Introduction
Management of pain poses to be a major challenge for clinicians during root canal treatment. Therefore, maximum efficacy of local anaesthesia is a pre-requisite for painless execution of the clinical procedures.
Although the Inferior Alveolar Nerve Block (IANB) is the most routinely administered technique for achieving profound anaesthesia during root canal treatment of mandibular teeth, it does not always ensure successful anaesthesia with clinical studies demonstrating a success rate varying from 15% - upto 57% only [1].
Clinicians regularly prescribe analgesics as premedication for management of mild to moderate pain [2] due to pulpal inflammation prior to injection of local anaesthesia. NSAIDs reversibly inhibit cyclooxygenase (COX) enzyme mediated production of prostaglandins (PGs) and thromboxane A2. Given the ability of NSAIDs in reducing nociceptor activation by decreasing the levels of inflammatory mediators [3], it has been hypothesized that pre-medication with NSAIDs will positively influence the success rate of local anaesthesia in patients with irreversible pulpitis [4–6].
Diclofenac and ketorolac are two commonly used nonsteroidal anti-inflammatory drugs (NSAIDs) used to manage moderate to severe pain. These drugs have been found to be beneficial in cases of exaggerated inflammation due to their ability to non-selectively inhibit the COX enzyme pathway. Since a considerable number of teeth indicated for root canal treatment are diagnosed with acute irreversible pulpitis, these NSAIDs may have significantly positive impact on the success of IANB. Moreover, they have a short half-life and an immediate release formulation which would make them ideal to be used in a single dosage prior to the management of severe odontalgia, in addition to ameliorating post treatment pain [7,8].
The purpose of this prospective, randomized, double-blind clinical study therefore, was to compare the efficacy of oral pre-medication with Ketorolac (KETO), Diclofenac Potassium (DP) and a Placebo (PLAC) medication on the anaesthetic efficacy of IANB with 2% lidocaine with 1:200 000 epinephrine in patients with irreversible pulpitis.
Materials and Methods
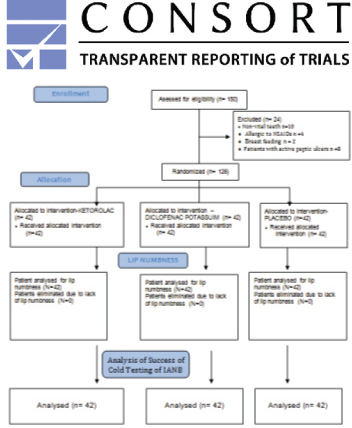
One hundred and fifty adult volunteers with acute irreversible pulpitis, within the age range of 18–65 years, who reported to the Department of Endodontics, were assessed for eligibility to participate in the prospective randomized double-blind clinical trial (4722/2015). The inclusion criteria were as follows: age 18 years or older, good health, moderate or severe pain in a first or second mandibular molar with no intake of medicaments for 12 hour prior to treatment. Sample size calculation revealed that a minimum of 21 patients per group would be required to detect a difference of 10 in the mean VAS score of the two groups, at an alpha of 0.05 with power a of 80%. A p-values < 0.05 was considered to indicate statistical significance. All of the 150 volunteers were evaluated for participation in the study, following the guidelines suggested by the CONSORT group [9] for planning and reporting clinical trials [Table/Fig-1]. Subjects with non-vital teeth, those allergic to NSAIDs and lignocaine, pregnant and lactating women, those who were not capable of giving proper consent or were experiencing only mild pain (as verified with VAS), and patients with active peptic ulcers were eliminated from the study. Hence, 42 patients were allocated to each group to justify the sample size. Ethical clearance was obtained from the institutional ethical committee which was in accordance with the Declaration of Helsinki. The procedure was explained to the patients and written informed consents were obtained. Preoperative radiographs of the involved teeth were recorded.
CONSORT 2010 Flow Diagram.
The selected subjects had a diagnosis of SIP (Symptomatic irreversible Pulpitis) and presented with prolonged moderate or severe pain (>10 s) after cold testing (Endo-Ice F, Coltene/Whaledent Inc., Cuyahoga Falls, OH, USA).
