Alcohol Used as Disinfectant before Venipuncture does not Lead to Sample Haemolysis or Sample Dilution
Devajit Sarmah1, Booloo Sharma2, Dilutpal Sharma3, Sheeja Mathew4
1 Associate Professor, Department of Biochemistry, Narayan Medical College, Jamuhar, Bihar, India.
2 Associate Professor, Department of Biochemistry, I Q City Medical College, Durgapur, West Bengal, India.
3 Associate Professor, Department of Biochemistry, King George Medical University, Lucknow, Uttar Pradesh, India.
4 Research Assistant & Laboratory Technician, Department of Biochemistry, R D Gardi Medical College, Agar Road, Surasa, Ujjain, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr Devajit Sarmah, Associate Professor, Department of Biochemistry, Narayan Medical College, Jamuhar, Bihar -821305, India.
E-mail: dr.devajit@gmail.com
Introduction
Sample haemolysis is often the leading cause of sample rejections in clinical laboratory. Isopropyl alcohol or ethyl alcohol, used as disinfectant during sample collection is often considered an important cause of sample haemolysis or sample dilution; although there is a paucity of scientific documentation verifying the same.
Aim
To verify whether avoidance to wipe out alcohol from the venipuncture site, before sample collection leads to sample haemolysis; or leads to sample dilution.
Materials and Methods
This was a prospective randomized study, where every second patient coming to the phlebotomist during the study period, in the age group of 20 to 50 years, was considered for the study. A total of 60 patients were considered for the study. For unbiased comparison sample were collected from both left upper limb (alcohol dry) and right upper limb (alcohol wet) of all the patients. Visual inspection for haemolysis was done, and serum potassium (K), Calcium (Ca), Lactate Dehydrogenase (LDH), Aspartate transaminase (AST), Alanine transaminase (ALT), Alkaline phosphatase (ALKP) and Glucose were estimated in both the set. Also experiences of patients in both limb collections were considered.
Results
On visual inspection none of the sample was haemolysed. 51.67% of the patients experienced same level of discomfort in both limbs (alcohol dry and alcohol wet) during venipuncture. While 28.3% experienced burning sensation in alcohol wet limb, another 20% experienced a more soothing sensation in the alcohol wet limb during venipuncture. There is no statistically significant difference in the measured value of serum K, LDH, Ca, AST, ALT and ALKP and Glucose between the two sets of sample - alcohol dry and alcohol wet.
Conclusion
The study concludes that avoidance to wipe alcohol before venipuncture does not lead to sample haemolysis or sample dilution. Also most patient experienced same or more soothing sensation in alcohol wet limb. Therefore sample can be collected without a waiting period for alcohol to dry off, thereby preventing haemoconcentration and decreasing sample collection time.
CLSI, Dilution, Hemolysis, Isopropyl alcohol
Introduction
Collection of sample is often considered as an important site for pre-analytical errors. Very often unsuitable samples are rejected in a routine laboratory. Of all the causes of sample rejections, haemolysis accounts for 40%-70 % of the unsuitable sample; nearly five times higher than other causes, such as insufficient, incorrect and clotted samples [1–5]. Most of the sample haemolysis occurs during sample collection and transportation or during sample processing. In an effort to minimize the pre-analytical errors the Clinical Laboratory Standards Institute (CLSI), the World Health Organization (WHO), and other allied groups have developed guidelines and protocols to be followed during sample collection, transportation and processing [6–9]. These recommendations are based on available data, although few of these recommendations lack scientific evidence in support.
Almost all available guidelines recommends that the skin at the venipuncture site should be cleaned with a sterile disinfectant (preferably 70% isopropyl or ethyl alcohol) applied to 5 x 5 cm gauze, swab or a cotton ball, using a firm but gentle pressure. Cleansing should start from the centre of the venipuncture site and move downwards and outwards to cover an area of 2 cm or more. After cleaning, alcohol should be allowed to dry completely for up to 30 seconds, or gently removed with clean sterile gauzes after which sample should be collected. This is attributed to two reasons-firstly, alcohol can cause discomfort to the patient and secondly, aspiration of alcohol through the collection needle into blood containers may cause spurious haemolysis of the sample or it can lead to sample dilution, and the sample may become unsuitable [6,7,10]. In India samples are very often collected by untrained phlebotomist who do not usually follow these steps of alcohol cleansing and drying, and also evidence suggests that these recommendations are not always followed elsewhere as well [8,11,12]. If this is the case then we think that most of the sample haemolysis may occur in this step of sample collection. Also, use of alcohol swab is said to decrease the glucose value of the measured sample. So, in order to verify the association of avoidance of wiping alcohol from the collection site and incidence of sample haemolysis or sample dilution we designed this randomized study. The study also proposes to check whether the waiting period of 30 seconds for alcohol to completely dry off from the venipuncture site as recommended, can be avoided.
