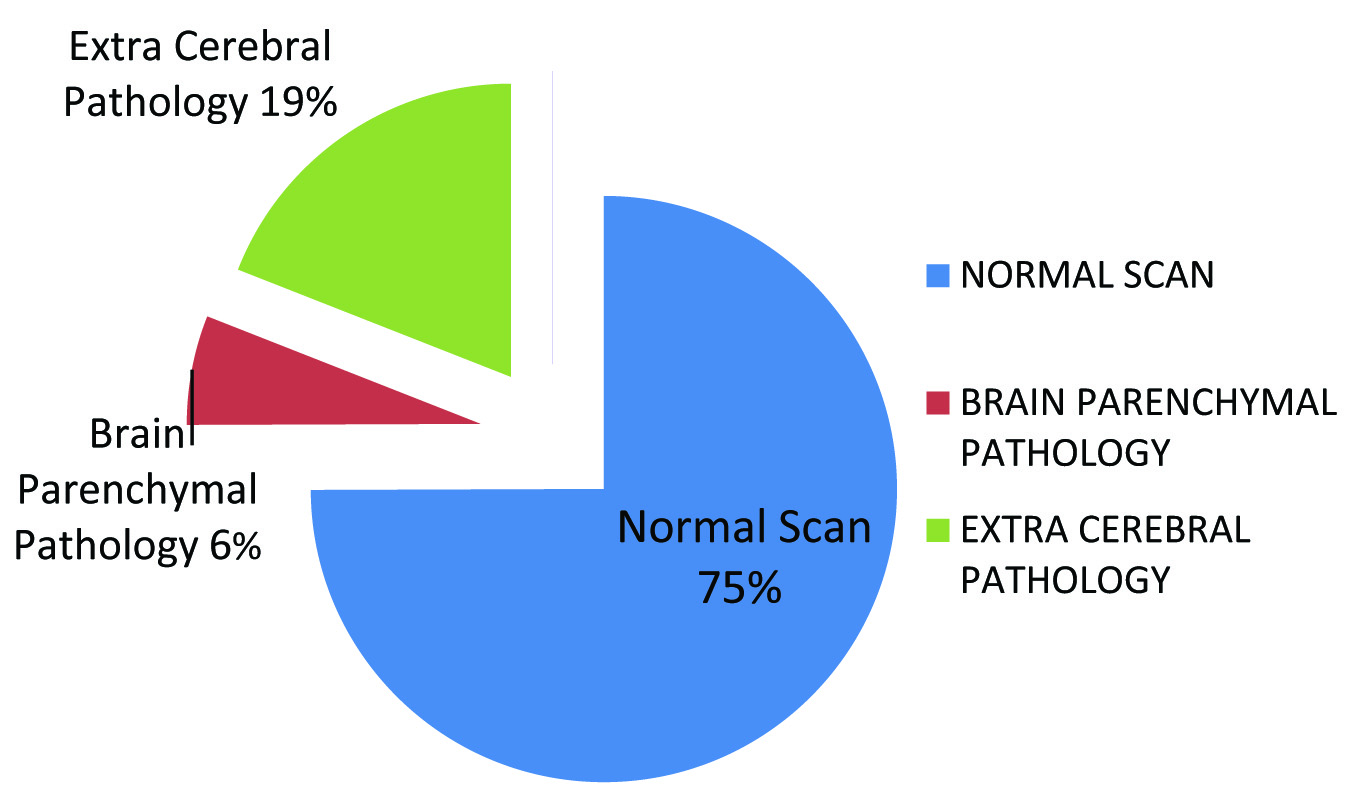
The age group ranged from 10 years to 70 years with the mean of 33 years [Table/Fig-4]. Patients less than 10 year of age is not included in the study because very few presented with sole complaint of headache and reliable history taking is difficult in this age group. Group A included 48 cases (9.6%) whereas 452 cases (90.4%) were included in group B [Table/Fig-3]. Approximately 75% of the patients included in the study demonstrated absolutely normal neuroimaging findings. Out of 500 patients only 29 (5.8%) showed brain parenchymal pathology while other associated findings were seen in 97 pts (19.4%) [Table/Fig-5]. Out of 97 patients; sinusitis is seen in 58 cases (11.6%), bone related pathology seen in 26 cases (5.2%) and CSOM seen in 13 cases (2.6%) (p-value 0.022 which is significant). Out of the 29 cases of brain parenchymal pathology, 6 cases had calcified granulomas, 4 cases had ring enhancing lesions, 5 cases had presumptive brain tumour, 5 cases had parenchymal bleed, 3 cases had presumptive demyelination, 4 case had subarachnoid and subdural haemorrhage and 2 case had aneurysm [Table/Fig-6,7,8,9 and 10].
