The healing of wound is a sequence of cellular and biochemical activities, which aim towards restoring tissue integrity and functional capacity after injury [1]. Healing usually takes place uneventfully without any complications in most of the cases, but various intrinsic and extrinsic factors can affect the process.
Oral and maxillofacial surgical procedures often produce open wounds. A dressing material should cover these wounds to prevent microbial infection, foreign material contamination, wound contracture, and improve healing. The existence of a variety of wound types with varied healing modes and phases led to the evolution of different types of wound dressings.
Wound dressings before 1960s, were considered passive products that had a minimum role in the healing process [1]. Currently, oral mucosa or skin grafts are used as dressings; however, both these dressings have disadvantages in intraoral use like limited availability and presence of adnexal structures, abnormal tissue texture interfering with function respectively [1].
Therefore, there is search for an ideal dressing material to cover these defects. One such product is bovine derived collagen, a biologic material, which can be moulded into desired form and used in many clinical conditions as temporary dressing materials with favourable results [2–6]. Tolerance of xenogenous collagen by host tissue and its successful use as a temporary cover for raw areas in oral cavity was assessed.
Materials and Methods
This study of clinical evaluation of use of collagen membrane in intraoral defects was done in the Department of Oral and Maxillofacial Surgery; GITAM Dental College and Hospital, Visakhapatnam, Andhra Pradesh. Ethical committee clearance was obtained for doing the study with the use of bovine derived collagen membrane.
A total of 30 patients between 20-60 years, with ASA - grade 1 who requires intraoral dressing for the raw surfaces resulting from excision of premalignant lesions like leukoplakia, irritational growths, mucocele and pre-prosthetic surgical procedures were included in the study. Patients below 20 years and above 60 years of age, evidence of systemic or oral infection, uncontrolled systemic disorders i.e., ASA grade ii-vi are excluded from the study.
The collagen used in this study is a purified bovine reconstituted collagen. Reconstitution was done to remove atelocollagen component, which lowers its antigenicity. This reconstituted collagen is cross-linked with tanning agents like gluteraldehyde or chromium sulphate; to improve its tensile strength, to decrease its rate of resorption. Collagen membrane which comes in varying dimension of 5x5 cm, 10x10 cm and 25x25 cm, with thickness of 0.6mm, produced by EUCARE pharmaceuticals.
Surgical Procedure
Relevant history was taken from the patients and careful clinical examination was done. Appropriate patient’s consent was taken. Surgical excision of the intraoral lesion was done under local anaesthesia by following aseptic precautions. After surgical excision, haemostasis was attained. Collagen membrane is thoroughly washed in sterile saline solution (in order to remove the preserving medium). Membrane was trimmed according to wound size and quilting/nicks given to the membrane to facilitate drainage. It was stabilized and sutured to the edges of the wound. A few sutures were also given in the centre of the defect for appropriate membrane adaptation and drainage of the collected fluid below the membrane through the holes created in taking the bite for placing sutures.
Parameters Assessed
Haemostasis achieved by the membrane was assessed and scored on the day of surgery:
2 - GOOD - no bleeding or when bleeding stops with in 5 min
1 FAIR -slight bleeding or no intervention required or haemostasis achieved after prolonged period i.e., more than 5 min
0 - POOR -bleeding that required intervention for achieving haemostasis
Pain being subjective, assessed on the 4th postoperative day, based on patients own words:
2 - GOOD (none to mild)
1 - FAIR (moderate)
0 - POOR (severe)
Presence of granulation tissue noted at the end of two weeks as:
2 - GOOD (entire wound)
1 - FAIR (nearly the entire wound)
0 - POOR (inadequate)
Epithelialization noted at the end of the month as:
2 - GOOD (entire wound)
1 - FAIR (nearly the entire wound)
0 - POOR (inadequate)
Contracture of the wound at the end of the month was recorded:
2 – GOOD (<25%)
1 - FAIR (25 to 50%)
0 - POOR (severe i.e. >50%)
Additional Paramaters Assessed:
6. Conformability of the collagen sheet i.e. dressing ability.
7. Infection present or absent during the period of healing.
8. Adherence based on the ability of collagen to adhere to the wound after irrigating the area with sterile saline was recorded after suture removal.