Materials and Methods
A total of 60 patients coming to the Central Clinical Biochemistry laboratory of RD Gardi Medical College were considered for the study, conducted from July 2014 to February 2015. It was a prospective randomized study, where every second patient coming to the phlebotomist during the study period, in the age group of 20 to 50 years, was considered for the study. Informed consent was taken from all the participants and clearance from the Institutional Ethical Committee was obtained.
Sample collection: Samples were collected from both the upper limbs of the patients. Samples were collected after the venipuncture site in the left upper limb was wiped with 70% isopropyl alcohol (manufactured by Johnson and Johnson, India) and after the area is completely dried off the alcohol (30-35 sec after applying 70% isopropyl alcohol). These samples were labeled as alcohol dry. To make an unbiased comparison sample were again collected after the venipuncture site on the right upper limb of the same individual is cleaned with excess of 70% isopropyl alcohol and before the applied alcohol is dried off (within 5 sec of 70% isopropyl alcohol application). These samples were labeled as alcohol wet. Patients with small or fragile veins were rejected, as collection in such cases can lead to haemolysis of sample. Also, excessive negative pressure during sample collection is avoided, which is also said to induce haemolysis.
Samples were collected using 5 ml of Dispovan disposable sterile syringe manufactured by PH Healthcare Pvt. Ltd., Gujarat, India, and transferred to collecting tubes manufactured by Becton Dickenson India. After removing the needle from the syringe, transfer of sample was done gently through the side of the collecting tube and mixing or shaking of sample tubes were avoided.
Patients were asked for the discomfort experienced during the procedure of sample collection in the left upper limb (alcohol dry) and the right upper limb (alcohol wet).
Visual inspection for haemolysis was done for every sample independently by the three observers.
Serum potassium (K), Calcium (Ca), Lactate Dehydrogenase (LDH), Aspartate transaminase (AST), Alanine transaminase (ALT), Alkaline phosphatase (ALKP) and Glucose were estimated in both the set. Sample were analysed by Vitros-250 dry chemistry analyser, manufactured by Ortho Clinical Division of Johnson & Johnson. To homogenize the procedure and reduce bias all the samples were analysed within one hour of collections.
Statistical Analysis
Results are expressed as mean±SD. Wilcoxon-Mann-Whitney test was used to assess the significance of differences by SPSS software. Statistically significant was considered when p < 0.005.
Results
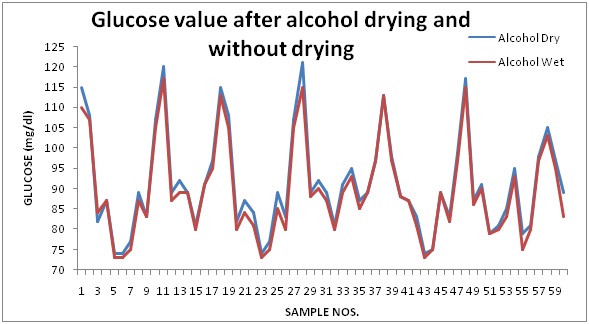
As identified by visual inspection by three independent observers none of the samples underwent haemolysis. When the patients were asked about the difference in their experiences when samples were collected from the left upper limb (alcohol dry) and the right upper limb (alcohol wet), most of the patients admitted that the level of discomfort is same on both the limbs (51.67%), few patients (28.3%) however experienced burning sensation on the right upper limb (alcohol wet) while another 20% experienced a more soothing experience on the right upper limb (alcohol wet) as depicted in [Table/Fig-1]. There was no statistically significant difference in the measured value of serum K, LDH, Ca, AST and ALT between the two sets of sample - alcohol dry and alcohol wet. The results depicted as mean±SD are shown in [Table/Fig-1]. There was no significant difference (p > 0.005) in the measured value of ALKP and glucose between the two sets - alcohol dry and alcohol wet. The results depicted as mean±SD are shown in [Table/Fig-2]. The difference in the values of glucose in alcohol dry and alcohol wet samples are depicted as line diagram in [Table/Fig-3].
