Oral mucosal surface lesions may be categorized generally as scrapable or non scrapable, white or red. White lesions are normally seen in the oral cavity and are often found as an incidental finding on routine examination. They may be benign, premalignant or malignant in nature. White, non scrapable lesions include linea alba, leukoedema, frictional keratosis, leukoplakia, oral submucous fibrosis, lichen planus and carcinomas [1].
Due to the fact that some of these lesions may turn in to malignancy affecting the lifestyle and mortality of the patient, all these lesions should be taken seriously and diagnosed based on history, clinical and histopathological findings. Review of the literature has shown that there are very few epidemiological studies on oral mucosal lesions and in particular white lesions. Few prevalence related studies have been done on potentially malignant conditions, rarely correlating their clinicopathologic correlation [2,3].
To the best of our knowledge there is no study on clinico-pathologic correlation of white, non scrapable oral mucosal surface lesions in Southern India, particularly in Andhra Pradesh and ours is the first such correlative study.
Materials and Methods
This clinico-pathologic correlation study included 100 cases of white, non scrapable lesions from various dental colleges in Andhra Pradesh by a single observer. After obtaining institutional ethical clearance and informed consent from all the subjects, a detailed case history of each patient was recorded. Provisional diagnosis was made on clinical examination. For confirmation of the provisional diagnosis, patients were subjected to incisional biopsy and immediately the specimens were sent for processing and histopatholgically examined. Biopsy was performed in all the cases from representative areas and the tissue was fixed in 10% formalin, then the tissue was processed, sectioned and stained with haematoxylin and eosin. The clinico-pathologic correlation was carried out by finding out the discrepancy index.
Interpretation of Staining
All the haematoxylin and eosin stained slides belonging to 100 study cases were observed by two independent observers. They were observed under binocular microscope (Olympus BX51 Research microscope). Each slide was first viewed under low power objective (5X) and then subsequently observed under high power objectives (10X, 40X). All the tissue sections in each slide were scanned and the best one was taken for noting down the findings and giving histopathological diagnosis. The confirmatory histopathological diagnosis was arrived at by the concurrence of two observers.
Results
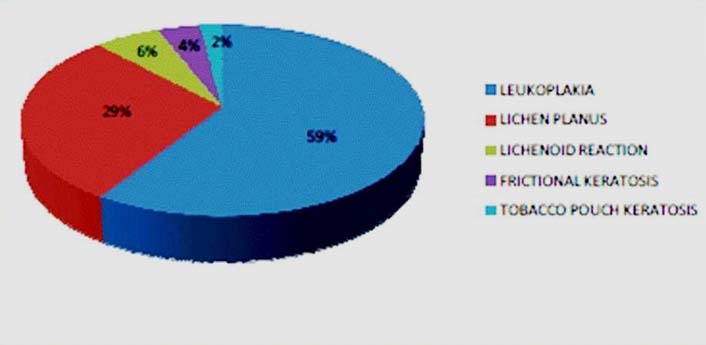
Among 100 cases, 71 cases (71%) were males and 29 (29%) were females. Based on the clinical diagnosis, there were 59 cases (59%) of leukoplakia, 29 cases (29%) of lichen planus, six cases (6%) of lichenoid reaction, four cases (4%) of frictional keratosis and two cases (2%) of tobacco pouch keratosis.
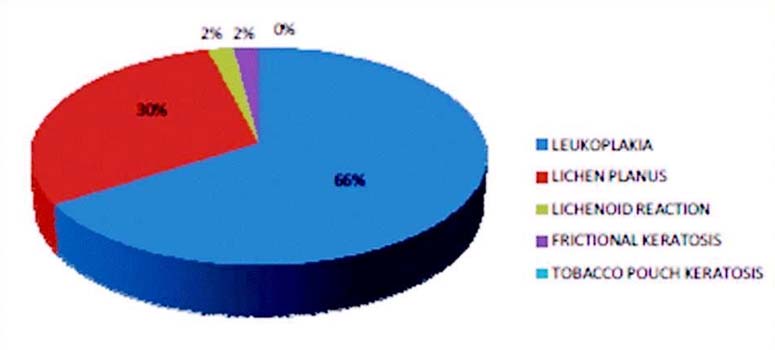
Based on histopathological diagnosis, there were 66 cases (66%) of epithelial hyperplasia and hyperkeratosis (leukoplakia), 30 cases (30%) of lichen planus, two cases (2%) of lichenoid reaction (histologically similar to lichen planus but with known causative agents), two cases (2%) of frictional keratosis (hyperkeratosis without dysplasia) cases [Table/Fig-1,2 and 3].
