Endodontic Management of a Mandibular Incisor Exhibiting Concurrence of Fusion, Talon Cusp and Dens Invaginatus using CBCT as a Diagnostic Aid
Ruchi Juneja1, Varun Kumar2
1 Senior Resident, Department of Conservative Dentistry and Endodontics, Post Graduate Institute of Dental Education & Research, Chandigarh, India.
2 Consultant Endodontist, Faces n’ Smiles Dental & Orthodontic Clinic, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchi Juneja, H.N. 259/5, Sarai Mohalla, Near Jain Mandir, Rohtak, Haryana-124001, India.
E-mail: ruchijuneja1986@gmail.com
Teeth with aberrant anatomy present a challenge to the endodontist. Advanced tools like cone beam computed tomography aid in exploring the details of endodontic architecture in such cases. The aim of this case report is to highlight the advantage of CBCT in endodontic management of teeth with multiple dental anomalies. A mandibular lateral incisor associated with an extraoral sinus tract revealed unusual clinical anatomy. A provisional diagnosis of type III dens in dente was made based on radiographic findings. Considering the complex anatomy, CBCT was advised to get a confirmatory diagnosis. The anatomic details revealed by CBCT differed significantly from the provisional diagnosis. A final diagnosis of concurrence of fusion with a supernumerary tooth, talon cusp and type II dens invaginatus was established and endodontic treatment of the concerned tooth was carried out. Non-surgical endodontic treatment resulted in successful resolution of the sinus tract and healing of the periapical lesion. CBCT, thus proves to be an excellent diagnostic tool for management of teeth with unusual anatomy, paving way for a conservative treatment free of endodontic mishaps.
Extraoral sinus tract, Root canal treatment, Supernumerary tooth
Case Report
A 22-year-old male presented to Department of Conservative Dentistry & Endodontics, Post Graduate Institute of Dental Sciences, Rohtak, Haryana, India; with pain and swelling in chin region for two days. There was a history of pus discharge from chin region one year back, for which patient consulted a dermatologist. Symptoms resolved at that time with an antibiotic treatment with co-amoxiclav. But the sinus recurred after six months and patient was referred to general surgeon. Surgical drainage and curettage procedure was carried out leading to a remission of symptoms. However, the lesion appeared again after five months. No history of any trauma to tooth or maxillofacial region was reported.
Clinical examination revealed a sinus tract stoma on the chin and swelling in the mental region with frank purulent discharge on application of pressure [Table/Fig-1]. The tooth #42 was mildly sensitive to percussion. No abnormal pocket depths or mobility was detected. Intraoral examination revealed no carious or discoloured tooth. However, mandibular right lateral incisor (tooth 42) was bulky. Presence of an additional cusp like structure on the lingual aspect, indicative of talon cusp was also noticed [Table/Fig-2]. A slight depression with a small dark spot was present in the centre of the tip of this additional cusp, raising the suspicion of an invagination into this cusp. The tooth showed no response to electric and thermal pulp tests.
Preoperative photograph showing a swelling in chin region indicative of mental space infection and cutaneous opening of sinus tract tract with active pus discharge.

Preoperative photograph: occlusal view showing wider mandibular right lateral incisor with talon cusp. Arrow shows the dark spot indicating an invagination.

