Abraham Colle of Dublin, Ireland in the year 1814 was the first to describe what is now commonly known as Colles fracture, he had described it as a fracture lacking the typical characteristic of crepitus and abnormal mobility. He also recognized the high incidence of residual deformity when the fracture had healed and also noted the cases in which the reduction of fracture could be carried out while marking the propensity for the deformity to occur. In his original article Abraham Colles noted that “one consolation that remains is that at some remote period the limb will again enjoy perfect freedom in all its motions and be completely exempt from pain” [1].
The fracture of distal radius was previously known for being common in elderly with low function demand who sustained a low energy trauma. But the incidence of this fracture is increased due to increasing number of elderly population along with increasing number of road traffic accidents and other high energy traumas in all age groups who end up sustaining this fracture [2]. This coupled with the ever increasing demand for perfect reduction and decreased complications in treatment of this fracture among the patients has brought greater significance to the way these fractures are managed.
There are numerous treatment modalities available to orthopaedic surgeons in the treatment of a distal radius fracture; these include closed reduction and casting, closed reduction and percutaneous pinning by different methods such as Kapandiji intrafocal pinning, transradial styloid pinning, pinning via the Listers tubercle or transulnar pinning. Other modalities of treatment include closed reduction and external fixation by means of ligamentotaxis to realign fracture displacement, open reduction by volar or dorsal approach and internal fixation by different implants such as screws, plates, or screws with locking plate [2–4].
While deciding the treatment modality there are numerous factors to consider before finalizing the most appropriate one for each patient, these include the patient’s age, lifestyle, associated injuries, co-morbidities, functional demands, dominance of hand, type of fracture, alignment of fracture, condition of soft tissues, weather the fracture is open or closed and economic constraints of the patient. All these factors play a paramount role in the final decision in the treatment of the distal radius fracture [3,4].
In the elderly the quality of the bones are poor compared to the young and active patients, in these patients it is hard to maintain the distal radius fracture by simple external splintage without any additional support to prevent the collapse. It is in these patients that percutaneous pinning adds the extra support needed to maintain the fracture in desired alignment and reduction [5,6].
Percutaneous pinning is recommended as a simple way of providing additional stability to immobilization in a cast in extra articular fracture of distal radius in which anatomical reduction is obtained by closed reduction [6,7].
To evaluate the radiological outcome of closed reduction and casting versus closed reduction with percutaneous K-Wire fixation and casting in the treatment of the distal radius extra-articular fracture with reference to the restoration of radial height, radial inclination, volar tilt of the distal articular surface and assess the functional outcome of the same measured by the Gartland and Werley demerit scoring system.
Materials and Methods
This prospective randomized control study was conducted on 60 patients attending as out-patient or in-patient at Department of Orthopaedics in our tertiary care center from December 2013 to May 2015 who have been found to have extra-articular fractures of distal radius and fulfill all the inclusion and exclusion criteria.
Inclusion criteria
All patients with radiologically confirmed extra-articular fractures of distal radius (AO types 23-A2, 23-A3), are medically fit, willing for the procedure and consented to be part of the study, are above the age of 18 years and presenting with injuries not older than 2 weeks.
Exclusion criteria
Patients with intra-articular fractures involving radio-carpal joint, Open fractures of distal radius, Distal radius fracture associated with Neurovascular Deficit, Fractures in children and Patients found to be at poor anaesthetic risk are excluded.
Based on the selection criteria: 35 cases of closed reduction and casting and 35 cases of percutaneous k wire fixation were included of which 5 patients in each group were lost to follow up. Sampling was done by simple randomization of the cases done according to a computer generated simple randomization protocol. The data obtained from the two groups was analysed by using unpaired student’s t-test for continuous variables. The results were analysed by SPSS version 20.
The 70 patients were between the ages of 24 years to 73 years with a mean age of 47.45 years. The patients were allocated randomly into two equal groups of 35 patients each as per the simple computer randomization protocol. The first group was treated by closed reduction and cast application and the second group was treated by closed reduction percutaneous K-wire fixation and cast application. Five patients in each group were lost to follow up and hence the final study was conducted with 30 patients in each group and a total of 60 patients.
All fractures were classified by AO classification and only AO type 23-A2 and 23-A3 fracture patterns were included in the study.
Following admission, complete history was noted regarding the mode of injury, severity of trauma. All patients were examined for deformity, swelling, tenderness, bony irregularities of distal radius and relative position of radial and ulnar styloid process were elicited. Movements of the wrist and hand were evaluated. Distal vascularity was assessed. The involved forearm and wrist was immobilized in a below elbow slab and kept elevated. Pain and inflammation were managed with analgesics and anti oedema medications. All routine investigations were done.
