Gastric Trichobezoar with Rapunzel Syndrome: A Case Report
Anoop Dixit1, Mohd Arshad Raza2, Rohit Tiwari3
1 Post Graduate Student, Department of General Surgery, RMCH, Bareilly, (U.P.), India.
2 Associate Professor, Department of General Surgery, RMCH, Bareilly, (U.P.), India.
3 Post Graduate Student, Department of General Surgery, RMCH, Bareilly, (U.P.), India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mohd Arshad Raza, Associate Professor, Department of General Surgery, Rohilkhand Medical College and Hospital (RMCH), Bareilly-243006, (U.P.), India.
E-mail: drarshadraza@gmail.com
Bezoars are collections of non-digestible matter that usually accumulates in stomach and can extend to small bowel. Trichobezoars (concretions of hair) are unusual and are usually found in young psychiatric females, who often deny eating their own hair (trichophagy). We are presenting a case of gastric trichobezoar with a long thin tail in a 20 years young female with a history of trichophagia. Patient was managed by exploratory laparotomy and anterior gastrotomy. Postoperatively she recovered well and was discharged in satisfactory condition with advice for psychiatric follow-up.
Bezoar, Gastrotomy, Trichophagia
Case Report
A 20-year-old married female patient presented with chief complaints of off and on vomiting for six months, progressive loss of appetite for four months, pain and lump in abdomen for two months. On general physical examination, the patient was thin built well looking female with normal basal parameters. Abdominal examination revealed a well defined, smooth and hard intrabdominal lump of 8 x 10cm in the epigastric region. The lump was having palpable curved (convex) lower border but upper border not reachable (fingers could not be insinuated between the lump and costal margin). The lump was moving with respiration and dull on percussion. Differential diagnosis of gastric trichobezoar and gastric malignancy was made clinically. Abdominal ultrasound showed a large mass in the epigastric region with echogenic anterior margin.
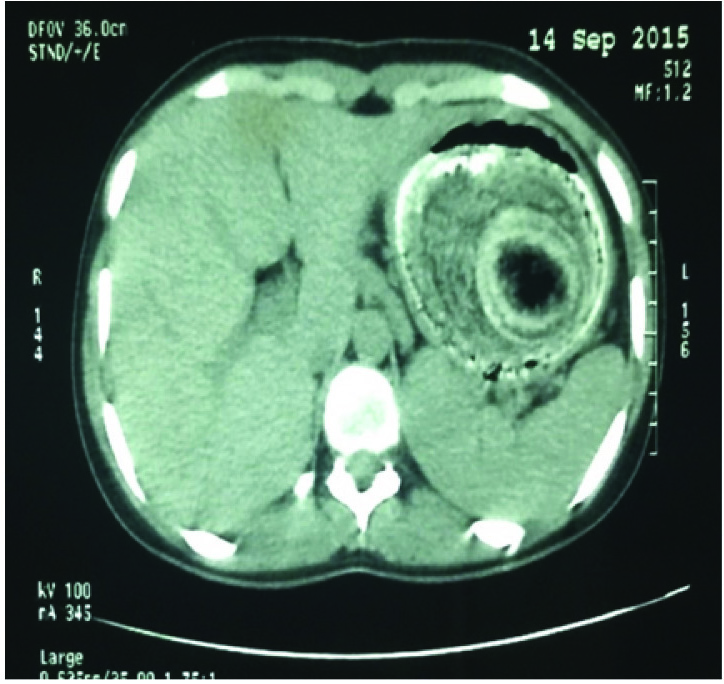
Contrast Enhanced Computed tomography (CECT) showed grossly distended stomach with heterogenous intraluminal content showing areas of curvilinear band like hyper densities and scattered lucencies suggestive of Gastric Trichobezoar [Table/Fig-1].
A well-circumscribed lesion, composed of concentric whorls of different densities with pockets of air enmeshed within it, appears in the region of stomach.
Prompted by the investigations, we enquired further, to which she admitted about habit of hair eating for last one year.