Before initiating the treatment, the patients were asked to rate their pain on a Heft Parker visual analogue scale (VAS) [10] with markings on 170-mm line which indicates the levels of pain [10]. The marks in millimeter were then eliminated from the scale, and the scale was categorized into four groups: no pain (corresponding to 0 mm); faint, weak or mild pain (corresponding to 1–54 mm); moderate to severe pain (corresponding to 55–114 mm); and strong, intense, maximum possible pain (corresponding to more than 114 mm) [11].
A trained dental hygienist divided the 42 tablets of each NSAID into three bottles: Ketorolac (KETO), Diclofenac Potassium (DP) and Placebo (PLAC). The bottles were masked with an opaque label and were randomly assigned as Group A, B & C respectively. The patients were then randomly divided into three groups of 42 patients each and one tablet was given to each one of them 1 hour before the procedure.
Randomization of patients was achieved by simple random sampling with a linear congruential generator by a trained dental hygienist who was blinded to the treatment procedures. Only the alphabetical values were recorded on the data sheets to blind the experiment. After 1 hour of oral administration of the tablets, all patients received standard IANB injections using 1.8 mL of 2% lidocaine containing 1: 200 000 epinephrine (Lidayn, India). The solution was deposited using self aspirating syringes (Septodont, Saint-Maur-des-Fosses Cedex, France) with 27-gauge needles (Septoject, Septodont, France) at a rate of 1 mL/ min.
Fifteen minutes after administration of the initial IANB, each patient was questioned regarding the onset of lip numbness on his or her lip. If profound lip numbness was not recorded within 15 min, the block would be considered unsuccessful and the patient would be excluded from the study. However, none of the subjects in this study were excluded due to lack of lip numbness. The tooth in question was then tested again with cold spray and the possible outcomes were recorded. In case of positive response with cold spray, the test would be recorded as failure and supplemental anaesthesia would be required. In the present study however, none of the anaesthetized teeth showed positive response with cold test. The tooth was then isolated with a rubber dam and a standard endodontic access cavity was prepared using a tapered safe-ended diamond bur under water spray coolant. In case of pain during the treatment, the outcome was recorded as failure and supplemental anaesthesia was given. Success of IANB was defined as no pain during endodontic access preparation and root canal instrumentation. All diagnosis and injections were carried out by the same clinician, and the evaluation of effect of the treatment was conducted by an independent investigator, both of whom were blinded regarding the administered treatment.
Statistical Analysis
The data were recorded on a Microsoft Excel sheet (Microsoft Office Excel; Microsoft Corp, Redmond, WA, USA) for statistical evaluation using a commercial program (Mini Tab version 7.0). Age of the patient as well as initial and post-injection VAS scores were tabulated and compared using One-Way Anova and Post-Hoc Tests, Tukey pair wise, Paired t-test. The gender of the patients were compared by chi-square test. The significance level was set at p = 0.05 for these analyses. The percentage of successful IANB in the KETO, DP and PLAC groups were compared.
Results
The age, gender, initial VAS scores and tooth type were tabulated [Table/Fig-2,3,4 and 5]. There were no significant differences with respect to age (p =0.098), gender (p= 0.801) and pre-injection VAS scores (DP-KETO p =0.645, PLAC-KETO p =0.964, PLAC-DP p = 0.801) between the three groups [Table/Fig-3,4 and 5]. One hundred percent of the patients had subjective lip anaesthesia with the IAN blocks.
Distribution of teeth in the three groups.
| Tooth | KetorolacGroup(N=42) | DiclofenacPotassium(N=42) | Placebo(N=42) |
|---|
| First molar | 30 | 19 | 18 |
| Second molar | 12 | 23 | 24 |
| Parameter | Group I | Group II | Group III |
| Age (Mean ± SD) | 30.85 ± 8.67 | 30.40 ± 8.69 | 30.73 ± 7.83 |
*one-way Anova test
F-value = 0.03, p-value = 0.098, not significant.