Radiographs of injured wrist with forearm in neutral position were taken both in Posteroanterior view and Lateral view. The following radiographic parameters were noted, Radial inclination in PA view, Radial length in PA view, Palmar tilt in Lateral view.
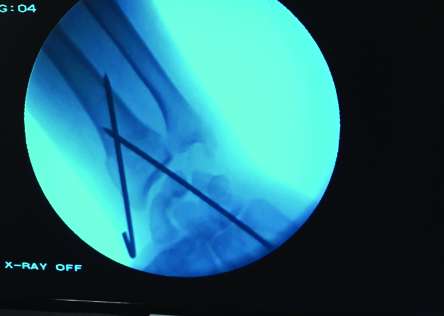
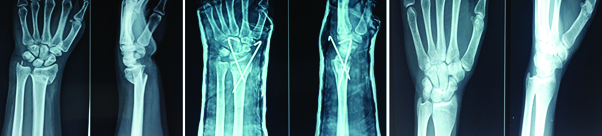
The fracture reduction was carried out under short general anaesthesia (SGA). Reduction was achieved by firm longitudinal traction to the hand against the counter traction by an assistant who grasped the arm above the flexed elbow while the distal fragments were pushed into palmar flexion and ulnar deviation using the thumb of the other hand, the patient’s hand was brought into pronation, palmar flexion and ulnar deviation [Table/Fig-1]. A plaster cast was applied extending from below the elbow to the metacarpal heads, maintaining the wrist in palmar flexion and ulnar deviation (Colles Cast) in the closed reduction group. While in the K wiring group, once acceptable reduction is achieved 1.5 mm K-Wires were passed through the radial styloid process piercing the far medial cortex of proximal fragment under C arm guidance. An additional K-wire was passed through the ulnar side of the radius engaging the opposite cortex when deemed necessary by the operating surgeon [Table/Fig-2,3]. Confirming the satisfactory reduction under C arm, K-Wires were bent and cut, sterile gauze applied beneath the pin. Plaster cast was applied extending from below elbow to metacarpal heads with wrist in neutral.
Closed reduction under C arm guidance.


C arm guided placement of second K-wire.
Postoperative pain and inflammation were managed with analgesics and anti oedema medications and limb elevation. Patients treated with percutaneous K wiring were given Intravenous cefaperazone sulbactum 1.5 grams twice daily for 3 days, followed by oral cefixime 200 mg twice daily, patients were asked to perform active finger movements, elbow and shoulder movements from day one.
Immediate Postoperative check x-rays were taken in both PA and Lateral, the reduction of fracture was confirmed and any displacements were noted. Patients were discharged after three days with routine POP instructions with active finger, elbow and shoulder exercises and followed up after two weeks.
All cases were followed up after two weeks, four weeks and six weeks. They were radiologically assessed for re-displacement. After six weeks K-wires and cast were removed and patients were assessed clinically for fracture union, range of movements and radiological parameters, physiotherapy was advised. After six weeks, regular follow up was done at an interval of three months and six months respectively.
Assessment of Outcome
Functional outcome assessment
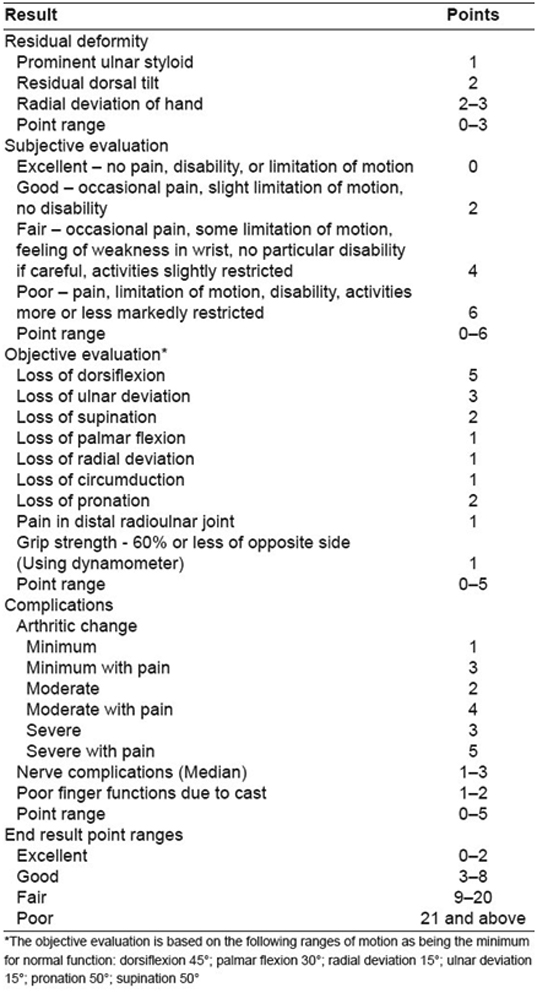
The functional outcome of the patients was assessed at 6 months Postoperative by Demerit score system of Gartland and Werley [7] [Table/Fig-4].