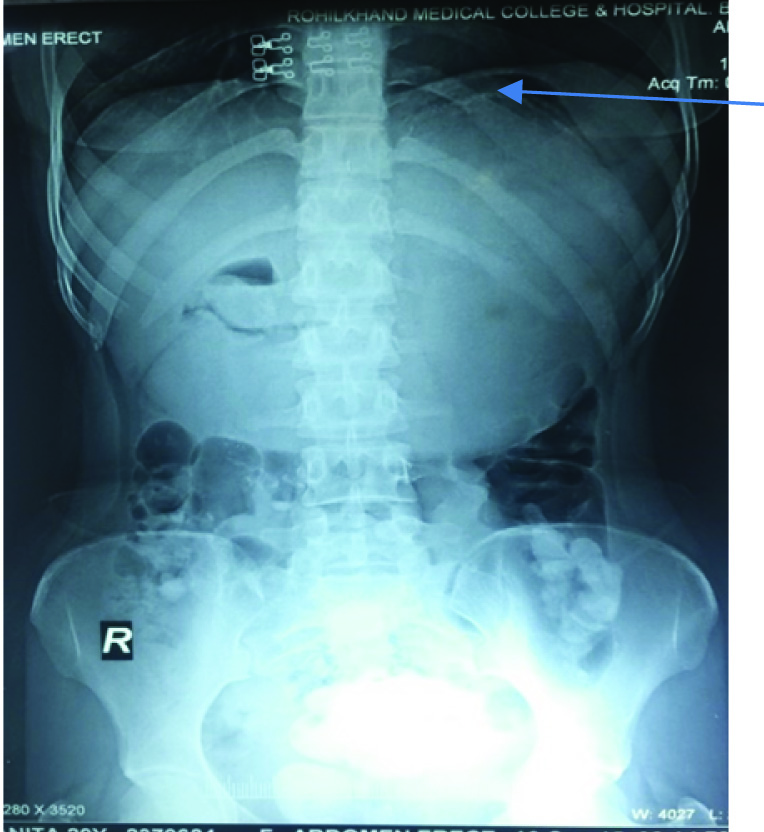
For our clinical interest we also asked for X-ray abdomen-AP erect [Table/Fig-2] which is showing ragged upper margin of lump depicting upper border of Trichobezoar.
Plain X-ray abdomen AP erect view.
Based on the above findings we decided to perform surgery for the trichobezoar. Hospital psychiatrist was consulted for evaluation of any associated psychiatric illness and counselling/treatment. An informed consent was taken from the patient and her husband. Trichobezoar was removed by upper midline Exploratory Laparotomy with anterior gastrotomy under GA [Table/Fig-3,4].
A hair ball occupying the whole stomach.
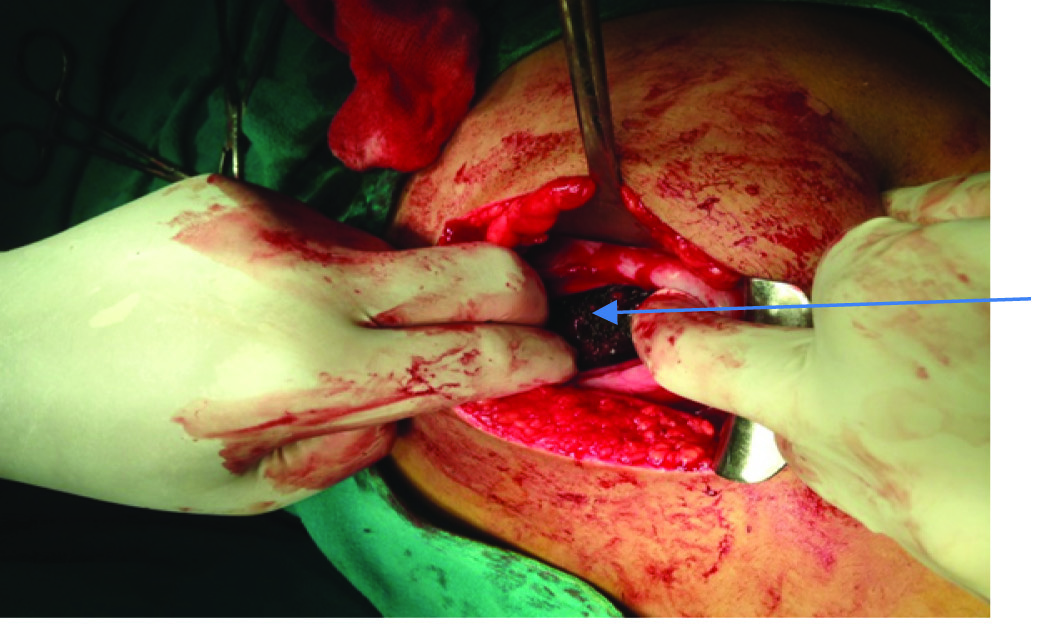
Main mass of hairs during the act of removal

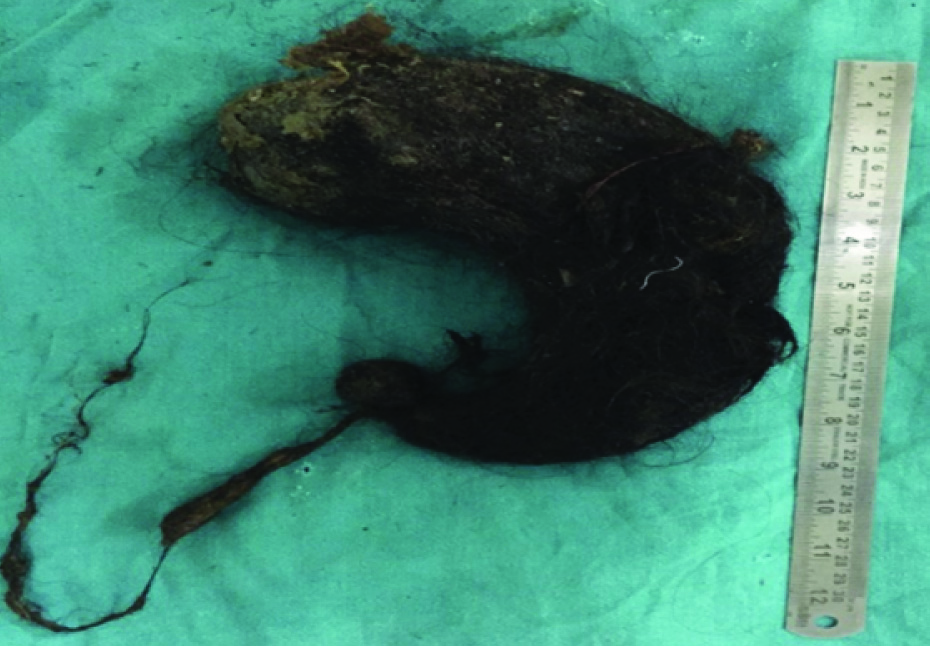
A giant trichobezoar was removed through an anterior gastrotomy along with its tail (Rapunzel syndrome). Gastric mucosa inspected but there was no sign of any complication (ulceration, haemorrhage etc.). The mass weighed 1950 g and measured 23x17 cm [Table/Fig-5].
Specimen of Rapunzel syndrome with large hair ball taking the shape of stomach and tail recovered from duodenum and jejunum.
The gastrotomy was closed in two layers and the abdomen was closed with drainage. Postoperatively patient recovered well, allowed orally on 5th post-op day, skin stitches removed on 10th post-op day and patient discharged from hospital in satisfactory condition.