Comparision of age between the three groups.
| Pair | p- value* |
|---|
| Age of DP-Age of KETO | 0.967, Not significant |
| Age of PLAC-Age of KETO | 0.998, Not significant |
| Age of PLAC-Age of DP | 0.982, Not significant |
*post-hoc tukey test, not significant
Gender distribution of patients studied for three groups.
| Gender | Group IKetorolacGroup(N=42) | Group IIDiclofenacPotassium(N=42) | Group IIIPlacebo(N=42) | All |
|---|
| Male | 23 | 20 | 22 | 65 |
| Female | 19 | 22 | 20 | 61 |
| Total | 42 | 42 | 42 | 126 |
*Chi-square =0.445, df =2, p-value = 0.801, not significant
Comparision of pre-injection VAS scores between the three groups.
| Pre-injection VAS score | p-value |
|---|
| DP - KETO | 0.645 |
| PLAC - KET0 | 0.964 |
| PLAC - DP | 0.801 |
*Post–hoc tukey test, there was no significant difference between the three groups.
There was statistically significant difference in the post-injection VAS scores between the three groups (DP-KETO p = 0.032, PLAC- KETO p= 0.000, PLAC-DP p = 0.008) [Table/Fig-6]. Also, the post-injection VAS Scores showed significantly lesser values (p= 0.000) than the pre-injections scores for all the three groups. The post-injection values was least in group I (KETO)-22.76 ± 15.41 followed by group II(DP)- 31.79 ± 16.93 & was maximum in group III (PLAC)-42.52±16.33 [Table/Fig-7]. The cold test elicited negative response in 100% of patients in all the three experimental groups.
Comparision of post-injection VAS scores between the three groups.
| Post-injecion VAS score | p-value |
|---|
| DP - KETO | 0.032 |
| PLAC - KETO | 0.000 |
| PLAC - DP | 0.008 |
*Post-hoc tukey test, there was significant difference between the three groups.
Comparision of pre-post injection VAS scores between the three groups.
| Parameter | Group I -KETO(Mean ± SD) | Group II -DP(Mean ± SD) | Group III -PLAC(Mean ± SD) |
|---|
| Pre-injection VAS | 85.74 ± 25.05 | 81.62 ± 18.34 | 84.55 ± 19.33 |
| Post-injection VAS | 22.76 ± 15.41 | 31.79 ± 16.93 | 42.52 ± 16.33 |
| p-value | 0.000 | 0.000 | 0.000 |
*Post-hoc tukey test, there was significant difference between the three groups.
On the basis of absence of pain during access and canal instrumentation, the percentage of successful IAN blocks were as follows: 76.19% (32 of 42 patients) for the KETO group, 54.76% (23 of 42 patients) for the DP group and 28.57% (12 of 42 patients) for the PLAC group [Table/Fig-8]. The percentage of successful IANBs was significantly higher in the KETO group when compared with the DP and the PLAC group [Table/Fig-9]. No adverse events were encountered during the study.
Comparison of percentage of successful cold test and inferior alveolar nerve block amongst the three groups.
| Cold testsuccessful (%) | IANB successful(%) |
|---|
| Ketorolac | 42 of 42 (100%) | 32 of 42 (76.19%) |
| Diclofeanc potassium | 42 of 42 (100%) | 23 of 42 (54.76%) |
| Placebo | 42 of 42 (100%) | 12 of 42 (28.57%) |
Inter group comparison of success inferior alveolarnerve block.
| IANB SUCCESS | p-value |
|---|
| KETO-DP | 0.034 |
| KETO-PLAC | 0.000 |
| DP-PLAC | 0.012 |
Discussion
The present study evaluated the efficacy of pre-medication with ketorolac and diclofenac potassium on the success of IANB. The results of the present study demonstrate that the success of IANB was significantly higher in patients pre-medicated with KETO when compared to DP or PLAC (p< 0.005).
