A Prediction Formula for Double Product in Pregnancy
Anita Teli1, Shrilaxmi Bagali2, Ravi Ghatanatti3
1 Assistant Professor, Department of Physiology, KLE’s J N Medical College, Belagavi, Karnataka, India.
2 Assistant Professor, Department of Physiology, BLDEU’s Shri B.M. Patil Medical College, Bijapur, Karnataka, India.
3 Consultant Cardiac Surgeon, Department of Cardiothoracic and Vascular Surgery, KLE’s Dr Prabhakar Kore Hospital and MRCBelagavi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anita Teli, Assistant Professor, Department of Physiology, KLE University’s Jawaharlal Nehru Medical College, Belagavi – 590010, Karnataka, India.
E-mail: anita.v.teli@gmail.com
Introduction
Maternal cardiovascular changes in pregnancy are numerous and increase in double product throughout pregnancy is the part of the same process. Double product is a cardinal surrogate of the myocardial oxygen demand and cardiac workload. It is the product of heart rate and systolic blood pressure and an important determinant of cardiovascular risk in hypertensive patients.
Aim
This study was intended to determine the double product by comparing normal individuals with different trimesters of pregnancy.
Materials and Methods
A cross sectional study was conducted in 220 healthy women in the age range of 18-35 years with 60 subjects each in 1st, 2nd and 3rd trimesters and 40 non pregnant subjects as control group. Cardiovascular parameters were recorded in both the groups. Statistical analysis was done by comparison of parameters using one-way ANOVA and post-hoc by Tukey-Krammer test. Correlation of double product and weeks of pregnancy was done using Pearson’s correlation. Regression analysis was done to know the predictor of double product.
Results
It was observed that there was statistically very highly significant increase (p=0.000) in the double product throughout the pregnancy and duration of pregnancy was found to be the predictor of the product.
Conclusion
The increase in the double product is due to increase in heart rate and stroke volume. Double product is the useful predictor for early identification of preeclampsia and acute myocardial infarction in pregnant women when compared to normal non- pregnant women and hence helps in the early management of complications.
Acute myocardial infarction, Diastolic blood pressure, Heart rate, Myocardial oxygen demand, Systolic blood pressure
Introduction
Pregnancy is the most important and essential physiological adaptation in the body. Overwhelming changes occur virtually in all the systems of the body, modifications in the cardiovascular system are constituent of the same. Systolic and diastolic blood pressures are found to decrease during second trimester. Cardiac output, heart rate and stroke volume tend to increase during pregnancy, thereby reducing the myocardial oxygen demand [1].
Myocardial oxygen consumption is relatively high compared to other organs. High oxygen consumption by the myocardium is required for the contraction and relaxation of cardiac muscle. Hence, the myocardial metabolism and function are closely related [2]. These adaptations during pregnancy are usually well tolerated by healthy women. However, there is a threat to those who are with ischemic heart diseases.
Acute Myocardial Infarction (AMI) is rare in women of child bearing age. But increase in risk of AMI has been shown from 3-4 fold [3–6]. Recent advances in reproduction and child bearing by older women are expected to increase the occurrence of AMI [7].
The double (rate-pressure) product (DP) is an increasingly used surrogate measure of myocardial oxygen demand and cardiac workload. It is systolic blood pressure (SBP) multiplied by heart rate (HR). The strong collation of DP with left ventricular mass has identified it as determinant of cardiovascular risk in hypertensive patients [8,9].
Fick’s principle is used to persuade the myocardial oxygen consumption in human beings, which is an invasive procedure and cannot be performed routinely. DP calculation by multiplying HR and SBP is non-invasive predictor of myocardial oxygen consumption that can be easily used on a larger population [10].
However, there is no previous study on the potential diagnostic use of the DP in pregnancy in our country. So this study was intended to determine the double product by comparing normal individuals with different trimesters of pregnancy.
Materials and Methods
The present cross-sectional study was conducted in the Department of Physiology of a Shri B.M. Patil Medical college and Research center, Bijapur to determine the cardiovascular changes in 1st, 2nd & 3rd trimesters of pregnancy and to compare the results with age matched healthy non pregnant women.
Method of Collection of Data
Study Group comprised of 180 pregnant women in the age group of 18-35 years attending the outpatient department of Obstetrics and Gynecology of a tertiary care hospital. The study group was further subdivided into 3 subgroups. Each sub group comprised of 60 women in 1st, 2nd and 3rd trimesters of pregnancy and Control Group comprised of 40 apparently healthy age matched (18-35 years) non pregnant women. Apparently healthy subjects were included in the study. History taking and thorough clinical examination was done to assess the apparent health status of the subject. Patients with history of cardiovascular diseases, diabetes mellitus, hypertension, tobacco consumption, alcohol intake, endocrine disorders, obesity & moderate to severe anaemia were excluded from the study.