Distribution of cases according to age.
| Sr.No. | Agegroupin yr | MaleNo. (%) | FemaleNo. (%) | TotalNo. (%) | Chi-SquareValue | p-value |
|---|
| 1 | 10-20 | 28 (5.6%) | 35 (7.0%) | 63 (12.6%) | 4.64 | 0.461(NS) |
| 2 | 20-30 | 51 (10.2%) | 94 (18.8%) | 145 (29.0%) |
| 3 | 30-40 | 47 (9.4%) | 92 (18.4%) | 139 (27.8%) |
| 4 | 40-50 | 29 (5.8%) | 50 (10.0%) | 79 (15.8%) |
| 5 | 50-60 | 15 (3.0%) | 23 (4.6%) | 38 (7.6%) |
| 6 | 60-70 | 17 (3.4%) | 19 (3.8%) | 36 (7.2%) |
| Total | | 187 | 313 | 500 | | |
Distribution of Cases According to CT/MRI Findings
Distribution of cases according to disease.
| Sr.No. | Diagnosis | MaleNo. (%) | FemaleNo. (%) | No. ofcases | Chi-SquareValue | p-Value |
|---|
| 1 | Normal | 127 (34.0%) | 247 (66.0%) | 374 | 11.0 | 0.199 (NS) |
| 2 | Paranasal Sinusitis | 22 (37.9%) | 36 (62.1%) | 58 |
| 3 | Bone related pathology | 15 (57.7%) | 11 (42.3%) | 26 |
| 4 | CSOM | 5 (38.5%) | 8 (61.5%) | 13 |
| 5 | Ring enhancing lesion and calcified granuloma | 4 (40.0%) | 6 (60.0%) | 10 |
| 6 | Brain tumors (SOL) | 2 (40.0%) | 3 (60.0%) | 5 |
| 7 | Demyelination | 2 (66.7%) | 1 (33.3%) | 3 |
| 8 | Parenchymal, subarachnoid and subdural hemorrhage | 6 (66.7%) | 3 (33.3%) | 9 |
| 9 | Aneurysm | 1 (50.0%) | 1 (50.0%) | 2 |
(a) Axial contrast enhanced MRI image of brain is showing large peripherally enhancing SOL in frontal region (arrow). (b) Axial CECT image of head shows a well-defined, markedly enhancing, rounded mass lesion in frontal region most likely meningioma (arrow)

(a) Axial CT image of brain shows a large acute hematoma in right basal ganglia (arrow) with intra ventricular extension (curved arrow). (b) Axial CT image of brain is showing chronic SDH in bilateral frontal and parietal regions (arrows)

(a) Axial CT image of PNS in bone window shows concentric mucosal thickening (arrow) in both maxillary sinuses due to sinusitis. (b) Axial T2 weighted MR image of PNS shows concentric mucosal thickening in bilateral ethmoid (arrows) and sphenoid sinuses (curved arrow) due to sinusitis

(a) Axial CT image of brain shows calcified granulomas with perilesional edema (arrow). (b) Contrast enhanced T1 weighted axial MR image is showing a ring enhancing lesion in left parietal region (arrow)

Overall the most prevalent pathology found in the study is paranasal sinusitis which is located in the maxillary sinuses in most of the cases and was coexisting with ethmoid, frontal and sphenoid sinusitis in few cases.