Gartland and Werley demerit scoring system [7].
The functional outcome scores were then compared to ascertain for any statistically valid difference in outcome by an unpaired student’s t-test.
Radiological assessment
The radiological outcome was assessed based on the values of radial height, radial inclination and volar tilt in the PA and Lateral radiographs of the treated wrists and were individually assessed by unpaired student’s t-test to ascertain for any statistically valid difference between the radiological outcome between the two groups.
Results
This study was conducted with a total of 60 patients, 30 patients were each randomly divided into two groups. 30 patients in the first group were treated with closed reduction and casting, 30 patients in group two were treated with closed reduction percutaneous pinning with K-Wires and cast application.
There was no statistically significant difference in the range of movement outcomes between the two groups [Table/Fig-5,6 and 7].
| Palmar Flexion | Dorsi flexion | Supination | Pronation | Ulnar deviation | Radial deviation |
|---|
| Cast application group | 63 | 61 | 64 | 61 | 22 | 16 |
| K-wiring group | 64.5 | 62 | 67 | 64.5 | 23 | 17 |
A patient from the cast application group showing the final range of movements

A patient from the K-wiring group showing final range of movements

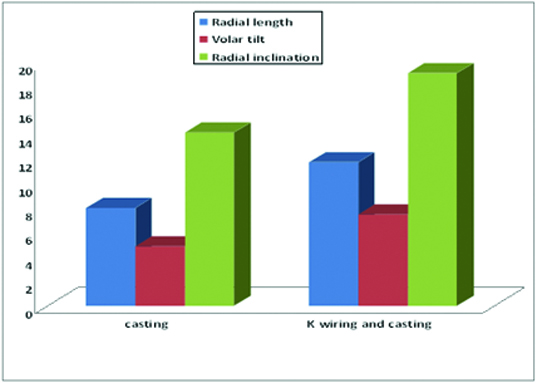
The radiological parameters were assessed for pre reduction, post reduction, 6 weeks post reduction and at 3 months [Table/Fig-8,9 and 10].
Pre Op, Post Op and 6 month follow up X-rays of a patient from the cast application group
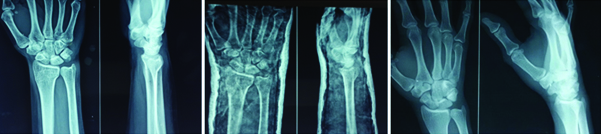
Pre Op, Post Op and 6 month follow up X-rays of a patient from the K-wiring group.
There was a statistically significant difference in all three radiological parameters of the patient groups.
The mean radial height in the casting group was 8.033mm while the mean in the k-wiring group was 11.783mm. The unpaired student’s t-test on the values obtained in both groups revealed a p-value of 0.0001
The mean volar tilt in Cast application group was 4.867 degrees and that in the k-wiring group was 7.5 degrees the unpaired student’s t-test revealed a p-value of 0.0001.
The mean radial inclination in the Cast application group was 14.23 degrees and that in the k -wiring group was 19.1. Unpaired student’s t-test on the values revealed a p-value of 0.0001.
The functional scoring was done as per the Gartland and Werley demerit scoring system [Table/Fig-11].
| Excellent | Good | Fair | Poor |
|---|
| Cast application Group | 13 | 9 | 7 | 1 |
| K-wiring Group | 11 | 13 | 5 | 1 |
The Cast application group had thirteen excellent, nine good, eight fair and one poor result the mean outcome score of the group was 5.2.
The K wiring group had eleven excellent, thirteen good, five fair and one poor result, the mean score of the group was 5.17.
The unpaired student’s t-test on the values obtained from both groups yielded a p-value of 0.9816.
Indicating that statistically there was no significant difference in the functional outcome between the two groups.
Discussion
Fractures of distal radius are common injuries encountered in orthopaedics, especially with increasing number of low energy fractures in elderly, the other contributing factor is the ever increasing cases of road traffic accidents [2]. Also, as the average life expectancy is increasing, orthopaedic surgeons will need to focus on treating osteoporotic fractures, particularly those in post menopausal women as noted by Young et al., [5].
Studies by Jupiter et al., and Cooney et al., have suggested that there is a direct relationship between anatomical result and functional outcome [2,3].