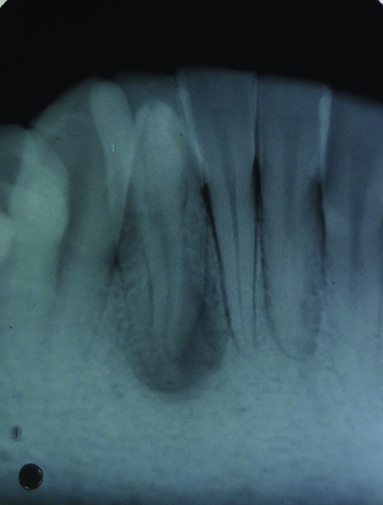
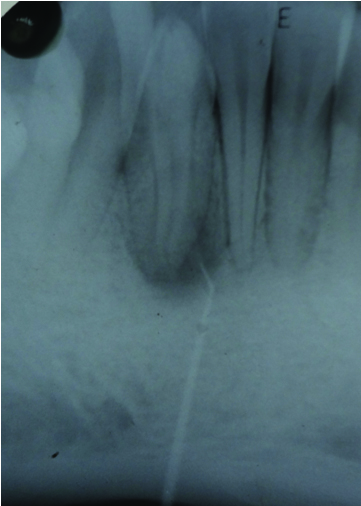
Radiographic examination revealed unusual tooth anatomy, comprising of a radio-opacity in the coronal region and an increase in root width. The appearance was suggestive of type III dens invaginatus. A periapical lesion was also evident [Table/Fig-3]. Tracing with a gutta percha cone confirmed this tooth as the source of infection [Table/Fig-4]. An accurate interpretation of the anatomy of this tooth did not seem possible with this radiographic examination. Therefore, it was decided to obtain a three dimensional imaging of the concerned tooth using CBCT. Informed consent was obtained from the patient, and CBCT was done using i-CAT (Hatfield, Pennsylvania, USA).
Preoperative periapical radiograph showing two root outlines and periapical lesion
Gutta-percha pointing towards #42
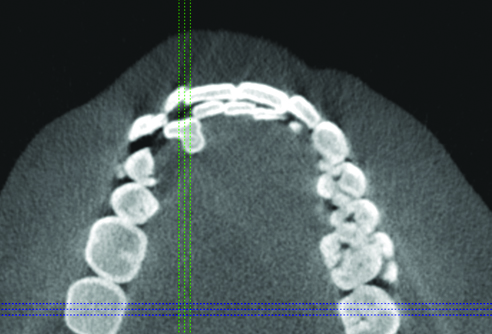
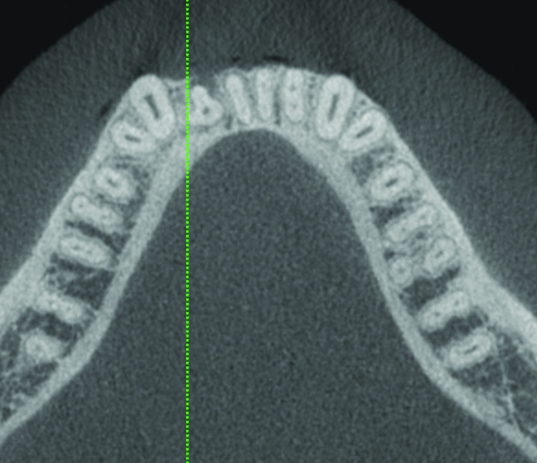
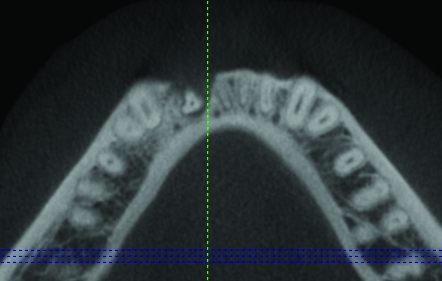
CBCT images in transverse cross-section confirmed dens invaginatus in the middle of the talon cusp [Table/Fig-5]. However, saggital sections revealed that invagination extended from the tip of the talon cusp to cervical third of the root only, hence being a type II dens invaginatus [Table/Fig-6]. The invagination was in close proximity to the pulp chamber and canal, but did not seem to have a direct communication [Table/Fig-7]. The root was much broader mesiodistally when compared to the contra lateral tooth throughout the remaining length [Table/Fig-8,9]. Cross-sections of the root in middle [Table/Fig-8] and apical thirds [Table/Fig-9] depicted that the lingual half of the root was much wider than the buccal half, indicating a possible union with a supernumerary tooth.
Transverse cross-section of crown with CBCT showing dens invaginatus in the middle of talon cusp.
Saggital section with CBCT showing dens invaginatus extending from the most incisal point of talon cusp to cervical third of the root.