Irreversible pulpitis is a clinical condition characterized by episodes of sharp shooting pain which lasts from a few minutes up to several hours. In this painful condition, the pulp is in a highly inflamed state often resulting in inadeqaute anaesthesia. Lowered pH as a result of the inflamed state of the tissue minimizes the amount of the available base form of the anaesthetic that penetrates the nerve sheath and membrane. This further reduces the ionized form of the anaesthetic within the nerve resulting in decreased anaesthesia. Moreover, nerves arising from the inflamed tissue have altered resting potentials and reduced excitability thresholds [12–14].
Also, the tetradotoxin-resistant (TTXr) class of sodium channels have been shown to be resistant to the action of these local anaesthetics [15]. A related factor is the increased expression of sodium channels in pulp diagnosed with irreversible pulpitis [16].
Two percent lidocaine was selected for this study because previous studies comparing lidocaine to other anaesthetics including articaine demonstrated little or no significant difference in the success rate of pulpal anaesthesia [11,17].
In 30-80% of patients with irreversible pulpitis a single IANB has not been found to be adequately effective requiring a supplemental anaesthesia to be given [18]. Researchers have suggested that an effective local anaesthesia may be obtained if the clinician prescribes NSAIDs as a premedication to reduce pulpal inflammation [19,20].
It is a commonly held belief that lip numbness implies pulpal anaesthesia; yet in two prior clinical trials, only 75% to 80% of the patients demonstrating lip numbness had experienced profound pulpal anaesthesia [21,22]. In the present study, 100% of the patients exhibited lip numbness due to accurate block anaesthesia which was capable of anaesthetizing the nerve fibers that supply the lip [23]. However, some of the patients experienced pain during access cavity preparation, thus indicating that lip numbness may not be an absolute indicator of pulpal anaesthesia, at least in inflamed pulps. Cold testing which was also performed following injection of local anaesthesia has been shown to cause contraction of the dentinal fluid resulting in a rapid outward flow within the patent tubules leading to a sharp sensation lasting the duration of the test. Studies have shown that cold testing may be considered more reliable than lip signs to determine when to initiate endodontic access in patients with irreversible pulpitis. However, it is important to note that negative response to cold testing does not necessarily indicate a successful IANB [24].
Success rate of IANB in an uninflamed pulp was reported to be 70% compared to 30% in teeth diagnosed with irreversible pulpitis [11,17,25–30]. The studies conducted to evaluate the success rate of IANB [11,26,31–36] demonstrate that successful execution of IANB may not always be adequate for performing root canal treatment on mandibular teeth.
Prostaglandins (PGs) have been found to up-regulate a variety of mechanisms that might decrease the efficacy of local anaesthetics. They alter the kinetics of activity of the voltage-gated sodium channels, resulting in increased depolarization; activation of extracellular G protein-coupled receptors namely P2 (Purinergic receptors) or EP3 receptors, which are expressed on trigeminal sensory neurons [37,38]. Prostaglandin levels are raised in inflamed pulps [39,40] and activation of nociceptors by PGs is a major cause for increased incidence of failure of (IANB) in patients with irreversible pulpitis [6,41]. Therefore, decreasing the amount of prostaglandins may increase the efficacy of local anaesthetics.
Ketorolac or ketorolac tromethamine is a (NSAID) from the family of heterocyclicacetic acid derivatives. It has been found to be as effective as morphine or meperidine for pain relief [42,43].
The proposed mechanisms for the efficacy of KETO include inhibition of conduction of C fibres, which are more resistant to local anaesthesia than A-delta fibres. Also, opening up of the K+ channels located within the primary afferent nerve endings results in antinociception and hence is a vital step in the peripheral antinociceptive effect of several NSAIDs. Activation of the Nitric oxide–cyclic Guanosine Monophosphate (GMP) pathway could induce antinociception through the opening of K+channels. Such a mechanism has been implicated for the antinociceptive action of ketorolac, which is responsible for increasing the success rate of IANB [44]. Diclofenac potassium, which is a benzoic acid derivative is a potent NSAID which significantly reduces pain within 15 to 30 minutes [45].
Research suggests that diclofenac can inhibit the thromboxane-prostanoid receptor, affect arachidonic acid release and uptake, inhibit lipoxygenase enzymes, and activate the nitric oxide–cGMP antinociceptive pathway [46]. The degree and duration of the damage of tissue and up-regulation of prostaglandins occurring before they are inhibited by the NSAIDs is also a factor in influencing the success of IANB [47].
