Sialocele of Parotid Duct: Report of Case with Review of Literature
Ravleen Nagi1, Yashoda Bhoomi Reddy Kantharaj2, Rakesh Nagaraju3, Sujatha Janardhan Reddy4
1 Senior Lecturer, Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Sakri, Bilaspur, Chhattisgarh, India.
2 Senior Professor, Department of Oral Medicine and Radiology, Faculty of Dental Sciences, MS Ramaiah University of Applied Sciences, Bangalore, Karnataka, India
3 Reader, Department of Oral Medicine and Radiology, Faculty of Dental Sciences, MS Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
4 Professor and Head, Department of Oral Medicine and Radiology, Faculty of Dental Sciences, MS Ramaiah University of Applied Sciences, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ravleen Nagi, Senior Lecturer, Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Sakri, Bilaspur-495001, Chhattisgarh, India. E-mail : ravleennagi@yahoo.in
Parotid duct sialocele is a salivary cavity arising at the expense of parotid duct. Facial trauma is the most common cause of this rare condition. If left untreated, a sialocele may develop into a significantly large facial swelling. Fistula formation may occur, often draining extraorally. We report a case of Parotid duct sialocele that was assessed by sialography and ultrasonogarphy and was managed by placement of intraductal cannula for fifteen days till duct was found patent. We also discuss various treatment options of this condition in this case report.
Management, Sialography, Ultrasonography
Case Report
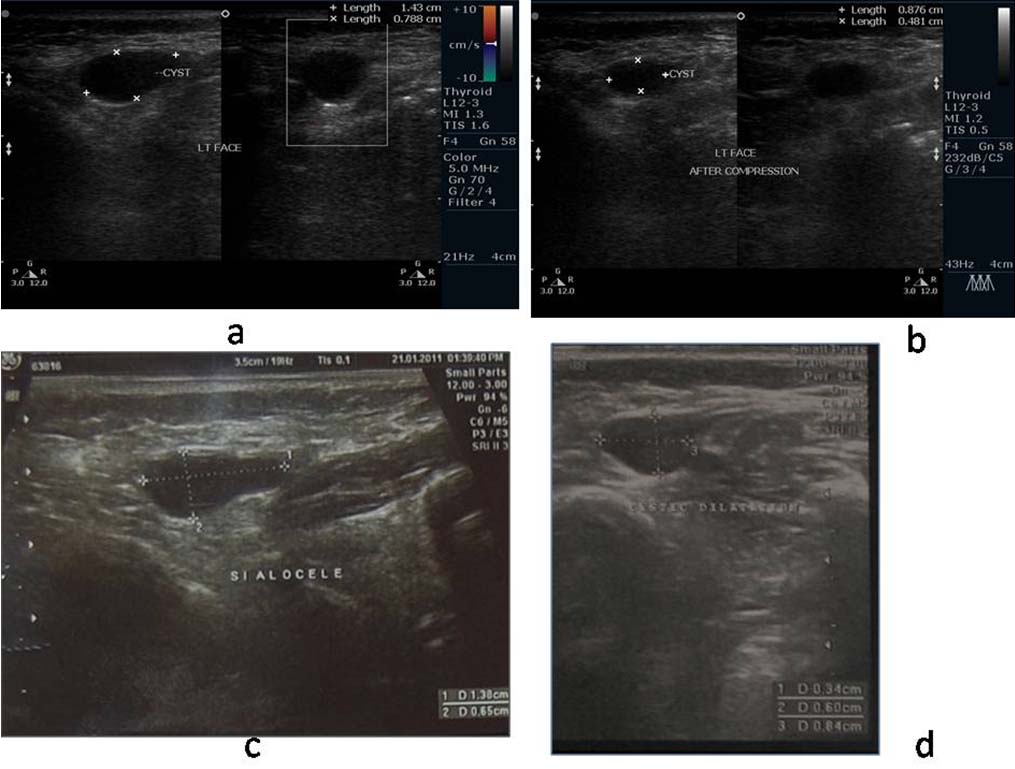
A 37-year-old female patient presented with chief complaint of pain and swelling on the inner side of left cheek region since one year which aggravated on chewing with the involved side. She had history of trauma one year back. Utrasonography [Table/Fig-1] two months back by a referring dentist revealed a well defined thin walled anechoic cyst with bulbous dilatation [Table/Fig-1a&c]. On compression of cyst, the cyst reduced in size [Table/Fig-1b]. Sialography of left parotid duct revealed sausage like appearance [Table/Fig-2]. Based on sialogaraphic and ultrasonographic findings, final diagnosis of sialocele of left parotid duct and sialodochitis was given. Decompression of the siaolocele was done [Table/Fig-3]. Patient was again followed up at two months. Ultrasonography revealed reduced size of bulbous dilatation [Table/Fig-1d]. Sialography revealed well defined radiopacity with decreased accumulation of contrast medium [Table/Fig-4]. There was absence of diverticuli and sialodochitis. Duct was patent with normal salivary flow. Patient was advised to massage the gland after meals and to stimulate salivary secretion by sour substance such as lemon.
a) Ultrasonography shows well defined thin walled anechoic cyst measuring (1.43x 0.78 cm) within layers of the cheek close to left buccal mucosa; b) Ultrasonography shows the cyst reduced in size (0.87x 0.48 cm) after compression; c) Ultrasonography shows mild prominence of left parotid with bulbous dilatation (14x6) mm at its distal end; d) 2months follow up ultrasonography shows size of bulbous dilatation at its distal end reduced to 6x8 mm.
Sialography of left parotid revealed well defined radiopacity i.r.t 26 and 27 with accumulation of contrast media; Dilatation of the duct with constriction proximally was also seen behind posterior border of the ramus of the mandible giving sausage link appearance, sialodochitis (red arrows).