Experience of patients during sample collection from both the alcohol dry and alcohol wet limbs.
| Parameter | Number of respondents (%) |
|---|
| Discomfort same in both the limbs | 31 (51.67%) |
| More burning sensation in the alcohol wet limb | 17 (28.3%) |
| More soothing sensation in the alcohol wet limb | 12 (20%) |
Difference in the serum values of the measured parameter of the alcohol dry and alcohol wet samples.
| Parameter | Alcohol dry | Alcohol wet | p |
|---|
| Mean ± SD | Mean ± SD |
|---|
| Glucose | 91.03 ± 12.18 | 89.45 ± 11.76 | >0.005 |
| ALKP | 69.8 ± 17.38 | 69.87 ± 16.87 | >0.005 |
| Potassium | 4.65 ± 0.41 | 4.7 ± 0.4 | >0.005 |
| AST | 33.15 ± 6.65 | 33.56 ± 6.5 | >0.005 |
| ALT | 44.93 ± 31.06 | 43.73 ± 31.53 | >0.005 |
| LDH | 483.15 ± 89.89 | 484.38 ± 90.61 | >0.005 |
| Calcium | 9.73 ± 0.37 | 9.68 ± 0.38 | >0.005 |
Glucose value after alcohol drying and without drying
Discussion
Clinical diagnostic laboratory has attained a considerable importance in modern medical practice. Despite this, clinical laboratories still suffer from age old problems of sample rejections. One of the most important and serious cause of sample rejection is sample haemolysis [1–4]. The protocol of sample collections as suggested by CLSI and others have recommended complete wiping and drying off the alcohol which is the commonest disinfectant used for sterilization [6,7]. But this step of CLSI H03-A6 document prolongs the tourniquet application time leading to venous stasis. Though alcohol has been attributed to cause spurious haemolysis and sample dilution, no published literature conceptually supports this, and our study therefore tries to verify this.
Haemolysis generates a consistent trend towards overestimation of aspartate aminotransferase (AST), alanine aminotransferase (ALT), potassium, calcium and lactate dehydrogenase (LDH). However, the values of alkaline phosphatase (ALKP) and glucose might be substantially decreased, due to dilutional effects [13–16]. Our present study fails to show any significant difference in these parameters tested from the alcohol dry and alcohol wet limbs. Our study correlates with the findings of Salvango et al., who found that alcohol swab does not lead to spurious haemolysis [8]. Usually very small amount of 70% isopropyl alcohol is used for disinfecting the collection site and such a quantity is incapable of causing sample haemolysis or sample dilution. The result of the study suggests that alcohol used as a disinfectant is neither a cause of spurious sample haemolysis nor a cause of sample dilution.
Our present study shows that none of the samples were haemolysed when collected from both the alcohol dry and alcohol wet limb as per the visual inspection for haemolysis done by three independent observers. When asked about the patient’s experiences during sample collection from both the limbs (alcohol dry and alcohol wet), as indicated by table 1, 51.67% of the study participants found no difference in the level of discomfort. While 28.3% experienced increase burning sensation on the alcohol wet limb, 20% however experienced a more soothing feeling on the alcohol wet limb. This suggests that a majority of the participants either experience same or more soothing experience in the alcohol wet limb.
If we summarise the findings of this study we find that avoidance to wipe alcohol before venipuncture is not a source of spurious haemolysis or a cause of sample dilution. So we can ascertain two benefits of such a simple procedure of not waiting for the alcohol to dry off before venipuncture. Firstly, the time for tourniquet application will be reduced which ultimately will avoid local haemoconcentration that may result in erroneous laboratory findings [17]. Secondly, the time of sample collection can be reduced which will be beneficial for high through put centers. Moreover most of the respondents felt same discomfort on the alcohol wet collection as in alcohol dry collection suggesting an easy application of the procedure. The study therefore is thought to decrease the average time of sample collections leading to an increase efficiency of the phlebotomist and in turn prevent unnecessary haemoconcentration due to long duration of tourniquet application. This will also reduce the apprehension of the laboratory personals, who keeps worrying over the sample collection procedure by the phlebotomist.