The criteria for judgement of collagen dressing membrane with respect to the results obtained is based on the scoring pattern which was used by Bessho k et al., in their study of a new bi-layer artificial dermis for vestibular extension [5]. Using this scoring pattern effectiveness of collagen membrane was evaluated.
Effectiveness of the membrane was obtained by adding the scores of haemostasis, pain relief, granulation, epithelialization and contracture of the wound as:
If total score is 8-10 - very effective
If total score is 5-7 - effective
If total score is 0-4 - in effective (bessho k et al., [5])
Results
Collagen membrane was used as a dressing material for 30 intra oral raw wounds among which excision of epulis growths-4, mucocele-2, pyogenic granuloma-2, irritational firoma-6, leukoplakia patches-9, frenectomies-7.
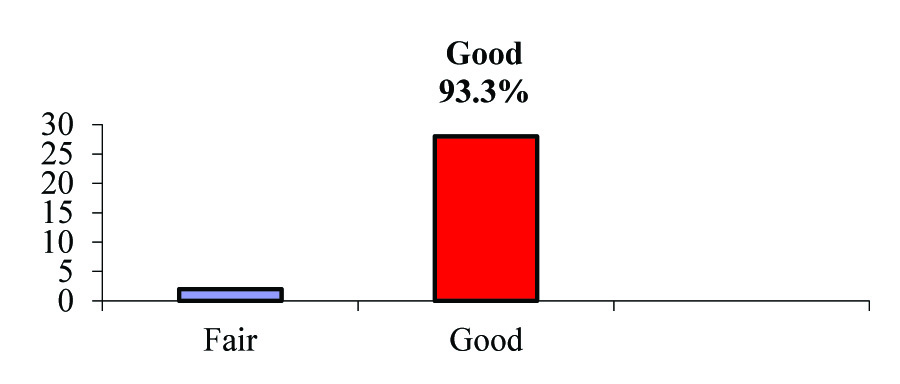
[Table/Fig-1] shows GOOD haemostasis in 28 cases (93.3%), FAIR in two cases (6.6%).
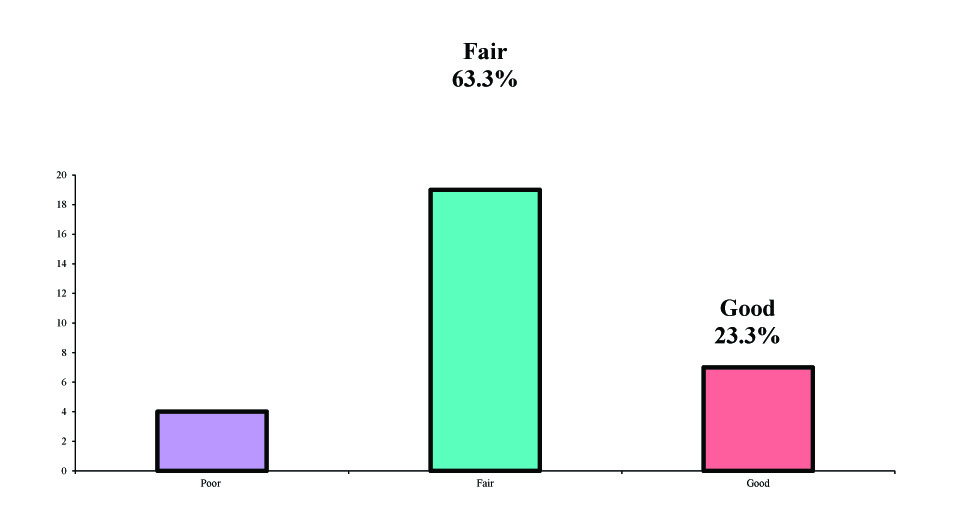
[Table/Fig-2] shows pain relief is GOOD in seven cases (23.3%), FAIR in 19 cases (63.3%), POOR in 4 cases (13.3%).
