Acute appendicitis is one of the most common surgical conditions that are diagnosed in children presenting with acute abdominal pain in the emergency department. An atypical presentation of symptoms is encountered in 30% of cases. Atypical localization of the appendix as in left sided appendicitis, although rare, has an increased risk of missed or delayed diagnosis. We present two consecutive cases of left sided appendicitis in order to describe how increased awareness in the second case helped us to avoid pitfalls in the management and diagnosis of this atypical and variant condition. Increased cautiousness and awareness of left sided appendicitis can assist emergency physicians to avoid pitfalls in the management and diagnosis of this atypical and variant condition.
Appendectomy, Abdominal pain, Misdiagnosis
Case Report 1
An eight-year-old female patient visited our ED complaining of continuous abdominal pain starting 2 days ago. Associated symptoms included fever reaching 37.8oC, nausea and anorexia. Physical examination revealed right and left abdominal tenderness and guarding more of the right lower abdominal quadrant. Laboratory investigation revealed leukocytosis with a shift to the left and increased CRP value. Imaging investigation was performed by abdominal ultrasound (U/S) that did not reveal any finding that was pathognomonic for acute appendicitis or any other surgical condition but rather excluded any pathology from other parenchymal organs and the internal genitalia. Strangely, as proved later, ultrasound at that point did not identify any suggestive findings of intestinal malrotation.
The child was clinically diagnosed with acute appendicitis and was prepared for her operative management by an open appendectomy with a right lower transverse incision. Surprisingly, the cecum and ileocecal valve were not located in their typical position in the right iliac fossa but were identified to the left of the midline. We were forced to lengthen the incision to the midline to deliver them into the wound and we noticed that the ileocecal valve was localized to the right of the cecum. At that time the suspicion of possible intestinal malrotation emerged. After completion of the appendectomy the small intestine was thoroughly investigated and was found to have a broad mesentery so no further intervention was made.
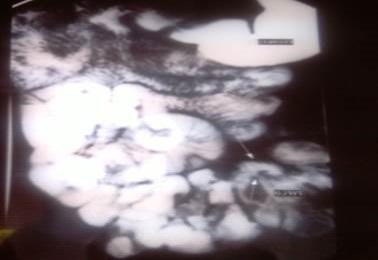
The postoperative period was uneventful and further imaging investigation for possible malrotation was performed. Repetition of abdominal U/S revealed reversal of the anatomic relationship of the superior mesenteric vessels while upper gastrointestinal (GI) series showed the cecum and ascending colon to be located in the left iliac fossa [Table/Fig-1]. The diagnosis of intestinal malrotation type Ia was confirmed and the child was discharged from the hospital. On discussion with our radiologists, it was concluded that right sided symptomatology, minimal suspicion of the disease and possibly decreased experience of the radiologist on-call contributed to the negative identification of intestinal malrotation in the initial ultrasound investigation.
GI series showing small bowel in the right abdomen and cecum and ascending colon in the left abdomen (arrows).
Case Report 2
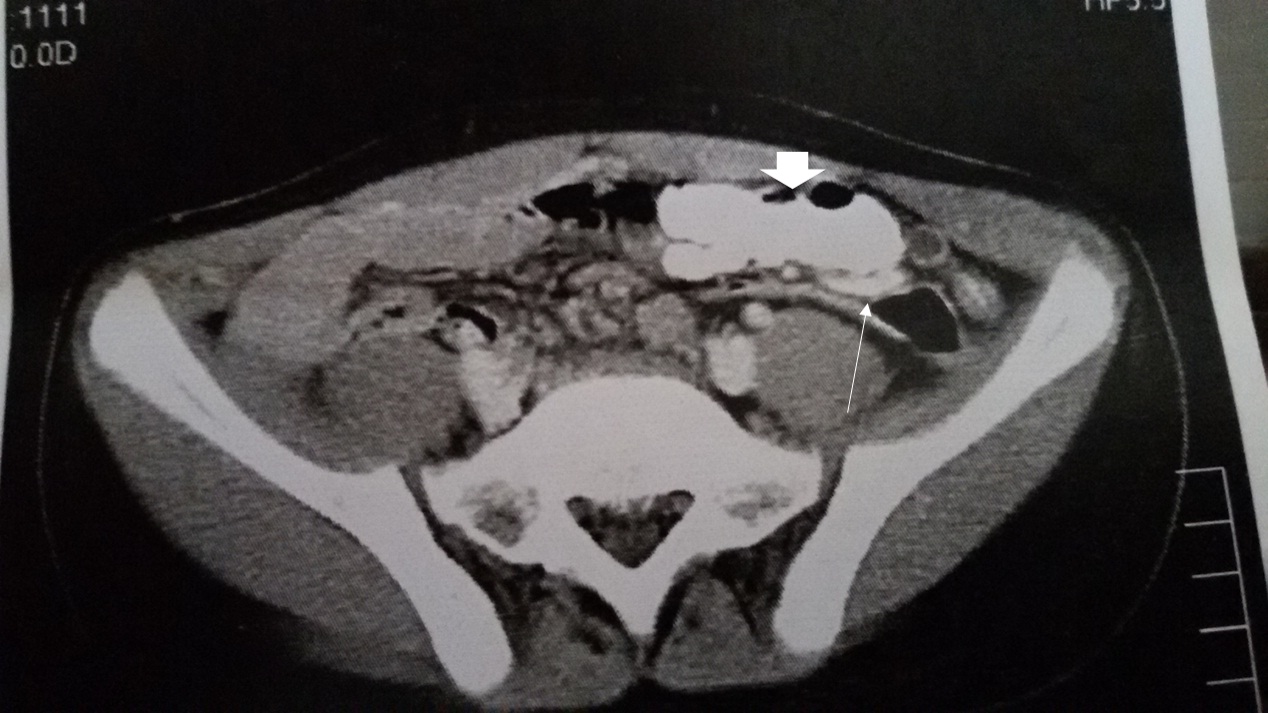
Ten months later, a 10-year-old male patient presented in the ED complaining for abdominal pain starting 3 days ago and located in the left abdomen. Associated symptoms included pyrexia (38.2oC), anorexia and nausea. Physical examination revealed tenderness and guarding in the left lower abdominal quadrant and laboratory investigation showed leukocytosis with polymorphonuclear neutrofilia and increased CRP. Our increased alertness and suspicion due to the previous case led to design a more structured approach to the possible diagnosis of LSA. Abdominal X-ray showed intestinal air fluid levels in the left abdomen and U/S investigation revealed a structure with a diameter around 8mm that resembled an inflamed appendix located in the left iliac fossa. The anatomic relationship of the superior mesenteric vessels could not be estimated so we proceeded to abdominal CT evaluation. The localization of an inflamed appendix in the left iliac fossa was confirmed but the relationship of the superior mesenteric levels was normal [Table/Fig-2].