The findings were considered significant in those who presented with headache and associated with other neurological findings (Red flag sign or CWC sign). 29 cases out of 48 (60.4%) in group A as compared to 97 cases out of 452 (21.4%) in group B had positive CT or MRI findings (p-value 0.001 which is highly significant) [Table/Fig-3]. Cases referred from causality, emergency medicine and neurosurgery department yielded more positive results than cases of other departments.
Discussion
The International Headache Society has classified headache broadly into two categories, primary and secondary, primary is without any organic cause and secondary is with an established cause [7]. Primary headache includes migraine, cluster headache and tension headache. For the diagnosis of these types of headaches only clinical assessment are sufficient and no neuroimaging is considered necessary [7].
Although in general headache is 2 to 3 times more common in females than males [8]. Migraine and tension headache are more common in females while cluster headache is the only type of headache that is more common in males than females (M: F ratio is 4:3) [9]. It classically occurs in young to middle-aged males particularly in smokers; with a peak incidence in late 20s. Cluster headache tends to recur during a defined time interval, hence the term ‘cluster’ given.
Many precipitating factors are well known most notably the consumption of alcohol. In a susceptible person stress and climatic changes may be a trigger factor [10].
Various studies have been conducted at different parts of the world at different time to assess the utility of CT and MR Neuroimaging techniques in patients with headache [11–13]. One such study which was conducted at Samsun, Turkey among 70 patients to investigate the incidence of intracranial pathology by CT scanning amongst adult patients who meet Clinical Warning Criteria (CWC) for secondary headaches and to determine the importance of CWC in predicting a possible lesion on CT scan [11]. The CWC is consisting of sudden onset of headache, rise in the frequency and intensity of headache, frequently changing character of headache, no response to analgesics and headache associated with focal neurological symptoms. The results of the study revealed 64.3% of CT scans of head was absolutely normal and 35.7% Scans manifest a positive finding which probably responsible for headache. The rate of detection of positive finding was quite higher among patients who meet CWC criterion [11].
Similar study was conducted at Chitwan medical college, Bhartapur-10 Nepal in 2013 among 256 patients which showed that 73% of patients presenting with headache had no morphological abnormality in CT scans of brain and reported absolutely normal scan [12].
In our study out of total 500 patients, 25.2% patients were diagnosed with a probable cause of headache by CT or MRI scan and 74.8% scan show an absolutely normal scan. In our study 60.4% cases of group A demonstrated an abnormality in CT or MRI scan of brain in comparison to only 21.4% cases of group B.
Another study was conducted among paediatric patients at George Washington University School of Medicine, Washington DC, to evaluate the utility of CT head in the diagnosis of a cause responsible for headache in paediatric patients seeking treatment for headache in the emergency department. The conclusion was that young children presenting with headache with normal neurological examination and insignificant history, CT scans seldom lead to diagnosis or contribute to immediate management [13]. Clinicians should be cautious in advising CT scan in young children to avoid the hazardous radiation exposure in such a young age however MRI is a better alternative in paediatric patients if neuroimaging is essential to reach a diagnosis or to exclude some serious intracranial pathology however cost, cooperation and claustrophobia may be a concern.
MR imaging is not first line imaging technique for the evaluation of patients who presented with chronic or recurrent headache with normal neurological signs. Neither contrast study nor repeated MR imaging contributed to reach the diagnosis of chronic or Recurrent Headache. A study was conducted at Gunma University Hospital of Japan, to evaluate the efficacy of MRI in the diagnosis of an abnormality in patients who presented with chronic or recurrent headache without any neurological deficit. Out of a total of 306 patients, 169 pts (55.2%) had no abnormality in the scan, 135 pts (44.1%) had a minor associated abnormality while only two pts (0.7%) have intracranial pathology which may be culprit of headache [14].