Institutional ethical clearance was obtained. Purpose of the study was explained to the subjects who had volunteered for the study. An informed written consent was obtained. A thorough physical & systemic examination (cardiovascular system) of each subject was done. Recordings were taken between 9 am to 12 Noon. The study was conducted from December 2009 to January 2011.
The following parameters were recorded
Record of Study Parameters: After giving 20mins of rest in supine position, Blood Pressure (SBP and DBP in mmHg) and ECG were recorded. Heart rate was calculated by 1500/R-R interval. The double product was calculated by multiplying SBP by HR (mmHg/min).
Statistical Analysis
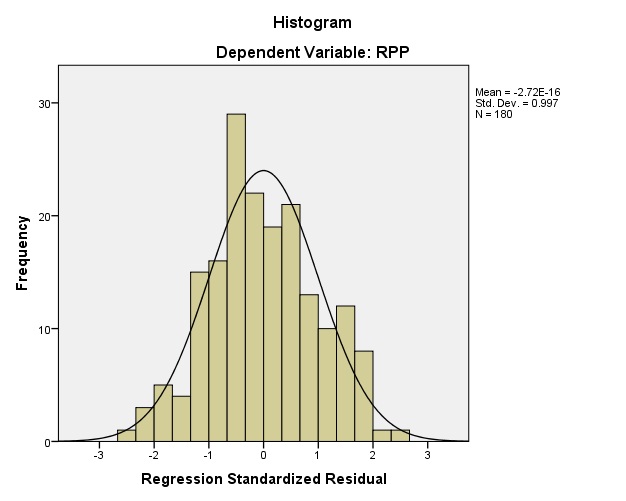
Statistical analysis was done using SPSS 20. Data was analysed for normal distribution [Table/Fig-1]. Comparison of parameters was done using one-way ANOVA and post-hoc by Tukey-Krammer test. Correlation of DP and weeks of pregnancy was done using Pearson’s correlation. Regression analysis was done to know if duration of pregnancy is the predictor of DP.
Blood pressures, heart rates and double products of control and study group subjects.
| Parameters | Group 1(n=40)Control | Group 2(n=60)1st tri | Group 3(n=60)2nd tri | Group 4(n=60)3rd tri | p-values |
|---|
| SBP (mmHg) | 118.6+4.34 | 116.3±7.28 | 109.63±5.53*# | 117.6±7.76 f | 0.000 |
| DBP (mmHg) | 74.0±4.83 | 74.46 ± 6.47 | 66.8±5.03*# | 75.9±7.09 f | 0.000 |
| HR (b/mins) | 75.58±4.17 | 83.38 ± 8.20* | 88.26±8.54*# | 95.7±6.66*#f | 0.000 |
| DP (mmHg/min) | 8998±615.92 | 9692.8±1114.0* | 9626.2±1032.79* | 11237±1007.5*#f | 0.000 |
Data presented are Mean±SD. Analysis of data was done by one-way ANOVA and post-hoc by Tukey- Krammer test. The *depicts comparison with Group 1, # depicts comparison with group 2, the f depicts comparison with Group 3 *p < 0.05, # p < 0.05, f p < 0.05. Group 1 (Control), Group 2 (1st Trimester), Group 3 (2nd Trimester), Group 4 (3rd Trimester). SBP is the systolic blood pressure, DBP is diastolic blood pressure, HR is heart rate and DP is double product.
Results
Mean ± SD of HR, SBP, DBP and double product was calculated and compared using one-way ANOVA test and post-hoc by Tukey-Krammer test and have been tabulated in [Table/Fig-1]. One-way analysis of variance showed a significant difference in heart rate, SBP, DBP and DP between the control group and 1st, 2nd, 3rd trimesters of pregnancy.
Heart Rate: Although heart rate was in the normal range, it was significantly higher during different trimesters of pregnancy compared to the control group. The maximum increase in heart rate was observed in 3rd trimester.
SBP: In comparison with the control groups there was a slight decline in SBP in 1st, 2nd and 3rd trimesters of pregnancy with maximum decline in 2nd trimester.
DBP: In comparison with the control groups there was a decline in DBP in 1st and 2nd trimester of pregnancy with maximum decline in 2nd trimester.