A psychiatric evaluation diagnosed her having an adjustment disorder. She was discharged with advice for psychiatric follow-up to avoid recurrence.
Discussion
Bezoars are collections of nondigestible matter that usually accumulates in stomach and can extend to small bowel. Different types of bezoars are Phytobezoar (vegetable origin), Trichobezoar (composed mainly of hair), Lactobezoar (concentrated milk formula), Pharmacobezoar (mixed medicine bezoars), and food bolus bezoars. Trichobezoars (concretions of hair) are unusual and are usually found in young psychiatric females, who often deny eating their own hair (trichophagy). It is caused by the pathological ingestion of hair, which remains undigested in the stomach [1]. Human hair is resistant to digestion and peristaltic movement because of its smoothness. Continuous ingestion of hair, over a period of time, can lead to their impaction along with mucus and food material into the stomach. In some cases, however, the trichobezoar extends through the pylorus into jejunum, ileum or even colon. This condition, called Rapunzel syndrome, was first described by Vaughan et al., in 1968 [2]. Bezoars may present with abdominal pain, nausea/vomiting, early satiety, weight loss, intestinal obstruction, ulceration leading to bleeding and/or perforation. Rarely intussusception can also happen [3]. Our patient presented with off and on nausea, progressive loss of appetite, upper abdominal pain and lump.