Total number of cases included in the study and distribution of these cases according to Clinical Diagnosis (CD) and confirmatory Histopathological Diagnosis (HPD).
| Sl.No | Lesion Type | Clinical Diagnosis | Histopathological Diagnosis |
|---|
| 1 | Leukoplakia | 59(59%) | 66(66%) |
| 2 | Lichen planus | 29(29%) | 30(30%) |
| 3 | Lichenoid Reaction | 6(6%) | 2(2%) |
| 4 | Frictional keratosis | 4(4%) | 2(2%) |
| 5 | Tobacco pouch keratosis | 2(2%) | - |
| Total | 100 | 100 |
Graph showing distribution of cases according to clinical diagnosis.
Graph showing distribution of cases according to histopathological diagnosis.
Correlation between clinical diagnosis and histopathological diagnosis.
Among 100 cases included in the study, 78 cases (78%) correlated and 22 cases (22%) did not correlate with the histopathological diagnosis [Table/Fig-4,5].
Distribution of cases based on correlation between Clinical Diagnosis (CD) and Histopathological Diagnosis (HPD).
| S.No | Lesion Type | No. of cases based on CD | No. of CD cases correlated with HPD | No. of CD cases not correlated with HPD |
|---|
| 1 | Leukoplakia | 59(59%) | 54(92%) | 5(8%) |
| 2 | Lichen planus | 29(29%) | 21(73%) | 8(27%) |
| 3 | Lichenoid Reaction | 6(6%) | 1(16%) | 5(84%) |
| 4 | Frictional keratosis | 4(4%) | 2(50%) | 2(50%) |
| 5 | Tobacco pouch keratosis | 2(2%) | 0 | 2(100%) |
| Total | 100(100%) | 78(78%) | 22(22%) |
Graph showing Distribution of cases based on correlation between Clinical Diagnosis (CD) and Histopathological Diagnosis (HPD) and their correlation.
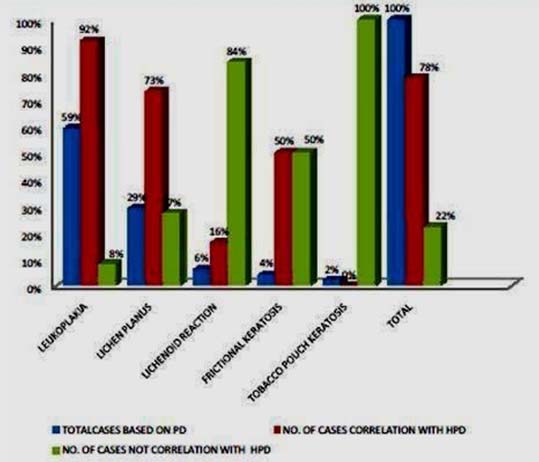
The total discrepancy index (DI) (the number of incompatible diagnosis/the number of total sample) X100 was 22%.
Histopathological diagnosis of non correlating cases
Among 22 non correlating cases [Table/Fig-6],
Histopathological diagnosis of non correlating cases.
| Sno | Lesion Type | Total | Leukoplakia | Lichen planus | Lichenoid Reaction |
|---|
| 1 | Leukoplakia | 5 | - | 5 | - |
| 2 | Lichen planus | 8 | 7 | - | 1 |
| 3 | Lichenoid Reaction | 5 | 2 | 3 | - |
| 4 | Frictional keratosis | 2 | 2 | - | - |
| 5 | Tobacco pouch keratosis | 2 | 1 | 1 | - |
| Total | 22 | 12 | 9 | 1 |
Five cases with a clinical diagnosis of leukoplakia were diagnosed as lichen planus,
Eight cases of lichen planus were diagnosed as seven cases of leukoplakia and one case of lichenoid reaction,
Five cases of lichenoid reaction were diagnosed as two cases of leukoplakia and three cases of lichen planus,
Two cases of frictional keratosis were diagnosed as leukoplakia and
Two cases of tobacco pouch keratosis as one case of leukoplakia and one case of lichen planus.
Discussion
In day to day practice, one should have an adequate knowledge of the incidence and appearance of the most frequently occurring oral lesions, especially the white lesions. With so many additions and modifications of terminologies and classifications, these lesions pose a challenge.