Many such studies have been conducted previously at different institutions and outcome have shown the results that CT is modality of low yield in patients who investigated for chronic headache without any neurological abnormality [15]. Although the majority of patients who present with chronic or recurrent headache in OPD of any general practitioner or hospital without any neurological deficit, many of them use to undergo neuroimaging with CT or MR imaging to exclude any serious intracranial pathology [4,16]. Thus our effort should be to reduce the hazardous radiation exposure before advising CT for headache, as CT scan involves considerable radiation dose.
Maximum cases of our study belong to reproductive age group. Unnecessary CT scan exposes the patient to radiation and its side effect in this vulnerable age group. Because the yield of CT or MRI scans in group A is very significant in comparison to the group B, use of CT /MRI scans must be ethical and selective especially in patients of group B considering the cost and radiation exposure. Neuroimaging is mandatory for the patients suffering from one or more red flag or CWC signs as mentioned above. The associated findings like paranasal sinusitis, calcified granulomas, mild DNS, CSOM and mastoiditis may be incidental findings and falsely increasing the yield of CT.
A patient presented after few episodes of severe headache may harbour considerable anxiety and fear of brain tumour or many other serious diseases which not only badly affect person’s behaviour, psychology and even economic benefit in terms of productivity from their job. The assessment of value for loss is inherently very subjective and difficult to measure. So one practically possible way to do so would be simply ask the patient or relatives how much they would be willing to pay for neuroimaging which would diagnose or exclude significant pathology of brain [17–21].
Weingarten et al., in their study showed that a headache associated with brain tumour may be non-specific and so many times cannot be reliably differentiated from other more common benign causes of headache strictly on clinical grounds so in those cases neuroimaging play an important role to include or exclude the possible cause [22]. Presence of white matter disease is mostly coexisting with chronic hypertension and aging process in most of the cases [23,24] but it may not be primary cause of headache.
Women suffer 2 to 3 times more from primary headache especially migraine than males; this has been proved again in our study. This could be due to hormonal factors. The link between migraine and female sex hormone is well established. Migraine has strong correlation with menstrual cycle, pregnancy, OCP, menopause and HRT [25]. It has been observed in our study that person either male or female belongs to urban area is more prone to primary headache. The reasons responsible for it may be comparatively stressful urban life, noise and air pollution, long hours of driving or transportation, excessive use of electronic devices e.g. mobile phone, television, computer and lack of healthy physical activity which leads to cervical spondylosis and referred headache. Due to better availability of health care and diagnostics facilities in cities and awareness for early treatment; positive detection rate is quite high in urban population while in general, rural population seeks treatment for headache in later stage due to socio-economic causes [26–28].
Our data analysis & results confirm the impression that careful history taking and thorough physical examination is sufficient to exclude major intracranial pathologies and it is cost-effective means for evaluating headache patients with non-focal neurological examinations. CT and MRI both are not suitable as a screening tool and should be reserved for those patients in whom there is a high clinical suspicion of some serious intracranial pathology.
Paranasal Sinus disease is certainly associated with headache in so many cases. MRI and CT are more sensitive for inflammatory changes in the sinuses than plain X-ray but the clinical significance and cost effectiveness of such type of MRI or CT scan is debatable. We have not separated acute and chronic headache in our study because we are primarily interested in determining the impact of CT/MRI on the management of patients presenting with the sole symptom of headache whether it was acute or chronic.
Conclusion
CT/MRI of patients with non-focal headache yields a low percentage of clinically significant positive findings in neuroimaging. The cost-effectiveness of MRI or CT as a screening tool in these patients is having limited value. Neuroimaging of brain is rarely helpful in the diagnosis of headache if it is not associated with other symptoms and /or signs of an intracranial pathology. The reasons for imaging of headache are complex; however, it includes potential psychosocial benefits of a negative test to patient, fear of litigation on treating physician and doubts about the sensitivity of the physical examination. Patients with red flag sign or who meets with clinical warning criteria of secondary headache must undergo for neuroimaging by CT or MRI. In the absence of these, the only reason for CT or MRI scan seems to be reassuring the patients and their loved ones that ‘nothing to worry’ and ‘take the medicine and you will be cured’.