The lacrimal glands (LGs) are paired, almond-shaped structures, located at the upper-outer portions of orbits, adjacent to the lateral and superior rectus muscles [1]. The LG is a target tissue especially in autoimmune and granulomatous diseases. Changes in LG size may be helpful in diagnosis of these atypical and difficultly identified pathologies [2,3]. Therefore evaluating the LG sizes in computed tomography (CT) scan which is an accessible and widespread method in head and neck imaging, may enable early diagnosis and treatment of mentioned pathologies [4]. Previous studies stated that LG dimensions and volumes may change with age, gender and race [5]. Hence knowledge the normal dimensions and volumes of healthy LGs according to ethnicities may be helpful early diagnosis of gland pathologies in routine radiologic procedures.
Previous studies only evaluated either gland dimensions or volume and to the best of our knowledge, there is no report in which gland dimensions and volume were presented together. In addition, normal LG dimensions and volume in non-diseased orbits of the Turkish population has not been established up to date.
In this study, we aimed to evaluate the dimensions and volume of non-diseased LG in a Turkish population, the relationship of measurements with laterality, age and gender and compared our results with previous studies.
Materials and Methods
Institutional ethics committee approval was obtained prior to this retrospective study. Two hundred seventeen consecutive paranasal CT scans, performed in Balıkesir University Education and Training Hospital between August 2013 and January 2014 were evaluated. CT scans of subjects whom are equal or older than 18-year-old without any orbital pathology were included in the study. Both sides of all subjects were evaluated separately. Subjects