CT imaging showing appendix and cecum in the left abdomen (arrow and arrowhead respectively).
After completion of the preoperative investigation the operative approach was planned and performed. A transverse right lower transverse skin incision near the midline that facilitated the investigation of the left iliac fossa was applied. A “wondering” cecum and the inflamed appendix were easily delivered into the wound and the appendectomy was performed. Inspection of the small intestine and its mesentery did not reveal any malformation and operation was completed. No complications were encountered during the postoperative period and the child was discharged safely from the hospital. Follow up is uneventful and free of any complications for both patients.
Discussion
Acute appendicitis is one of the most common surgical causes of abdominal pain in children. Typical presentation includes abdominal pain located in the periumbilical region and/or the right iliac fossa which is associated with nausea, fever and anorexia and abdominal tenderness during physical examination.
However, several atypical presentations have been reported in the literature which is estimated to be the 1/3 of all cases [1,2]. When the presentation is atypical the diagnosis of acute appendicitis can be quite challenging and a series of imaging investigations and also increased alertness and expertise are mandatory [3].
Left lower abdominal pain can be caused by a number of pathological conditions including left acute pyelonephritis, left renal or uretelal stone, irritable bowel syndrome, Meckel diverticulitis, Crohn’s disease, ulcerative colitis, left ovarian disease or fallopian inflammation or can be of muscle origin [4]. Acute appendicitis is scarcely considered in the differential diagnosis of left lower abdominal pain.
LSA causing pain and tenderness in the left abdomen is extremely rare and can occur in relation either to a true left sided appendix found in cases of situs inversus or midgut malrotation, or a “wandering” cecum with a long mesentery and an excessively long right sided appendix that crosses the midline [2,5].
Situs inversus is an extremely uncommon condition that may be complete when both thoracic and abdominal organs are transposed (situs inversus totalis-SIT) or partial when only one of those cavities is affected. After studying 71000 human appendix specimens, Collins D reported that the incidence of acute appendicitis associated with SIT is 0.016% [5]. In more recent study of 95 cases of LSA published in literature, 69.4% had SIT while 24.2% had midgut malrotation [6].
Midgut malrotation is a term used to describe a spectrum of conge-nital positional anomalies of the intestine caused by incomplete rotation of the primitive midgut around the axis of the superior mesenteric artery during fetal development. Around 50% of cases present in the first week of life while 60% are diagnosed in the first month of life due to its severe complications of midgut volvulus [7]. The rest may be diagnosed in childhood or adulthood either due to complications of the abnormality itself (midgut volvulus) or incidentally during the investigation of acute or chronic pathologies involving abdominal pain such as LSA [8,9].
Malrotation is classified into several types according to the embryological state of development. Errors in the first stage of rotation result in type Ia malrotation or non-rotation where the proximal small intestine lies on the right and the cecum on the left. Type Ia is estimated to be an incidental finding in 0.2% of adults. It is considered to be the most frequent and the least dangerous because the root of the mesentery is broad and long, and is most possible to be found during LSA evaluation [10].