An upper abdominal mass remains the commonest presenting sign [4]. In our case also there was a palpable intraabdominal lump in epigastric region which was moving well with respiration and hard in consistency with curved (convex) lower border.
Diagnostic modalities include US, CT scan and upper endoscopy. CT scan has a high accuracy rate, but the accuracy of US in such cases is not so high [5]. The diagnosis is made easily at endoscopy or, indeed, from a plain radiograph [1]. We also diagnosed and confirmed our case with US, CT and plain radiograph.
Although a psychiatric trouble is usually present, this is not always the case as the syndrome may affect healthy women [6,7].
Firm or hard masses in the mid upper abdomen are usually suspected for malignant processes, especially in adults and in old age. Trichobezoar should be considered as a differential diagnosis in young females who present with either history of ingestion of hair or complain of epigastric pain, weight loss and epigastric mass.
Management options include endoscopic removal, laparoscopic removal, or via laparotomy. Gorter et al., in a retrospective review of 108 cases of trichobezoar, evaluated the variable treatments tried in these cases; it was noted that whereas 5% of attempted endoscopic removals were successful (small trichobezoars may respond to endoscopic fragmentation and vigorous lavage), 75% of attempted laparoscopic surgical extractions were successful. However, laparotomy followed by gastrotomy was 99% successful and thus favoured as their management of choice [8]. We also managed our case by laparotomy and anterior gastrotomy. Medical treatment as enzyme therapy with papain, cellulase, or acetylcysteine may be tried but usually ineffective [7,9]. So non-operative treatments are discouraged because of high failure rate.
Conclusion
Although rare, trichobezoars, should not be forgotten as a differential diagnosis in young females presenting with vague upper abdominal complaints and an epigastric lump. Complications are not infrequent, a diagnosis of trichobezoar and its treatment well in time will prevent these complications. Also, recurrences are known. A psychiatric evaluation, counselling and treatment are helpful in preventing these recurrences.
[1]. John NP, Timothy JU, Stomach and duodenum. In: Williams NS, Bulstrode CJK, O’Connell P.R. edsBailey and Love’s Short Practice of Surgery 2013 26th edBoca Raton, FLCRC Press:1023-1057. [Google Scholar]
[2]. Vaughan ED, Sawyers JL, Scott HW, The Rapunzel syndrome. An unusual complication of intestinal bezoarSurgery 1968 63:339-43. [Google Scholar]
[3]. Dalshaug GB, Wainer S, Hollaar GL, The Rapunzel syndrome (trichobezoar) causing atypical intussusception in a child: a case reportJ Pediatr Surg 1999 34(3):479-80. [Google Scholar]
[4]. Debakey M, Oschner A, Bezoars and concretions: Comprehensive review of literature with analysis of 303 collected cases and presetitations of 8 additional casesSurgery 1939 5:132-60. [Google Scholar]
[5]. Sharma Y, Chhetri RK, Makaju RK, Chapagain S, Shrestha R, Epigastric mass in a young girl: trichobezoar. Imaging diagnosisNepal Med Coll J 2006 8:211-12. [Google Scholar]
[6]. Salaam K, Carr J, Grewal H, Sholevar E, Baron D, Untreated trichotillomania and trichophagia: surgical emergency in a teenage girlPsychosomatics 2005 46:362-66. [Google Scholar]
[7]. Coulter R, Antony MT, Bhuta P, Memon MA, Large gastric trichobezoar in a normal healthy woman: case report and review of pertinent literatureSouth Med J 2005 98:1042-44. [Google Scholar]
[8]. Gorter RR, Kneepkens CMF, Mattens ECJL, Aronson DC, Heij HA, Management of trichobezoar: case report and literature reviewPediatric Surgery International 2010 26(5):457-63. [Google Scholar]
[9]. Jensen AR, Trankiem CT, Lebovitch S, Grewal H, Gastric outlet obstruction secondary to a large trichobezoarJ Pediatr Surg 2005 40:1364-65. [Google Scholar]