with a history of trauma, infiltrating or inflammatory lesions, even if the lesion was unilateral, were excluded. CT exams were performed with a 64-slice scanner (Toshiba Aquilion 64, Otawara, Japan) in routine 0.5mm slice-thickness paranasal CT protocol. Coronal reformatted images were constituted with DICOM imaging viewer (Aquarius 3D Workstation, Tera Recon, San Mateo, CA, USA). Both axial and coronal images were evaluated with a soft-tissue algorithm [6]. One image for measuring gland dimensions was chosen from axial and coronal images, in which LG was the largest.
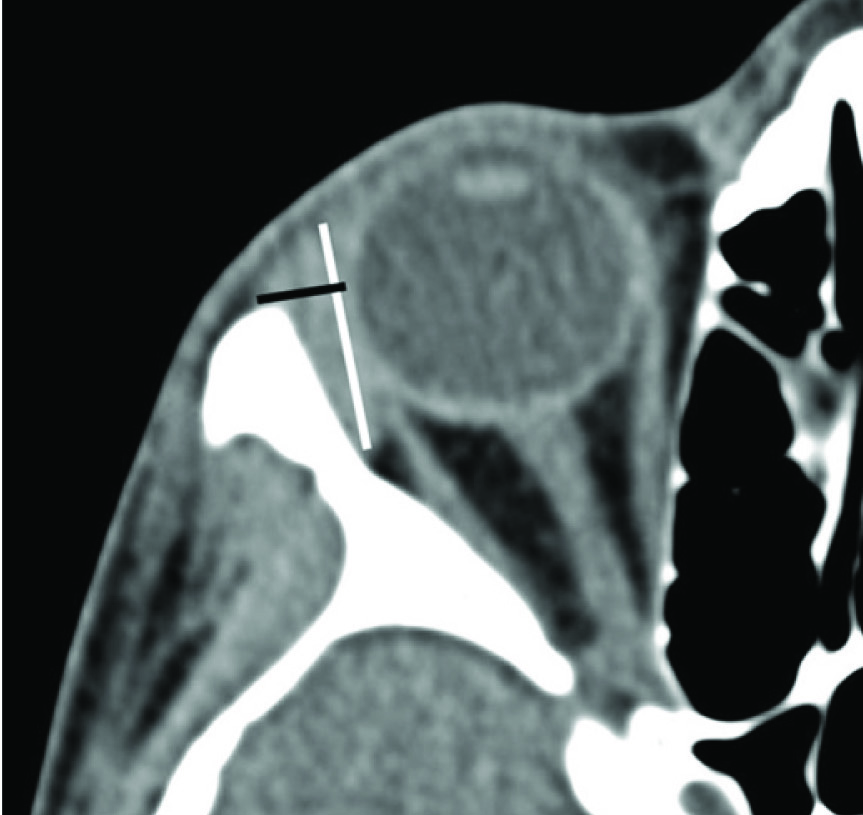
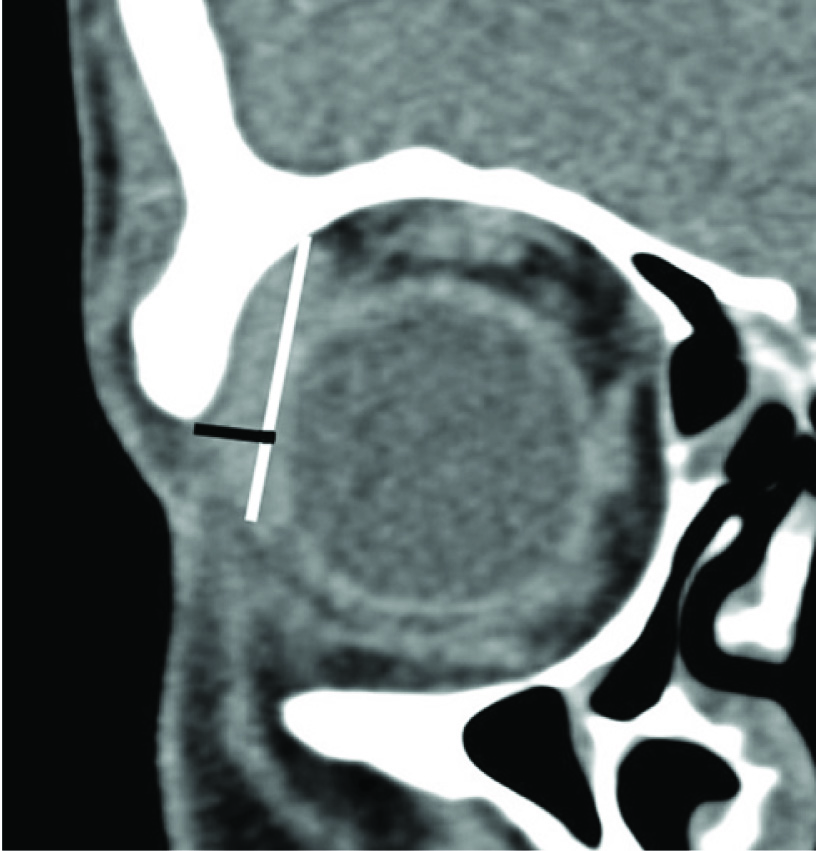
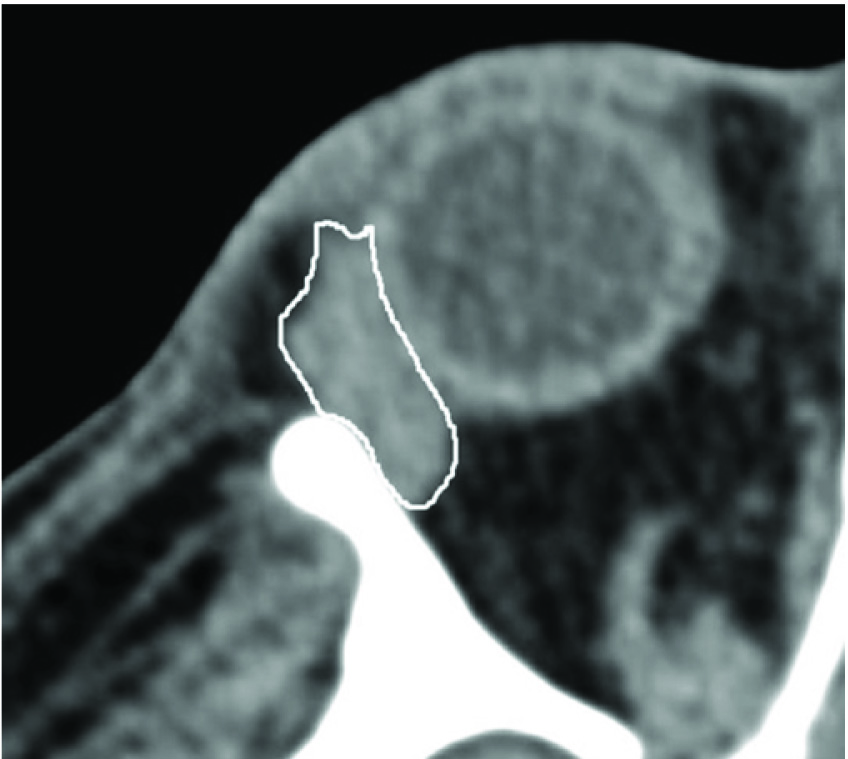
LG dimensions were calculated with the method described by Tamboli et al., in magnified images [Table/Fig-1,2 and 3] [6]. Two radiologists independently evaluated 20 random CT scans. After interobserver agreement was determined, one radiologist performed the remaining measurements. In the selected axial image, the length was calculated from the most-anterior tip to the most-posterior tip of the gland. The width was calculated from the medial to lateral edge at the widest location perpendicular to the length in the same image [Table/Fig-1]. In the selected coronal image, the length was calculated from the most-superior tip to the most-inferior tip. The width was calculated perpendicular to the length at the widest location from the medial edge to lateral edge [Table/Fig-2]. The volume of the LG was measured from axial images. The gland was outlined with a free-hand technique by the pencil tool in all consecutive images including the LG [Table/Fig-3]. The volume of selected area was calculated by the software (Aquariousi Ntuition edition, version 4.6; TeraRecon, San Mateo, CA, USA).