Both KETO and DP effectively block prostaglandins, and have a relatively short half-life’s. However, the results of the present study demonstrate KETO to be more effective than DP in inhibition of prostaglandins hence making it a more effective analgesic.
However, these drugs have some inherent limitations; they cannot be administered in patients with peptic ulcers, renal failure, bleeding disorders, those allergic to NSAIDs.
Conclusion
Oral premedication with NSAIDs like KETO & DP if given 1 hour prior to administering inferior alveolar nerve block has been found to be helpful in reducing pain intensity and causing the block to be effective. However, oral pre-medication with 10 mg KETO may result in a significantly higher percentage of successful inferior alveolar block in patients with irreversible pulpitis in comparison to pre-medication with 50 mg DP.
*one-way Anova test
F-value = 0.03, p-value = 0.098, not significant.
*post-hoc tukey test, not significant
*Chi-square =0.445, df =2, p-value = 0.801, not significant
*Post–hoc tukey test, there was no significant difference between the three groups.
*Post-hoc tukey test, there was significant difference between the three groups.
*Post-hoc tukey test, there was significant difference between the three groups.
[1]. Reader A, Nusstein J, Drum M, Endodontic anaesthesia -Successful Local Anaesthesia for Restorative Dentistry and Endodontics 2011 Hanover Park IIQuintessence Publishings:131-48. [Google Scholar]
[2]. Mickel AK, Wright AP, Chogle S, Jones JJ, Kantorovich I, Curd F, An analysis of current analgesic preferences for endodontic pain managementJ Endod 2006 32:1146-54. [Google Scholar]
[3]. Gokin AP, Philip B, Strichartz GR, Preferential block of small myelinated sensory and motor fibres by lidocaine: in vivo electrophysiology in the rat sciatic nerveAnaesthesiology 2001 95:441-54. [Google Scholar]
[4]. Simpson M, Drum M, Nusstein J, Reader A, Beck M, Effect of combination of preoperative ibuprofen/acetaminophen on the success of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitisJ Endod 2011 37:593-97. [Google Scholar]
[5]. Ianiro SR, Jeansonne BG, McNeal SF, Eleazer PD, The effect of preoperative acetaminophen or a combination of acetaminophen and ibuprofen on the success of inferior alveolar nerve block for teeth with irreversible pulpitisJ Endod 2007 33:11-14. [Google Scholar]
[6]. Modaresi J, Dianat O, Mozayeni MA, The efficacy comparison of ibuprofen, acetaminophen-codeine, and placebo premedication therapy on the depth of anaesthesia during treatment of inflamed teethOral Surg Oral Med Oral Pathol Oral RadiolEndod 2006 02:399-403. [Google Scholar]
[7]. Bakshi R, Jacobs LD, Lehnert S, Picha B, Reuther J, A double blind, placebo controlled trial comparing the analgesic efficacy of two formulations of diclofenacin postoperative dental painCurr Ther Res Clin Exp 1992 52:435-42. [Google Scholar]
[8]. Berg J, Fellier H, Christoph T, Grarup J, Stimmeder D, The analgesic NSAID lornoxicam inhibits cyclooxygenase (COX)-1/-2, inducible nitric oxide synthase (iNOS), and the formation of interleukin (IL)-6 in vitroJ Inflamm Res 1999 48:369-79. [Google Scholar]
[9]. Schulz KF, Altman DG, Moher D, CONSORT 2010 statement: Updated guidelines for reporting parallel group randomized trialsJ pharmacol 2010 1:100-07. [Google Scholar]
[10]. Heft MW, Parker SR, An experimental basis for revising the graphic rating scale for painPain 1984 19:153-61. [Google Scholar]