In our first case, the emergency physician and the surgical team were caught by surprise mainly because the diagnosis was established by clinical criteria and were somehow misled due to the right and left abdominal tenderness. Such a condition can result in 18.4% - 31% of LSA cases because the sensory innervation of the appendix remains orthotopic despite the variation of its position [5]. The long and broad mesentery of the small intestine suggested type Ia malrotation which did not need any other intervention but most importantly did not set any worries for unwanted events in the future.
Interestingly, suggestive findings of intestinal malrotation were missed in the initial abdominal ultrasound investigation. Right sided symptomatology, minimal suspicion of the disease and possibly decreased experience of the radiologist on-call contributed to this result. Shekhar et al., faced the same problem as they performed two U/S studies prior to CT investigation in a 10-year-old patient [11].
Ultrasonographic diagnosis of malrotation is proposed as advantageous for children, because apart from its increased accuracy, it lacks the radiation effects of other imaging studies. Inversion of superior mesenteric vessels orientation is considered to be diagnostic of the disease. In a study of 23 patients, Zhou et al., reported sensitivity, specificity, and accuracy of ultrasonography for determining malrotation at 100%, 97.8%, and 98.6% respectively [12]. On the other hand, Orzech et al., in their study of 211 patients reported a positive predictive value of 42.1% and a negative predictive value of 96.3%. They concluded that U/S can be used for ruling out malrotation but further imaging is required in case it is suggestive of any anomalous intestinal fixation [13].
In the second case, the increased alertness and suspicion of both the surgical and radiological teams, led to a more structured preoperative and intraoperative approach that resulted in a correct diagnosis, strategically planned operation and uneventful postoperative period.
Conclusion
LSA is a rare condition that is not usually encountered in the differential diagnosis of left abdominal pain in children. The approach to these patients, consists a diagnostic challenge but is also open to misdiagnosis and medical pitfalls. Mandatory tools for an accurate diagnosis include thorough medical history, detailed physical examination, laboratory and imaging investigation including U/S and CT imaging. Above all, increased experience, alertness, suspicion and cautiousness by the medical team including the emergency physician, radiologist and surgeon in the diagnostic approach of these patients, is the cornerstone for a correct diagnosis and safe management and treatment.
Conflict of interest : None of the contributing authors have any conflict of interest, including specific financial interests or relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.
[1]. Tawk CM, Zgheib RR, Mehanna S, Unusual case of acute appendicitis with left upper quadrant abdominal painInt J Surg Case Rep 2012 3:399-401. [Google Scholar]
[2]. Hou SK, Chern CH, How CK, Kao DF, Chen JD, Wang LM, Diagnosis of appendicitis with lower quadrant painJ Chin Med Assoc 2005 68:599-603. [Google Scholar]
[3]. See TC, Watson CJE, Arends MJ, Ng CS, Atypical appendicitis: The impact of CT and its managementJ Med Imaging Radiat Oncol 2008 52:140-47. [Google Scholar]
[4]. Yang CY, Liu HY, Lin HL, Lin JN, Left sided acute appendicitis: A pitfall in the emergency departmentJ Emerg Med 2012 43:980-82. [Google Scholar]
[5]. Collins D, Seventy-one thousand human appendix specimens: a final report summarizing 40 years’ studyAm J Proctol 1963 14:365-81. [Google Scholar]
[6]. Akbulut S, Ulku A, Senol A, Tas M, Yagmur Y, Left-sided appendicitis: Review of 95 published cases and a case reportWorld J Gastroenterol 2010 16:5598-602. [Google Scholar]
[7]. Millar AJ, Rode H, Cywes S, Malrotation and volvulus in infancy and childhoodSemin Pediatr Surg 2003 12:229-36. [Google Scholar]
[8]. Yang B, Chen WH, Zhang XF, Luo ZR, Adult midgut malrotation: multi-detector computed tomography (MDCT) findings of 14 casesJpn J Radiol 2013 31:328-35. [Google Scholar]
[9]. Ely AB, Gorelik N, Cohen-Sivan Y, Zissin R, Carpineta L, Osadchy A, Appendicitis in adults with incidental midgut malrotation: CT findingsClin Radiol 2013 68:1212-19. [Google Scholar]
[10]. Bider K, Kaim A, Wiesner W, Bongartz G, Acute appendicitis in a young adult with midgut Malrotation: a case reportEur Radiol 2001 11:1171-74. [Google Scholar]
[11]. Shekhar A, Hendahewa R, Premaratne G, A diagnostic dilemma: Left-sided appendicitis in a 10 year old boy with previously undiagnosed intestinal malrotation. A case reportInt J Surg Case Rep 2015 14:10-2. [Google Scholar]
[12]. Zhou LY, Li SR, Wang W, Shan QY, Pan FS, Liu JC, Usefulness of sonography in evaluating children suspected of malrotation: comparison with an upper gastrointestinal contrast studyJ Ultrasound Med 2015 34:1825-32. [Google Scholar]
[13]. Orzech N, Navarro OM, Langer JC, Is ultrasonography a good screening test for intestinal malrotation?J Pediatr Surg 2006 41:1005-09. [Google Scholar]