Limitataion
The small sample size is however a limiting factor for the study, and can be confirmed by a study involving larger participants and with much broader spectrum of laboratory tests.
Conclusion
This prospective randomized study proves that avoidance to wipe alcohol before venipuncture does not result in sample haemolysis or sample dilution. Also, majority of the patients experienced either similar or a more soothing experienced in the limb where collection is done without drying off alcohol. The study therefore indicates that this simple step of not waiting for the alcohol to dry off before venipuncture can be applied routinely, thereby reducing the time of tourniquet application as per CLSI protocol.
[1]. Lippi G, Guidi GC, Risk management in the preanalytical phase of laboratory testingClin Chem Lab Med 2007 45:720-27. [Google Scholar]
[2]. Jones BA, Calam RR, Howanitz PJ, Chemistry specimen acceptability. A College of American Pathologists Q Probes study of 453 laboratoriesArch Pathol Lab Med 1997 121:19-26. [Google Scholar]
[3]. Bonini P, Plebani M, Ceriotti F, Rubboli F, Errors in laboratory medicineClin Chem 2002 48:691-98. [Google Scholar]
[4]. Carraro P, Plebani M, Errors in a stat laboratory: types and frequencies 10 years laterClin Chem 2007 53:1338-42. [Google Scholar]
[5]. Sharma B, Sarmah D, Sonker P, Effect of different anticoagulants on HBA1C estimation and its stabilityJ Lab Physicians 2013 5:143-44. [Google Scholar]
[6]. Clinical Laboratory Standards Institute. Procedures for collection of diagnostic blood specimens by venipuncture; approved guideline – 6th ed. CLSI document H3-A6. Wayne, PA: Clinical and Laboratory Standards Institute; 2007 [Google Scholar]
[7]. World Heath Organization. WHO guidelines on drawing blood. Available at: http://whqlibdoc.who.int/publications/2010/9789241599221_eng.pdf. Accessed: November 10, 2013 [Google Scholar]
[8]. Salvagno GL, Danese E, Lima-Oliveira G, Guidi GC, Lippi G, Avoidance to wipe alcohol before venipuncture is not a source of spurious haemolysisBiochemia Medica 2013 23(2):201-05. [Google Scholar]
[9]. Sarmah D, Sharma B, Nath CK, Fluoride Anticoagulant Vials are Ideal for HbA1c Estimation in IndiaMed-ScienceOnline First: 11 May, 2015. doi:10.5455/medscience.2015.04.8291 [Google Scholar]
[10]. Lippi G, Caputo M, Banfi G, Buttarello M, Cerotti F, Daves M, Recommendations for collection of venous bloodRIMeL/IJLaM 2008 4:249-58. [Google Scholar]
[11]. Lima-Oliveira G, Lippi G, Salvagno GL, Montagnana M, Picheth G, Guidi GC, Impact of the phlebotomy training based on CLSI/NCCLS H03-a6 - procedures for the collection of diagnostic blood specimens by venipunctureBiochem Med 2012 22:342-51. [Google Scholar]
[12]. Simundic AM, Bilic-Zulle L, Nikolac N, Supak-Smolcic V, Honovic L, Avram S, The quality of the extra-analytical phase of laboratory practice in some developing European countries and Mexico - a multicentric studyClin Chem Lab Med 2011 49:215-28. [Google Scholar]
[13]. Guder W, Haemolysis as an influence and interference factor in clinical chemistryJ Clin Chem Clin Biochem 1986 24:125-26. [Google Scholar]
[14]. Sonntag O, Haemolysis as an interference factor in clinical chemistryJ Clin Chem Clin Biochem 1986 24:127-39. [Google Scholar]
[15]. Lippi G, Salvagno GL, Montagnana M, Brocco G, Guidi GC, Influence of haemolysis on routine clinical chemistry testingClin Chem Lab Med 2006 44:311-16. [Google Scholar]
[16]. Dimeski G, Clague AE, Hickman PE, Correction and reporting of potassium results in haemolysed samplesAnn Clin Biochem 2005 42:119-23. [Google Scholar]
[17]. Lima-Oliveira G, Lippi G, Salvagno GL, Montagnana M, Manguera CL, Sumita NM, New ways to deal with known preanalytical issues: use of transilluminator instead of tourniquet for easing vein access and eliminating stasis on clinical biochemistryBiochem Med 2011 21:152-59. [Google Scholar]