Walton et al., presented a method of holding unstable distal radius fracture with blunt ended K wires via intrafocal and intra medullary insertion, so modifying the Kapandji technique, 102 patients were treated with unstable distal radius fractures in this way and according to clinical need and scored radiologically and functionally using modified Lidstrom scoring system. They presented this as a reliable and useful method in treatment of these common fractures particularly in osteoporotic bones [8].
Kurup et al., conducted a study of 56 patients. They found that distal radius fractures treated by percutaneous K wire fixation, did not suffer significant loss of reduction of fracture position after removal of the pins. This remains true regardless of age, sex and fracture type according to AO type or duration of wire fixation [9].
Hashmi et al., conducted a study to assess the results of modified Kapandji wiring technique in unstable fractures of distal end of radius. They concluded that Kapandji wiring can be performed as a primary treatment for distal radius fracture. The indication for K wire osteosynthesis in a secondary displacement of a fracture that was initially reduced and held in plaster. Kapandji technique is one of the better treating options of an unstable Colles fracture, it results in a decreased time spent in plaster casts, better stability of a fracture fragment and an early rehabilitation with good postoperative range of motions and is easy to perform [10].
While anatomical reduction can usually be achieved by closed manipulation, there is still no clear consensus on the most appropriate method of maintaining the fractures. Studies by Walton et al., Hashmi et al., and Kurup et al., have been conducted with the use of percutaneous K wiring for stabilization of distal radius have been published. All claimed good results, but with the lack of controlled trials no clear consensus can be drawn [8–10].
Azzopardi et al., conducted a prospective randomized study of immobilization in cast versus supplementary percutaneous pinning and concluded that percutaneous pinning provides only a marginal improvement in radiological parameters compared to immobilization in cast alone, although this does not translate into improved functional outcome in elderly population [11].
Das AK et al., conducted a prospective study of 32 patients aged between 18 to 70 years with extra articular distal radius fracture. Patients were treated with closed reduction and percutaneous pinning using two to three K wires. They concluded that percutaneous pinning followed by immobilization of wrist in neutral position is a simple and effective method to maintain reduction and prevent stiffness of wrist and hand [12].
RR Bagul et al., conducted a prospective study of 30 cases where comparative evaluation in the measurement of the radial height, radial inclination, and ulnar variance in fracture distal end of radius treated with closed reduction and casting and closed reduction K wire fixation and casting. They concluded that the K wiring and casting group stands an upper hand over the closed reduction group for fractures of distal radius with respect to the near anatomical restoration of radial height, radial inclination and ulnar variance [13].
Our prospective randomized control study compared closed reduction and below elbow cast immobilization and closed reduction with percutaneous K wiring and below elbow cast immobilization of extra articular fractures of the distal radius (AO class 23-A2 and 23-A3). Both groups were immobilized for a period of six weeks in well moulded below elbow cast. Studies by Jupiter and Sahin have shown no advantage of above elbow casting [2,14].
There was a statistically significant difference in all three radiological parameters of the patient groups. The mean radial height in the Cast application group was 8.033mm while the mean in the K-wiring group was 11.783mm, the unpaired student’s t-test on the values obtained in both groups revealed a p-value of 0.0001. The mean volar tilt in Cast application group was 4.867 degrees and that in the K wiring group was 7.5 degrees, the unpaired student’s t-test revealed a p-value of 0.0001. The mean radial inclination in the Cast application group was 14.23 degrees and that in the K wiring group was 19.1. Unpaired student’s t-test on the values revealed a p-value of 0.0001, this was in line with other studies of similar nature conducted by Azzopardi et al., Das AK et al., and RR Bagul et al., which also concluded the same [11–13].
The functional outcome in our study was assessed by demerit score system of Gartland and Werley unlike other studies like the one by Wong [6] which used activities of daily life or Azzopardi [11] who used Mayo wrist score. In the present study, statistically there was no significant difference in the functional outcome between the two groups.
Limitations
The limitations of our study are in the number of patients i.e, only 30 patients in each group and a total of 60 patients were included in the study, a greater number of patients would have reduced the chances of any statistical error even further. The other shortcoming was the short follow up, as it was limited to 6 months. A longer follow up would have shown any late arthritic changes of the wrist and may have given a more conclusive result.
Conclusion
It can be concluded that closed reduction with percutaneous K wiring and below elbow cast application is a simple, minimally invasive technique that provides added stability and better radiological outcome with respect to treatment of extra-articular distal radius fracture as compared to closed reduction and below elbow cast application, but the functional outcome between the two treatment modalities is not statistically significant.