[11]. Claffey E, Reader A, Nusstein J, Beck M, Weaver J, Anaesthetic efficacy of articaine for inferior alveolar nerve blocks in patients with irreversible pulpitisJ Endod 2004 30:568-71. [Google Scholar]
[12]. Wallace J, Michanowicz A, Mundell R, A pilot study of the clinical problem of regionally anaesthetizing the pulp of an acutely inflamed mandibular molarOral Surg Oral Med Oral Pathol Oral RadiolEndod 1985 59:517-21. [Google Scholar]
[13]. Byers M, Taylor P, Khayat B, Effects of injury and inflammation on pulpal andperiapical nervesJ Endod 1990 16:78-84. [Google Scholar]
[14]. Modaresi J, Dianat O, Soluti A, Effect of pulp inflammation on nerve impulse quality with or without anaesthesiaJ Endod 2008 34:438-41. [Google Scholar]
[15]. Roy M, Narahashi T, Differential properties of tetrodotoxin sensitive and tetrodoxin resistant sodium channels in rat dorsal root ganglion neuronsJ Neurosci 1992 12:2104-11. [Google Scholar]
[16]. Sorensen H, Skidmore L, Rzasa D, Comparison of pulpal sodium channel density in normal teeth to diseased teeth with severe spontaneous painJ Endod 2004 30:287 [Google Scholar]
[17]. Mikesell P, Nusstein J, Reader A, Beck M, Weaver J, A comparison of articaine andlidocaine for inferior alveolar nerve blocksJ Endod 2005 31:265-70. [Google Scholar]
[18]. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ, Anaesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine in irreversible pulpitisJ Endod 1998 24:487-91. [Google Scholar]
[19]. Averbach M, Katzper M, Baseline pain and response to analgesic medication of flurbiprofenJ Am Med Assoc 1986 80(Suppl 3A):41-49. [Google Scholar]
[20]. Dinnoe R, Campbell Copper S, Hall D, Buckingham B, Suppresion of postoperative pain by preoperative administration of ibuprofen in comparision to placebo, acetaminophen and acetaminophen plus codeineJ Clin Pharmacol 1983 23:37-43. [Google Scholar]
[21]. Fuss Z, Trowbridge H, Bender I, Rickoff B, Sorin S, Assessment of reliability of electric and thermal pulp testing agentsJ Endod 1986 12:301-05. [Google Scholar]
[22]. Petersson K, Soderstrom C, Kiani-Anaraki M, Levy G, Evaluation of the ability of thermal and electric tests to register pulp vitalityEndod Dent Traumatol 1999 15:127-31. [Google Scholar]
[23]. Endodontics –Colleagues for Excellence (2009) –American Association of Endodontics (AAE) [Google Scholar]
[24]. Textbook of Endodontology 2010 2ndWiley Blackwell publicationMedtizi – [Google Scholar]
[25]. Tortamano IP, Siviero M, Costa CG, Buscariolo IA, Armonia PL, A comparison of the anaesthetic efficacy of articaine and lidocaine in patients with irreversible pulpitisJ Endod 2009 35:165-68. [Google Scholar]
[26]. Cohen HP, Cha BY, Spångberg LS, Endodontic anaesthesia in mandibular molars: a clinical studyJ Endod 1993 19:370-73. [Google Scholar]
[27]. Goldberg S, Reader A, Drum M, Nusstein J, Beck M, Comparison of the anaesthetic efficacy of the conventional inferior alveolar, Gow-Gates, and Vazirani-Akinosi techniquesJ Endod 2008 34:1306-11. [Google Scholar]
[28]. Childers M, Reader A, Nist R, Beck M, Meyers WJ, Anaesthetic efficacy of the periodontal ligament injection after an inferior alveolar nerve blockJ Endod 1996 22:317-20. [Google Scholar]
[29]. Dagher BF, Yared GM, Machtou P, The anaesthetic efficacy of volumes of lidocaine in inferior alveolar nerve blocksJ Endod 1997 23:178-80. [Google Scholar]
[30]. Vreeland DL, Reader A, Beck M, Meyers W, Weaver J, An evaluation of volumes and concentrations of lidocaine in human inferior alveolar nerve blockJ Endod 1989 15:6-12. [Google Scholar]