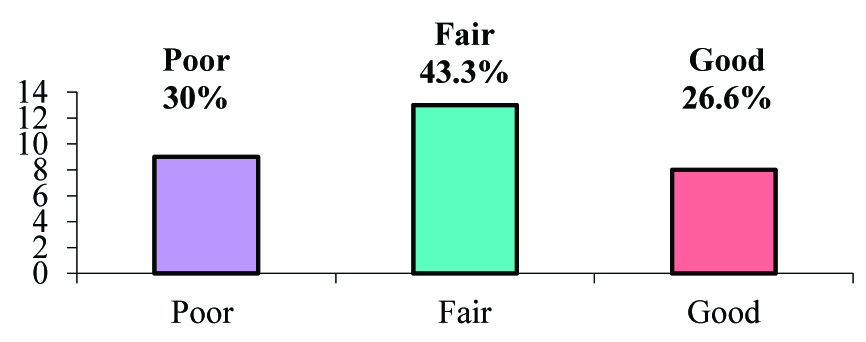
[Table/Fig-3] shows granulation is GOOD in eight cases (26.6%), FAIR in 13 cases (43.3%), POOR in 9 cases (30%).
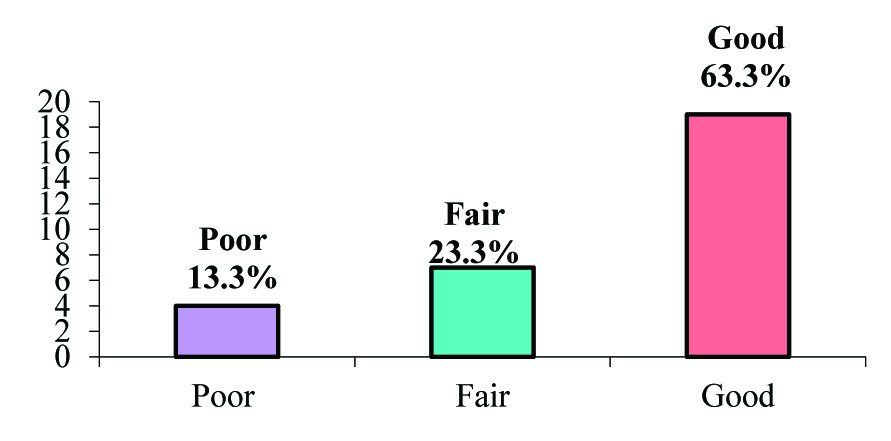
[Table/Fig-4] shows epithelialization is GOOD in 19 cases (63.3%), FAIR in 7 cases (23.3%), POOR in four cases (13.3%).
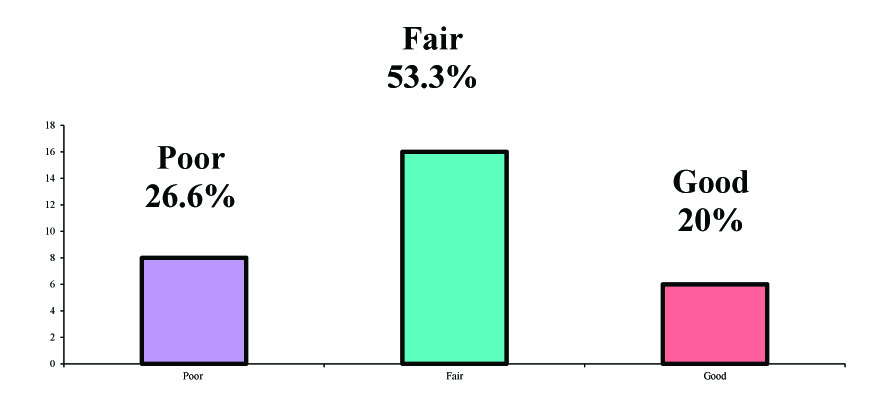
[Table/Fig-5] shows contracture is GOOD in six cases (20%), FAIR in 16 cases (53.3%), POOR in eight cases (26.6%).
[Table/Fig-6,7] shows total score of all the five parameters which is rated as effectiveness score.
Total score is 8-10 in 6 cases (20 %) - very effective,
Total score is 5-7 in 20 cases (66.6 %) - effective,
Total score is 0-4 in 4 cases (13.3%) - ineffective.
Distribution of samples by Haemostasis.
Distribution of samples by pain.
Distribution of samples by granulation tissue
Distribution of samples by Epitheliazation
Distribution of samples by Contracture.