White line represents the axial length and black line represents the axial width in the axial CT image.
White line represents the coronal length and black line represents the coronal width in the coronal CT image
The lacrimal gland was outlined with pencil tool in the axial image (white line).
Shapiro-Wilk test was used for evaluation of the normality distributions of each gland dimensions volume. Each sides of orbit were analyzed separately. Independent sample t-test was used for evaluating differences in laterality and gender. The Pearson correlation test was used for determining the relationship between LG volume and age. Interobserver intraclass correlation coefficient (ICC) was calculated with the ICC interpretations described by Landis and Koch [7].
Results
Four hundred orbits of 200 subjects included to the study. Male to female ratio was 113/87. The mean age was 40.56±16.33 years (18-86). There was no statistical difference at the age of males (40.94±17.41) and females (40.07±14.90) (p=0.71).
Lacrimal Gland Measurement
The dimensions and volume were normally distributed in the right and left orbits [Table/Fig-4]. The mean LG axial lengths were 16.2±2.0 mm in the right orbit and 16.0±2.0 mmin the left orbit. The axial width was 4.1±0.7 mm in the right orbit and 4.0±0.7 mm in the left orbit. The right and left mean values for coronal length and width were equal 18.3±2.3 mm and 4.1±0.7 mm respectively. The axial width of LG in right side was significantly higher than the left side (p=0.03). There was no statistically significant difference in the other dimensions between both sides. When intergender difference was evaluated, only the axial width was statistically significantly larger in males (p=0.05); whereas there was no statistically significant difference in axial length, coronal width and coronal length.