Transverse cross-section of dens-invaginatus (CBCT).
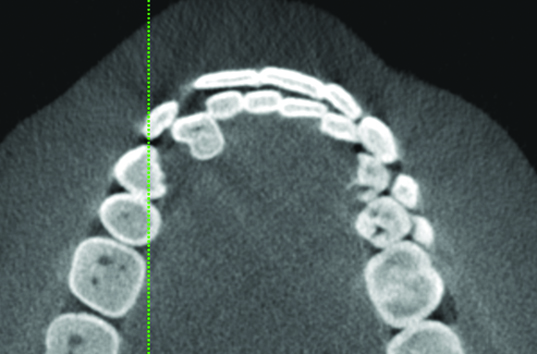
Transverse cross-section of middle third of the root (CBCT).
Transverse cross-section of apical third of the root (CBCT).
Based on clinical and objective findings, a diagnosis of necrotic pulp with chronic suppurative periradicular periodontitis was established and root canal treatment was planned. Access opening was prepared through the talon cusp using dental operating microscope (Carl Zeiss Surgical GmbH, Oberkochen, Germany). The invagination was removed with the Endo Access Bur (Dentsply Detrey, Konstanz, Germany) to obtain direct access to the canal [Table/Fig-10]. After biomechanical preparation, calcium hydroxide was placed in the root canal and the access cavity was sealed temporarily with Kalzinol (DPI, Mumbai, Maharashtra, India). Patient was advised to take an analgesic (Ibuprufen 400 mg) if required. No antibiotic treatment was prescribed. Calcium hydroxide was allowed to remain in the canal for seven days [1]. On the recall appointment after seven days, the discharge had subsided and sinus tract opening had closed [Table/Fig-11]. The tooth was not sensitive to percussion or digital pressure in apical region. Canal was dry without any discharge. Hence, the root canal was obturated with gutta percha with ZOE sealer using lateral condensation technique [Table/Fig-12]. The access cavity was then sealed with resin composite.
Access opening after complete removal of dens invaginatus.

Clinical photograph of the sinus tract at obturation appointment.

Immediate postoperative radiograph.

The patient was recalled for review after six months, and again after one year, and was found asymptomatic. Periapical radiograph showed clear signs of healing [Table/Fig-13,14].
One year follow-up of the patient: clinical view.

One year follow-up of the patient: radiographic view.