[31]. Kennedy S, Reader A, Nusstein J, Beck M, Weaver J, The significance of needle deflection in success of the inferior alveolar nerve block in patients with irreversible pulpitisJ Endod 2003 29:630-33. [Google Scholar]
[32]. Matthews R, Drum M, Reader A, Nusstein J, Beck M, Articaine for supplemental buccal mandibular infiltration anaesthesia in patients with irreversible pulpitis when the inferior alveolar nerve block failsJ Endod 2009 35:343-46. [Google Scholar]
[33]. Reisman D, Reader A, Nist R, Beck M, Weaver J, Anaesthetic efficacy of the supplemental intraosseous injection of 3% mepivacaine in irreversible pulpitisOral Surg Oral Med Oral Pathol Oral Radiol Endod 1997 84:676-82. [Google Scholar]
[34]. Nusstein J, Reader A, Nist R, Beck M, Meyers WJ, Anaesthetic efficacy of the supplemental intraosseous injection of 2% lidocaine with 1:100,000 epinephrine irreversible pulpitisJ Endod 1998 24:487-91. [Google Scholar]
[35]. Bigby J, Reader A, Nusstein J, Beck M, Anaesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks in patients with irreversible pulpitisJ Endod 2007 33:7-10. [Google Scholar]
[36]. Lindemann M, Reader A, Nusstein J, Drum M, Beck M, Effect of sublingual triazolam on the success of inferior alveolar nerve block in patients with irreversible pulpitisJ Endod 2008 34:1167-70. [Google Scholar]
[37]. Vane JR, Botting RM, Mechanism of action of nonsteroidal anti-inflammatory drugsAm J Med 1998 104:2S-8S. [Google Scholar]
[38]. Gould HJ, England JD, Soignier RD, Nolan P, Minor LD, Liu ZP, Ibuprofen blocks changes in Na v 1.7 and 1.8 sodium channels associated with complete Freund’s adjuvant-induced inflammation in ratPain 2004 5:270-80. [Google Scholar]
[39]. Reuben SS, Duprat KM, Comparison of wound infiltration with ketorolac versus intravenous regional anaesthesia with ketorolac for postoperative analgesia following ambulatory hand surgeryReg Anaesth Pain Med 1996 21:565-68. [Google Scholar]
[40]. Hargreaves K, Goodis H, Seltzer S, Bender IB, The Dental Pulp 2002 4th edCarol Stream, ILQuintessence Publishing Co [Google Scholar]
[41]. Wells JE, Bingham V, Rowland KC, Hatton J, Expression of Nav1.9 channels in human dental pulp and trigeminal ganglionJ Endod 2007 33:1172-76. [Google Scholar]
[42]. Varrassi G, Marinangeli F, Agro F, Aloe L, De Cillis P, A double-blinded evaluation of propacetamol versus ketorolac in combination with patient-controlled analgesia morphine: analgesic efficacy and tolerability after gynecologic surgeryAnaesth Analg 1999 88:611-16. [Google Scholar]
[43]. Mrosczczak E, Jung D, Yee J, Bynum L, Sevelius H, Massey I, Ketorolac tromethamine pharmacokinetics and metabolism after intravenous, intramuscular, and oral administration in humans and animalsPharm 1990 10(6):33S-39S. [Google Scholar]
[44]. Lázaro-Ibáñez GG, Torres-López JE, Granados-Soto V, Participation of the nitric oxide–cyclic GMP–ATP-sensitive K+ channel pathway in The antinociceptive action of ketorolacEur J 2001 426:39-44. [Google Scholar]
[45]. Naushaba Q, Musculo-skeletal and joint disorders: Comprehensive handbook of drug prescription 2006 6th edManualQuaterly Medical Channel Karachi:720 [Google Scholar]
[46]. Gan TJ, Diclofenac: an update on its mechanism of action and safety profileCurr Med Res Opin 2010 26:1715-31. [Google Scholar]
[47]. Simmons DL, Botting RM, Hla T, Cyclooxygenase isozymes: the biology of prostaglandin synthesis and inhibitionPharmacol Rev 2004 56:387-437. [Google Scholar]