Distribution of samples by effectiveness scores
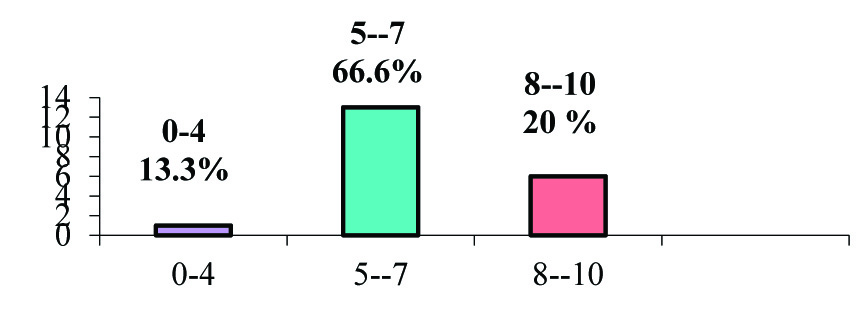
Distribution of Samples by Effectiveness Scores
| Effectiveness | No of Samples | % of Samples |
|---|
| 8-10(very effective) | 6 | 20 |
| 5-7(effective) | 20 | 66.6 |
| 0-4(in effective) | 4 | 13.3 |
| Total | 30 | 100.0 |
Discussion
The raw wounds of the oral cavity, as any other wound heals by granulation and epithelialization as the oral environment is always moist with contamination from saliva and food, compounded by constant movements of cheek and tongue [2]. The risk of infection in the oral cavity is also quite high, which may result in scarring and contraction. The oral cavity is highly sensitive to any residual scarring, which may undergo ulceration and could be a constant source of irritation to patients wearing dentures. It has been well documented that the incidence of infection & degree of contraction are considerably reduced when wounds dressed rather than left exposed. Experiments have shown that dressings create physiological interface between the wound surface, environment and permits repair [2].
An ideal soft tissue dressing should promote haemostasis, prevent infection, reduce pain, promote granulation tissue formation, rapid re-epithelialization, reduces contracture and avoids the donor site morbidity [7]. With this view in mind, raw wounds in orofacial region were covered with skin graft, mucosal graft [8].
Collagen can be used as an alternative to the above mentioned graft materials to cover the intraoral surgical defects. As there is a large body of evidence that collagen is a common denominator in all stages of wound healing it serves as the key extracellular component for repair and remodelling [9]. Unique features of collagen membranes include guiding function, chemotactic property, haemostatic property and can resist masticatory forces for sufficient time and allows granulation tissue to form. Bovine xenogenous collagen membrane is easily obtainable which does not require second operation and its associated morbidity [7]. Abundant availability of the material does not impose dimensional limitations to the surgical site and immediate availability. Collagen dressings are found to have significantly fastened the healing process as collagen serves as the most important element in all stages of wound healing according to Paul US et al., [9].
A clinical study of 30 patients where the raw areas resulting from excision of epulis growths (8), mucocele (2), irritational fibromas (10), leukoplakia (4), pyogenic granuloma (2), frenectomies (11) were covered with collagen membrane. The parameters studied are haemostatic effect, pain relief, granulation tissue formation, re-epithelization and the contracture of the wound.
Collagen membrane has a inherent property of haemostatic effect as it is a specific activator of platelets and helps in their adhesion to collagen fibre, aggregation. Study showed good haemostatic effect in 28 cases out of 30 (93.3%) and fair in two cases (6.6%) which is in accordance with the study conducted by Zucker et al., mannai et al., which stated that collagen produces rapid haemostasis and strengthens the clot. In the ultra structural study, interactions of platelets with microfibrillar collagen is studied, the platelet adherent to collagen appeared to undergo an actual sequential morphologic change. Collagen acts as chemotactic factor for platelets, influencing their adhesion, aggregation, and release reaction according to the co-stasis multi–centric collaborative writing committee [10].
Collagen when used to cover the raw area provides the coverage for sensitive nerve endings thereby diminishing degree of pain. As collagen is a natural substrate of extracellular matrix, is chemotactic to various cell types such as endothelial cells, fibroblasts there by leading to reduced inflammatory process which contributes to reduced pain and burning sensation. Pain relief was not achieved in four cases, wherein the collagen membrane was lost during early phase of healing. In rest of the cases the pain relief was rated as good in seven cases (23.3%) and fair in 19 cases (63.3%). This result is in accordance with the study conducted by Raghavendra Reddy et al., Paul US et al., Shobha Natraj et al., [3,9,11].