Oral lesions are caused by a wide variety of factors like effects of ageing, trauma, infections, neoplasia, systemic diseases, chemical and thermal agents, habits like areca nut, tobacco, alcohol, etc., [2,4]. These include lesions that show a minor change in colour like linea alba, leukoedema, amalgam tattoo, fordyce’s spots, reactive lesions like frictional keratosis, irritation fibromas, ulcerative lesions like traumatic ulcer, aphthous ulcer, benign lesions like papillomas, potentially malignant conditions like erythroplakia, leukoplakia, oral submucous fibrosis, lichen planus, and neoplastic lesions like oral squamous cell carcinomas [5,6].
“White, non scrapable oral mucosal surface lesions” show an abnormal area of oral mucosa that appears whiter than the surrounding tissue, which cannot be easily removed, usually is slightly raised not exceeding 2-3mm in thickness [6].
They frequently occur as solitary and rarely as multiple lesions, widely varying in size from few mm to cm and appear as papules, plaques or verrucous lesions. The surface of these lesions may be smooth to rough, fissured or wrinkled [7,8].
They generally present a slow, progressive growth pattern, but may also show invasive nature. Most of these lesions can be diagnosed based on their clinical presentation. Cases have been reported where these lesions were wrongly diagnosed after assessing their histo-pathological features. Hence, it is recommended to perform a biopsy for confirming the clinical diagnosis [9].
White, non scrapable lesions are frequently encountered by dental surgeons, dermatologists and ENT professionals. Though many studies on oral soft tissue mucosal lesions have been carried out both in abroad and in India, most of them have been carried out on solitary lesions like leukoplakia or lichen planus or as a whole on premalignant conditions [10–14]. Very few studies have been done solely on oral white, non scrapable mucosal lesions which comprise a major fraction of white lesions.
Our clinico-pathologic correlation study was carried out to study the characteristics of the commonly seen oral white, non scrapable surface mucosal lesions. It included: 1) Leukoplakia; 2) Lichen planus; 3) Lichenoid reaction; 4) Squamous carcinoma; 5) Frictional keratosis; 6) Tobacco pouch keratosis; 7) Hairy leukoplakia; 8) Nicotinic stomatitis; 9) Leukoedema; 10) Verrucous carcinoma [15–18]. Among all the mentioned lesions, we noticed mainly leukoplakia, lichen planus, frictional keratosis, lichenoid reaction and tobacco pouch keratosis. We did not include oral submucous fibrosis cases, considering the fact that it mainly has altered connective tissue rather than epithelial component.
The following observations were noted:
Demographics
With respect to age, a mean age of 40.1 years was found. Whereas Gurung P et al., found mean age to be 50 years in their study [19]. With respect to sex distribution; a predominant male predilection (71 cases, 71%) was noted, with female predilection of only 29 cases (29 %). This observation was similarly noted in few other studies [1,19], whereas Simi SM et al., found a female preponderance in their study [18]. With regard to site distribution, buccal mucosa was the predominant affected site in 68/100 (68%) followed by commissural mucosa (12/100 cases, 12%), palatal mucosa (7/100cases, 7%), gingival mucosa (6/100 cases, 6%), retro molar mucosa (5/100 cases, 5%), tongue (4/100 cases, 4%), alveolar mucosa (3/100cases, 3%), vermilion mucosa (2/100 cases, 2%) and lastly floor of the mouth (1/100cases, 1%). Gurung P et al., also found buccal mucosa as the commonest site in their study [19].
Diagnosis
Based on clinical diagnosis, the most common lesion diagnosed turned out to be leukoplakia (66,66%). This was in accordance with some studies, as most of them were prevalence based studies; comparisons could not be drawn [19,20].
As most of the studies showed leukoplakia as the most common finding and owing to its malignant potential and it being due to consuming tobacco in various forms, educative measures have to be taken both at individual level as well as community level for eradicating it.
Based on histopathological diagnosis, there were 66 cases (66%) of epithelial hyperplasia and hyperkeratoses (with (30%) and without (36%) dysplasia) (compatible with clinical diagnosis of leukoplakia). Our finding was in accordance with few other studies [21–23]. Very few prevalence based studies in this context like that of Bocor Bratic M averts an adequate comparison [20].
Among 100 cases included in the study, 78 cases (78%) correlated and 22 cases (22%) did not correlate with the histopathological diagnosis. The total Discrepancy Index (DI) was 22%, which was more compared to the study of Bocor Bratic M et al., [20].