DP: DP was significantly elevated in all three trimesters with peak value in 3rd trimester.
Correlation between Weeks of Pregnancy and DP
On Pearson correlation we observed a significant positive correlation (r = 0.447, p = 0.000) between weeks of pregnancy and DP [Table/Fig-2].
Linear regression analysis model.
| Parameters | R2 | β | Significance |
|---|
| Weeks of pregnancy | 0.200 | 0.447 | 0.000 |
Linear regression analysis was done to predict the value of DP based on duration of pregnancy. We observed that duration of pregnancy was a significant predictor of DP and overall regression model is a good fit for the data [Table/Fig-3,4].
Data showing normal distribution.
Correlation graph of double or rate pressure product and duration of pregnancy.
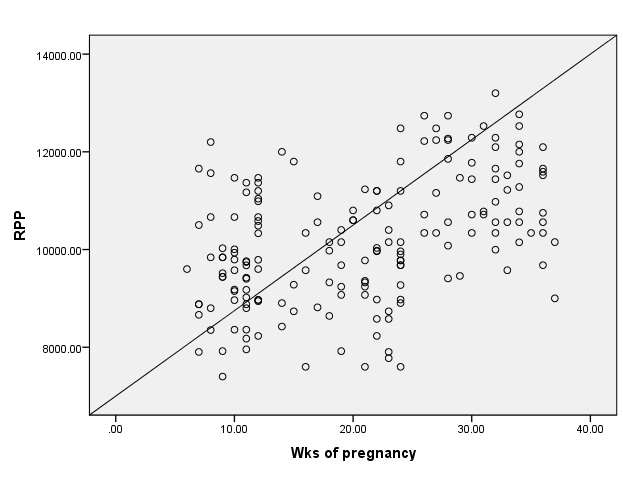
Regression equation: DP = 8891.89 + 62.809 * weeks of pregnancy.
Discussion
Pregnancy is a normal physiological process. There occur widespread adaptations in all the systems during pregnancy. The pregnancy induced changes in the cardiovascular system develop primarily to meet the increased metabolic demands of mother & fetus.
Our study revealed reduction in SBP and DBP in the 2nd trimester of pregnancy compared to control group and also when compared to 1st and 3rd trimesters of pregnancy, which was found to be significant statistically. In the normal course of pregnancy, the blood pressure during the first few months is similar to that of pre-pregnant women. In pregnancy there is usually 6-8% drop in SBP with 20-25% drop in DBP in second trimester. Pressures return to pre-pregnant level at term. The hormones oestrogen, progesterone, prostacyclins and prostaglandin E2 act as vasodilating factors thereby reducing the systemic vascular resistance. In addition decreases in pressures are also due to arteriovenous shunting in placenta [11]. Our study is in agreement with the findings of studies by Schier RW and Voss A et al., [12,13].
Statistically significant increase in the heart rate in all trimesters of pregnancy as compared to non pregnant women was noticed in our study. Heart rate increased by approximately 15% in the 5th week. It increased after 8th week to a maximum of approximately 85-90 beats per minute. There is usually an increase of 10-20 beats per min of heart rate in the last trimester of pregnancy. The increase in heart rate may have been prompted to maintain the cardiac output in a state of relative hypovolaemia [12]. The decrease in the both parasympathetic tone and vagal baroreflex activity are the mainstay for increase in heart rate [13]. The increased heart rate recompense for the fall in the stroke volume resulting from caval compression [14]. Our study was in agreement with the findings of the study conducted by Schier RW [12].
There was statistical significant increase in double product in all trimesters when compared with the control group. The rise was more noticed in the third trimester. The reason is being an enhanced stroke volume and heart rate during pregnancy [1] and also increasing the myocardial oxygen demand.
Oxygen supply to myocardium is decreased during pregnancy due to reduced diastolic blood pressure and physiological anaemia. Myocardial oxygen consumption is increased by 3-folds due to anxiety, pain and contraction of uterus during labour. Above factors may lead to of myocardial ischemia when coronary blood supply is compromised [3].
A study by Ayala D et al., identified Rate Pressure product as one of the cardiovascular risk factor. Their study on hypertensive pregnant women also showed linear increase in RPP throughout gestation until 34 weeks of pregnancy and found values were significantly elevated in complicated pregnancies and computed as the results should be taken into consideration for early identification of preeclampsia in both normotensive and hypertensive pregnant women [8].