Collagen dressings encourage wound healing through early deposition and organization of granulation tissue. It facilitates migration of fibroblasts in to the wound bed, encourages the metabolic activity of granulation tissue. Results showed as good in 8 cases (26.6%), fair in 13 cases (43.3%), poor in 9 cases (30%) which are in accordance with the studies of Onkar Singh et al., K Bessho and Muramaki et al., Shobha Natraj et al., [3–5].
Collagen membrane is known to stabilize the coagulum and enhances the early epithelial proliferation from the surrounding tissues. Good epithelialization was achieved in 19 cases (63.3%), fair in seven cases (23.3%), poor in four cases (13.3%) which are in accordance with the studies of Thoma et al., K Bessho and Shobha Nataraj et al., [3,4,12]. Faster re-epithelialization achieved with better colour match to the adjacent normal tissues.
The most important method for controlling scarring is by controlling infection and fastening re-epithelialization, collagen fulfils these goals, there by prevents scar contracture (Sanjay Rastogi [2]), contracture is found to be good in six cases (20%), fair in 16 cases (53.3%), poor in eight cases (26.6%). The results achieved are similar to that of the results of Masaki Fujioka et al., S Wakami et al., Herford et al., Shobha Nataraj et al., [3,7,13,14].
In our study collagen dressings showed accelerated healing process in accordance with the studies of M Shanmugam et al., Thoma et al., Omkar Singh, this may be explained through the formation of a gelatinized coagulum containing abundant amount of fibrinogen and fibronectin which contains high concentrations of chemo attractants, growth factors help in deposition and organization of freshly formed fibres [4,12,15]. Granulation tissue facilitates migration of fibroblasts in to the wound bed. Tissue biopsy with detailed histopathological study at frequent intervals is necessary to establish the fact that initial adherence and faster uneventful healing is possible by the use of collagen membrane for intraoral wounds, which is lacking in our study and is recommended in future studies.
Collagen membrane is supple & adapted to the wound no matter what the contour is. It was observed that membrane had good adherence to mucosa and wound bed. The adherence of collagen membrane is initially due to fibrin collagen interaction & later due to fibro vascular in growth into the collagen membrane [1,15]. This study had no histological study conducted to prove this fact.
Collagen membrane was robust enough to resist masticatory forces for certain time, to allow granulation tissue to form, later it underwent collagenolysis. The preparation of stents for larger defect is necessary to hold the collagen membrane close to the tissues until the initial phase of healing occurs, but for practical purpose it becomes difficult to fabricate, adapt and secure the stent in the intraoral region, for this reason it may be suggested that reinforced collagen membranes can be used in the areas where the wound bed is mobile i.e., buccal and labial mucosa and the normal collagen membrane can be used where the wound bed is stable like alveolus and palate.
Collagen appears to be biocompatible with no significant immune rejection with biodegradable characteristics in accordance to Marvin p levin, y Raghavendra reddy et al., David J Mishkin et al., AK Schlegel et al., K Bessho and Shobha Nataraj et al., Sanjay Rastogi et al., Omura et al., [2,3,6,11,16–18]. None of the case showed adverse or allergic reaction to the collagen proving its safety as a biological dressing. This result is in accordance with Y Raghavendra Reddy et al., [11].
Limitation
Limitations in this study are that in four cases of our study, (one on palate, second one in retro molar area) there was loss of collagen membrane because of continuous movements of tongue and membrane in the line of occlusion. Stabilization of the membrane to the surgical defect in this present study was done by suturing the membrane to the edges of the defect, which was a time taking and delicate procedure. It should be done without damaging the membrane. It can be recommended that the use of biological glue such as cyanoacrylates for this purpose can be tried in future study.
Conclusion
Reconstituted bovine derived, collagen membrane used in our study was found to be a useful dressing material to cover the raw areas of the oral cavity secondary to surgical excision of small lesions and where the base of the defect is immobile. Simple chair side application, ease of availability, no donor site morbidity, biocompatibility and better cosmesis makes the collagen membrane an ideal intraoral wound dressing material for faster uneventful healing.