With regard to correlation between clinical diagnosis and histopathological diagnosis based on individual lesion type,
Among 59 of clinically diagnosed cases of leukoplakia, 54 cases (91%) correlated and five cases (8%) did not correlate, with a DI of 8.47% (5/59X100). Similar studies by and Bokor Bratic M and Onofre et al., showed a higher DI of 17.6% and 24.4 % respectively [20,21].
Among 29 cases of lichen planus, 21 cases (73%) correlated and nine cases (27%) did not correlate with a DI of 31%.
Among 6 cases of lichenoid reaction one case (16%) correlated and five cases (84%) did not correlate with a DI of 83.3%,
Among four cases of frictional keratosis; two cases (50%) correlated and two cases (50%) did not correlate with a DI of 50% and
Among two cases of tobacco pouch keratosis; all cases (100%) did not correlate with the histopathological diagnosis with a DI of 100%.
As survival rate of oral cancers depend on early detection and management, hence a correct diagnosis based on clinicopathologic findings will improve the prognosis of these cases.
Non correlating cases might be due to the fact that few white lesions have overlapping clinical features like frictional keratosis and leukoplakia, lichen planus and lichenoid reaction etc. Hence it is strongly recommended to give a confirmatory diagnosis by correlating clinical and histopathological findings to avert misdiagnoses [22,23].
In our study greater prevalence of tobacco and alcohol consumption was observed in males compared to females. This was in accordance with few other clinical studies [19,20].
Histopathologically, among 66 leukoplakia cases, majority (36/66 cases, 56%) showed a hyperplastic and hyperkeratinised oral epithelium followed by atrophic and hyperkeratinized oral epithelium (23/66, 34%), thus justifying that increase in keratin could make a lesion appear white. Similar observations were made by other studies [1,5]. We noticed mild dysplastic features in 11 cases and moderate dysplasia in seven cases.
Lichen planus lesions were predominant in 3rd, 4th and 5th decades of life, males (60%) were more affected than females (40%), buccal mucosa (90%) was the common site affected followed by palatal mucosa (6%) and our findings were in accordance with many clinical studies [8–10].
Histopathological observations of lichen planus lesions showed an atrophic and hyperkeratinized epithelium (20/30 cases, 67%), followed by hyperplastic and hyperkeratinised epithelium (10/30 cases, 33%) with basal cell degeneration (27/30 cases, 97%). Majority of cases (28/30 cases, 92%) showed exocytosis of inflammatory cells into epithelium, (28/30 cases, 94%) showed intense, sub-epithelial band like predominantly a lympho-plasmacytic infiltrate. Similar observation was noted in few other studies [18,23].
Frictional keratosis was noted in 3rd and 4th decade, males were predominant (3/4 cases), with buccal mucosa (3/4 cases) as the principal site followed by retro molar area (1/4 cases). Histo-pathologically these lesions showed a hyperplastic, hyperkeratotic epithelium with parakeratosis, neither a prominent granular cell layer nor orthokeratosis was observed. Similar observations were recorded by Sudhakar S et al., [24].
Lichenoid Reaction or lichenoid lesions were commonly seen in 37-40 years age group, mainly affecting males (100%), all the cases showed buccal mucosal (100%) involvement. Histo-pathologically these lesions showed an atrophic and hyperkeratotic epithelium and an intense diffuse predominantly lympho-plasmacytic infiltrate. Similar observations were noted by few other authors [12–15].
Owing to very few cases recorded under frictional keratosis and lichenoid reaction adequate comparisons with other clinical studies could not be made.
Conclusion
Our study on ‘correlation of white, non scrapable oral mucosal surface lesions’ is the first study of its kind. An attempt has been made to clearly state what is a “white, non scrapable oral mucosal surface lesion" along with a mention of the lesions comprising this group. The histo-pathological diagnosis given to all lesions in the context of the clinical diagnosis helped in an accurate judgment of discrepancies between clinical and histopathologic diagnoses (DI).
The results of our study proved that a larger sample size would have served the purpose better and in the context of non existence of such studies, more work is needed to be done in near future. A clinician needs to be aware of the importance of all steps in arriving at a clinical diagnosis like proper history taking, thorough clinical observation and invariably needing a confirmative histopathological confirmation. A wrong diagnosis may lead to a wrong treatment, which may not only cause physical trauma to the patient but may also be fatal especially in lesions with malignant potential.
Owing to the serious nature of these potentially malignant conditions, we suggest the use of biologic markers in properly diagnosing them and also suggest that their management should be properly planned based on both clinical and histopathological criteria.