Descriptive statistics for lacrimal gland dimensions of the right and left orbits in millimeters.
| Percentiles |
|---|
| Measurement | Mean | SD | 5% | 10% | 25% | 50% | 75% | 90% | 95% |
|---|
| Right orbit |
| Axial Length | 16.2 | 2.0 | 12.8 | 13.6 | 15.0 | 16.3 | 17.5 | 18.5 | 19.0 |
| Axial Width | 4.1 | 0.7 | 3.0 | 3.2 | 3.6 | 4.1 | 4.6 | 5.1 | 5.3 |
| Coronal Length | 18.3 | 2.3 | 14.4 | 15.8 | 16.9 | 18.5 | 19.7 | 21.2 | 21.7 |
| Coronal Width | 4.1 | 0.7 | 3.0 | 3.2 | 3.7 | 4.1 | 4.5 | 5.0 | 5.5 |
| Left eye |
| Axial Length | 16.0 | 2.0 | 12.3 | 13.2 | 14.9 | 16.1 | 17.2 | 18.6 | 19.2 |
| Axial Width | 4.0 | 0.7 | 2.9 | 3.1 | 3.5 | 4.0 | 4.4 | 4.9 | 5.1 |
| Coronal Length | 18.3 | 2.3 | 14.4 | 15.4 | 17.0 | 18.3 | 19.8 | 20.9 | 22.0 |
| Coronal Width | 4.1 | 0.7 | 3.0 | 3.3 | 3.6 | 4.1 | 4.5 | 4.9 | 5.4 |
The mean LG volume was 0.617±0.210cm3in right orbits and 0.597±0.197 cm3 in the left orbits [Table/Fig-5]. There was a statistically significant difference between both sides (p<0.01). The volumes were similar in both genders without any statistical significance (p>0.6 for both sides).
Descriptive statistics for lacrimal gland volumes of the right and left orbits in cubic centimeters.
| Percentiles |
|---|
| Measurement | Mean | SD | 5% | 10% | 25% | 50% | 75% | 90% | 95% |
|---|
| Right orbit | 0.617 | 0.20 | 0.30 | 0.35 | 0.47 | 0.60 | 0.76 | 0.90 | 0.98 |
| Left orbit | 0.597 | 0.21 | 0.30 | 0.34 | 0.44 | 0.58 | 0.71 | 0.88 | 0.95 |
There was negative correlation between age and LG dimensions and volume which was statistically significant (p=0.001 and r>-0.351) [Table/Fig-6].
Distribution of right lacrimal gland volumes according to age
| Age | No | Vol (cm3) | SD |
|---|
| 18-29 | 58 | 0.757 | 0.196 |
| 30-39 | 43 | 0.674 | 0.194 |
| 40-49 | 42 | 0.561 | 0.147 |
| 50-59 | 30 | 0.520 | 0.147 |
| ≥ 60 | 27 | 0.401 | 0.138 |
| Total | 200 | 0.615 | 0.209 |
Interobserver Agreement
The interobserver agreement was assessed after 20 LG dimension and volume measurements were performed by two radiologists. The measurements of the two observers showed an excellent agreement with an ICC >0.760 for each calculation including axial, coronal length and width and volumes.
Discussion
Both magnetic resonance imaging (MRI) and CT can be used effectively for detection of LG pathologies [3,8–10]. It is important to reveal the anatomic characteristics of LGs because much pathology such as sarcoidosis, Sjögren disease, thyroid ophthalmopathy, benign and malign tumors manifest with changes in LG sizes [3,9,10]. Apart from evaluation of the gland particularly, knowing the gland size and imaging characteristics is also important since LG might fall into the head and neck radiologic examination.
Previous studies in the literature reported different LG sizes between different ethnicities. Tamboli et al., published the first study establishing non-diseased LG dimensions with CT [6]. They calculated LG dimensions in Caucasian patients with normal LGs. Significant difference was observed only in mean coronal length between the right and left orbits, other dimensions were similar between two sides. The second study describing non-diseased LG dimensions with CT was published by Lee et al., in a Korean population with normal LGs [11]. They suggested that the axial and coronal width were slightly larger in the left orbits.