Intraoral photograph showing inserted cannula and removal of cannula after fifteen days.

A 2 months follow up sialography of left parotid duct revealed well defined radiopacity i.r.t 27,37 with decreased accumulation of contrast medium as compared to first visit sialography and absence of diverticuli and sialodochitis.

Discussion
Parotid duct sailocele is a salivary cavity arising at the expense of a parotid duct. They are frequently reported in the literature and are essentially post- traumatic or iatrogenic after superficial parotidectomy. In contrast, only very few cases of parotid duct sialocele have been described, as only seven post traumatic cases were found in a review of English language literature since the 1950s [1]. Diagnosis of sialocele is made on the basis of history and clinical evaluation of the patient. Often the history includes facial trauma or surgery and in some cases ductal stenosis with subsequent dilatation may occur resulting in sialocele [2]. Differential diagnosis of sialocele includes retention cyst, sialodochitis, branchial cleft cyst and lymphoepithelial cyst. However, given a history of facial trauma or surgery diagnosis of sialocele can be made easily [3]. Imaging is required to confirm the diagnosis, to determine the size of ductal injury, size and location of cyst, and to plan management. Fluid collection, hematoma, or a fistula formation in a parotid gland is well demonstrated by high resolution ultrasonography. Conventional sialography may be performed, however some authors have proven that sialography may increase the pressure in the sialocele causing rupture and fistula. Still it has been considered as the mainstay for diagnosis and evaluation of the sialocele [4].
Management of sialocele has been controversial. A variety of surgical and nonsurgical treatment modalities have been proposed for parotid sialocele in the literature. Various conservative approaches are repeated needle aspiration, compression dressings, radiation therapy at 6-20 Gy and anti-sialogogues like atropine or probanthine can be used but their adverse effects limit their use [1]. Botulinum toxin injection has been used to treat parotid sialocele, but has not been reported to be used for treatment of parotid duct sialocele. Various surgical modalities to treat siaolcele are late primary repair or reconstruction of duct, creation of controlled internal fistula, parasympathetic denervation or sectioning of auriculotemporal nerve, duct ligation. Most of these procedures are invasive, often with poor success rates [5]. Another treatment consists of intraoral parotid duct catheterization as performed in the present case with good result and less chance of recurrence.
Conclusion
Parotid gland and parotid duct injuries represent a small percentage of overall soft tissue traumas but dentists must be aware of such injuries preventing onset of complications. Several treatments are currently available for sialocele. Intraoral parotid duct catheterization is a minimally invasive technique providing good results with low morbidity as performed in the present case.
[1]. Singh B, Awasthi PN, Dutta SN, Repair of traumatic pseudocyst of parotid ductJ Indian Dent Assoc 1979 51:89-90. [Google Scholar]
[2]. Parekh D, Glezerson G, Stewart M, Esser J, Lowson HH, Post traumatic parotid fistulae and sialocele a prospective study of conservative management in 51 casesAnn Surg 1989 209:105-11.B. [Google Scholar]
[3]. Canosa A, Post traumatic parotid sialocele: report of two casesJ Oral Maxillofac Surg 1999 57:742-45.1991 [Google Scholar]
[4]. Joffe N, Some sialographic findings in traumatic lesions of the parotid duct and glandAm J Roentgenol 1967 100:656-52..A [Google Scholar]
[5]. Sulabha AN, Sangamesh NC, Warad N, Ahmad A, Sialocele: An unusual case report and its managementIndian J Dent Res 2011 22:336-39. [Google Scholar]