Discussion
Fusion is defined as a thorough union of two separate tooth germs. Fusion can occur between two normal teeth or between a normal tooth and a supernumerary tooth. The occurrence of fusion is more common in maxillary anteriors [2,3], while being less frequent in mandibular arch. In a survey involving 9373 teeth, Hamasha and Al-Khateeb could not report any case of fusion in mandibular anterior teeth [4]. Fusion of a mandibular incisor with a supernumerary tooth has only been reported in a few case reports [5–8]. The concurrence of fusion with talon cusp in mandibular anterior region has been sporadically reported [6,9–11]. To the best of our knowledge, the concurrence of fusion and dens invaginatus in mandibular anterior region has been reported only once [12] and the concurrence of fusion, dens invaginatus and talon cusp in a mandibular anterior tooth, as reported here, has not been reported previously.
Intraoral periapical radiographs are two dimensional imaging tools which are not sufficient for accurate interpretation of complex three dimensional anatomy of pulp complex. CBCT has been shown to be useful in assessing the complex anatomy of teeth presenting with endodontic problems [13].
The present case was interpreted as a case of type III dens invaginatus on the basis of radiograph. However, CBCT revealed that invagination extended only up to cervical third of canal, indicating a type II invaginatus. The separate inner and outer root outlines visible in radiograph were actually the result of superimposition of outlines of the narrower buccal half and wider lingual half of the tooth.
The diagnosis of fusion between the permanent mandibular lateral incisor and a supernumerary tooth was done based on the transverse cross-sections of the root. An increased bulk on lingual surface of crown could be explained by a diagnosis of talon cusp. But the root also had an asymmetrical shape throughout its length, with the lingual half being much wider than the buccal half and an intervening invagination, which is non-consistent with the normal root anatomy of a mandibular incisor. The invagination and an increased bulk led to the diagnosis of a possible union of this mandibular lateral incisor with a supernumerary tooth. However, it’s always difficult to establish a differential diagnosis between fusion and gemination; and such teeth are commonly denoted by a neutral term “double teeth” [14]. Fused teeth are generally believed to present with two separate root canals, but a single fused root canal may also be present depending on the stage of development of tooth at which fusion took place [15]. In gemination, one tooth germ divides into two. So, the two teeth are usually mirror images of each other. On the other hand, supernumerary teeth are usually conical or aberrant in shape. Hence, a tooth fused with a supernumerary tooth is less likely to have similar shape of the two parts, as observed in present case [16].
Management of dens invaginatus depends on its severity. In type III cases, dens are treated as a separate canal, and root canal treatment of the invagination is performed [17]. In the present case, it was a type II dens invaginatus which was blocking direct straight line access to the main root canal, and hence it was removed completely with bur to enable its thorough cleaning, shaping and disinfection. Talon cusp in this case was present on lingual side of the tooth. It did not pose any interference in occlusion and was not aesthetically objectionable to the patient. Also, it was self-cleansing and not plaque retentive. Hence, it was not reshaped.
In this case, CBCT helped in providing a deep insight into the anomalous tooth anatomy before beginning any treatment. Moreover, mere adherence to the basic biological principles of endodontic treatment paved the way for a problem-free and successful endodontic treatment resulting in healing of cutaneous sinus tract and periapical lesion.
Conclusion
Accurate preoperative assessment of endodontic architecture is an essential key to success of endodontic treatment. Teeth with developmental anomalies usually have complex canal anatomy. A failure on the part of dentist to identify underlying endodontic architecture in anomalous teeth can lead to various endodontic mishaps and failures. CBCT, in this case, helped in revealing complex tooth anatomy which was not visible in radiograph; and hence aided in a simplified root canal treatment free of any endodontic mishaps.
[1]. Mohammadi H, Dummer PM, Properties and applications of calcium hydroxide in endodontics and dental traumatologyInt Endod J 2011 44(8):697-730. [Google Scholar]
[2]. Atasu M, Cimilli H, Fusion of the permanent maxillary right incisor to a supernumerary tooth in association with a gemination of permanent maxillary left central incisor: a dental, genetic and dermatographic studyJ Clin Pediatr Dent 2000 24(4):329-33. [Google Scholar]
[3]. Gupta SK, Saxena P, Jain S, Jain D, Prevalence and distribution of selected developmental dental anomalies in an Indian populationJ Oral Sci 2011 53(2):231-38. [Google Scholar]
[4]. Hamasha AA, Al-Khateeb T, Prevalence of fused and geminated teeth in Jordian adultsQuintessence Int 2004 35(7):556-59. [Google Scholar]
[5]. Peyrano A, Zmener O, Endodontic management of mandibular lateral incisor fused with supernumerary toothEndod Dent Traumatol 1995 11(4):196-98. [Google Scholar]
[6]. Sachdeva GS, Malhotra D, Sachdeva LT, Sharma N, Negi A, Endodontic management of mandibular central incisor fused to a supernumerary tooth associated with a talon cusp: a case reportInt Endod J 2012 45(6):590-96. [Google Scholar]
[7]. Gupta SK, Gupta J, Acharya SR, Ather A, Mandibular lateral incisor with four root canals: A unique case of double tooth diagnosed using multidetector computed tomographyImaging Sci Dent 2013 43(2):123-28. [Google Scholar]
[8]. Onçag O, Candan U, Arikan F, Comprehensive therapy of a fusion between a mandibular lateral incisor and supernumerary tooth: case reportInt Dent J 2005 55(4):213-16. [Google Scholar]
[9]. Prabhakar AR, Kaur T, Nadig B, Bilateral fusion of permanent mandibular incisors with Talon’s cusp: A rare case reportJ Oral Maxillofac Pathol 2009 13(2):93-96. [Google Scholar]
[10]. Dinesh Rao B, Hegde S, A Talon cusp on fused teeth associated with hypodontia: report of a unique caseEur J Dent 2010 4(1):75-80. [Google Scholar]
[11]. Sharma G, Nagpal A, Talon cusp: A prevalence study of its types in permanent dentition and report of a rare case of its association with fusion in mandibular incisorJ Oral Dis 2014 2014:595189 [Google Scholar]
[12]. Gangawar A, Singal D, Giri KY, Agarwal A, Keerthi SS, An immature type II dens invaginatus in a mandibular lateral incisor with Talon’s cusp: a clinical dilemma to confrontCase Rep Dent 2014 2014:826294 [Google Scholar]
[13]. Patel S, Dawood A, Pitt Ford T, Whaites E, The potential applications of cone beam computed tomography in the management of endodontic problemsInt Endod J 2007 40(10):818-30. [Google Scholar]
[14]. Tsesis I, Steinbock N, Rosenberg E, Kaufman AY, Endodontic treatment of developmental anomalies in posterior teeth: treatment of geminated/fused teeth—report of two casesInt Endod J 2003 36:372-79. [Google Scholar]
[15]. Rajendran R, Developmental disturbances of oral and paraoral structures. In: Rajendran R, Sivapathasundharam B, editorsShafer’s Textbook of Oral Pathology 2007 5th edNew DelhiElsevier [Google Scholar]
[16]. Nunes E, de Moraes IG, de Novaes PM, de Sousa SM, Bilateral fusion of mandibular second molars with supernumerary teeth: case reportBraz Dent J 2002 13(2):137-41. [Google Scholar]
[17]. Bishop K, Alani A, Dens invaginatus. Part 2: clinical, radiographic features and management optionsInt Endod J 2008 41(12):1137-54. [Google Scholar]