In our study, the axial length, coronal length and coronal width were similar in both right and left sides, and no statistically significant difference was observed. Statistically significant difference was found only in axial width between right and left orbits (p=0.03). The axial length in both orbits in our study was larger than the previous studies [Table/Fig-7]. The other dimensions were variable. The coronal length was longer and axial and coronal widths were shorter than that observed by Tamboli et al., in a Caucasian population [6]. According to the study of a Korean population, the axial width was equal with the right orbits but smaller in the left in our study [11]. Coronal width was larger and coronal length was shorter in our study in both sides when compared to the study reported by Lee et al [11]. The results of the current study might implicate the importance of the national difference in normal values of LG dimensions.
The mean lacrimal gland dimensions in different ethnicities in millimeters
| Caucasian [6]Tamboli et al. | Korean [11]Lee et al. | Currentstudy |
|---|
| Right eye |
| Axial Length | 14.7 | 14.9 | 16.2 |
| Axial Width | 5.1 | 4.1 | 4.1 |
| Coronal Length | 17.7 | 20.9 | 18.3 |
| Coronal Width | 5.2 | 3.6 | 4.1 |
| Left eye |
| Axial Length | 14.5 | 14.7 | 16.0 |
| Axial Width | 4.8 | 4.3 | 4.0 |
| Coronal Length | 16.9 | 20.7 | 18.3 |
| Coronal Width | 5.2 | 3.8 | 4.1 |
In a previous study, Avetisov et al., calculated LG volume with ultrasound in healthy subjects [12]. LG volume was reported in a range of 0.66 to 1.0cm3. In the first study to report the LG volume in CT imaging, Bingham et al., calculated the normal LG volumes in a Caucasian population [13]. LG volume measurement with MRI was also recently published. In this study, beyond being the first study to evaluate LG with MRI, they had the chance to compare LG volumes in different ethnicities and found that volume changes significantly according to the ethnical origin [5]. The results of our study support the finding of Bukhari et al., since our measurements in Turkish population was approximately 11.5-17.0% smaller compared to the different ethnicities in these two studies [5] [Table/Fig-8].
The mean lacrimal gland volumes in different ethnicities in cubic centimeters
| Ethnicity | | | Vol | SD |
|---|
| Middle Eastern[5] | Bukhari et al., | (n=367) | 0.743 | 0.332 |
| Indian [5] | Bukhari et al., | (n=35) | 0.776 | 0.371 |
| Asian [5] | Bukhari et al., | (n=13) | 0.883 | 0.394 |
| African [5] | Bukhari et al., | (n=84) | 0.870 | 0.342 |
| Caucasian [13] | Bingham et al., | (n=134) | 0.696 | 0.261 |
| Current study | | (n=200) | 0.617 | 0.217 |
Bingham et al., did not report significant difference between males and females similar to the present study results [13]. But Bukhari et al., reported higher gland volume in women [5]. In our study there was no statistically significant difference between gender.
The laterality had no effect in volumetric measurements of LGs in Bingham et al., [13] study. However, similar to our study, Bukhari et al., had found right gland volumes to be larger than the left [5].
Obata showed that lacrimal gland atrophy and fibrosis correlated with increasing age [14]. Studies both performed with MRI and CT reported a decrease in the lacrimal gland sizes with increasing age [5,6,13]. Also, in our study, there was a negative correlation between age and gland dimensions and volume. Decrease of LG volume was correlated with all axial and coronal dimensions.
Limitations
Our study has some limitations. First of all LG and surrounding tissue densities may cause a challenge, in measuring gland dimensions and volume in CT imaging. However, Bukhari et al., calculated LG volumes in both CT and MRI of 36 patients and reported no significant difference in two modalities [5]. The second limitation was the retrospective nature of our study that did not allow us to choose MRI or CT imaging.
Conclusion
In conclusion this study may serve a guide in determining the normal values of LG dimensions and volume in Turkish population. In this study LG dimensions and volume are showed some differences from previous studies performed in various ethnicities. Further studies may be helpful in determining normal values and ranges of healthy LG dimensions and volume in different ethnicities.