Limitation
There are certain limitations to our study; firstly it’s a cross-sectional study whose outcome is not as accurate as longitudinal study. Second because of the conventional blood pressure monitoring in the study the actual blood pressure variation associated with exertion i.e, ambulatory blood pressure monitoring could not be done.
Conclusion
The increase in the double product throughout pregnancy in all trimesters may be useful predictor for early identification of preeclampsia and acute myocardial infarction in pregnant women when compared to normal non- pregnant women. It is the safe and non- invasive test for determination of myocardial oxygen demand and hence helpful for early determination of complications and their management.
Data presented are Mean±SD. Analysis of data was done by one-way ANOVA and post-hoc by Tukey- Krammer test. The *depicts comparison with Group 1, # depicts comparison with group 2, the f depicts comparison with Group 3 *p < 0.05, # p < 0.05, f p < 0.05. Group 1 (Control), Group 2 (1st Trimester), Group 3 (2nd Trimester), Group 4 (3rd Trimester). SBP is the systolic blood pressure, DBP is diastolic blood pressure, HR is heart rate and DP is double product.
[1]. Elkayam U, Gleicher N, Hemodynamics and cardiac function during normal pregnancy and the puerperium. In: Elkayam U, Gleicher NCardiac Problems in Pregnancy 1998 3rd editionNew York, NYWiley-Liss:3-20. [Google Scholar]
[2]. Bagali S, Khodnapur J, Mullur L, Banu G, Aithala M, Aging and gender effects on rate-pressure product: an index of myocardial oxygen consumptionInt J of Biomed & Adv Res 2012 3:175-78. [Google Scholar]
[3]. Roth A, Elkayam U, Acute myocardial infarction associated with pregnancy—an updateAnn Intern Med 1996 125:751-62. [Google Scholar]
[4]. Ladner HE, Danielson B, Gilbert WM, Acute myocardial infarction in pregnancy and the puerperium: A population-based studyObstet Gynecol 2005 105:480-84. [Google Scholar]
[5]. James AH, Jamison MG, Biswas MS, Brancazio LR, Swamy GK, Myers ER, Acute myocardial infarction in pregnancy: A United States population-based studyCirculation 2006 113:1564-71. [Google Scholar]
[6]. Badui E, Enciso R, Acute myocardial infarction during pregnancy and puerperium: a reviewAngiology 1996 47:739-56. [Google Scholar]
[7]. Paulson RJ, Boostanfar R, Saadat P, Pregnancy in the sixth decade of life: obstetric outcomes in women of advanced reproductive ageJAMA 2002 288:2320-23. [Google Scholar]
[8]. Ayala DE, Hermida RC, Fernandez JR, Mojon A, Alonso I, Aguilar MF, Predictable changes in double (rate-pressure) product along gestation in normotensive and hypertensive pregnant womenAm J Hypertens 2003 16(S1):41A [Google Scholar]
[9]. Subha M, Pal P, Pal GK, Habeebullah S, Adithan C, Sridhar MG, Association of sympathovagal imbalance with arterial stiffness indices in women with risk factors for pregnancy-induced hypertension in first and third trimesters of gestationInt J Clin Exp Physiol 2014 1:113-19. [Google Scholar]
[10]. Nagpal S, Walia L, Hemlata Sood N, Ahuja GK, Effect of exercise on Rate Pressure Product in Premenopausal and Postmenopausal women with coronary artery diseaseIndian J Physiol Pharmacol 2007 51(3):279-83. [Google Scholar]
[11]. Niraj Yanamandra, Edwin Chandraharan, Anatomical and physiological changes in pregnancy and their implications in clinical practiceIn: Obstretics and Intrapartum emergencies: A practical guide to management 2012 Cambridge University PressAvailable from: http://assets.cambridge.org/97805212/68271/excerpt/9780521268271_excerpt.pdf [Google Scholar]
[12]. Schier RW, Briner VA, Peripheral arterial vasodilatation hypothesis of sodium and water retention in pregnancy: implications for pathogenesis of pre eclampsia-eclampsiaObstet Gynecol 1991 77:632-39. [Google Scholar]
[13]. Voss A, Malberg H, Schumann A, Wessel N, Walther T, Stepan H, Baroreflex sensitivity, heart rate and blood pressure variability in normal pregnancyAm J Hypertens 2000 13:1218-25. [Google Scholar]
[14]. Julian DG, Wenger NK, Heart disease and heart surgery during pregnancyIn: Women And Heart Disease 2000 United KingdomMartin Dunitz:196 [Google Scholar]