Residual ridge reduction after extraction is well known biological phenomenon and pattern of resorption is a well known fact [1]. Extensive resorption of mandibuar ridge results in shallow buccal vestibule and high insertion of mentalis muscle in relation to crest of the ridge, which leads to displacement of prosthesis [1–3]. Good functional denture or implant supported prosthesis needs adequate vestibular depth and attached gingiva. Many vestibular deepening techniques have been described since beginning of the era of surgery namely, Kazanjian, Godwin, Trauner, Clark, Obwegeser, Howe, Steinhauser, Tortorelli [4–12]. Vestibuloplasty repositions mucosa, muscle insertions, and increases denture flange area in turn stability of prosthesis [4]. All procedures are associated with varying degree of success. Disadvantages associated with existing procedures made the clinician to rethink for modifications, so that the modifications can overcome the disadvantages [13–16]. So, the study was planned to provide good attached gingiva and adequate vestibular depth using modified Kazanjian vestibuloplasty technique.
The study was aimed to evaluate efficacy of MKV technique for increasing vestibular depth in anterior mandible so that successful prosthesis can be delivered. Efficacy of technique was evaluated through operating time required, vestibular depth achieved, scarring or relapse and any postoperative complications associated with the healing.
Materials and Methods
Patients requiring vestibular deepening procedures presented to Department of Oral and Maxillofacial Surgery referred from Department of Prosthodontics, Sibar Institute of Dental Sciences, India and were randomly selected for the study group during 2013 to 2014.
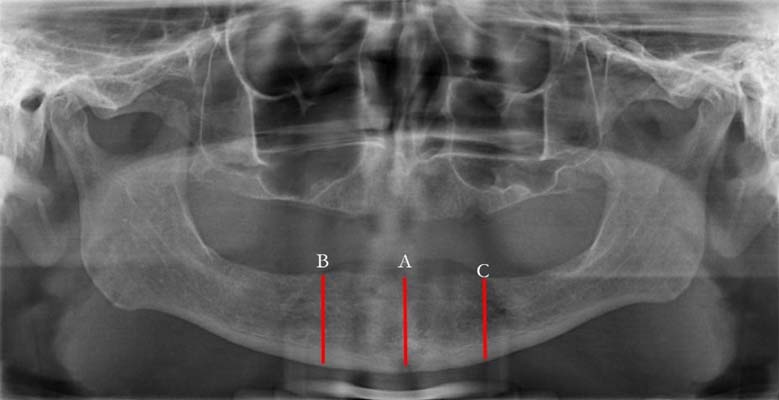
Selection Criteria: After clinical and radiographic examination, total of 10 patients with minimum 20mm of bone height and less than 5mm of vestibular depth were allocated for study protocol as determined by Department of Prosthodontics [Table/Fig-1]. Patient and attender were explained about surgical procedure and follow-up protocol to know their willingness for participation as volunteer for the study. Quality of oral mucosa was examined clinically and bone height was assessed radiographically. Radiographic assessment was performed using Sirona digital panoramic radiographic machine at predetermined points (midline, bilaterally just 2mm before mental foramen) by radiologist and surgeon [Table/Fig-2]. Indication for surgery was set by Department of prosthodontics. The minimum ridge height required for vestibular surgery ranged from 15-20 mm according to the published literature [2]. It is an essential bone height required to withstand normal occlusal forces and retention of prosthesis; which is a prerequisite to perform any vestibular deepening procedures [2]. Less bone height leads to compromised denture function, stability and inability to insert implants and sometimes may lead to fracture of hasal bone. Such bone deficiency requires augmentation surgery followed by deepening procedures [2]. So selection criteria opted was to have maximum amount of bone height required to deepen the vestibule without undue complications. Patients with ASA (American Society of Anaesthesiology) class I and II conditions were involved in the study. Patients with systemic disorders like hepatic, respiratory, cardiac, endocrine, or metabolic impairment which make the patient unfit for surgical procedure were excluded from study. Study protocol was approved by institutional ethical committee.
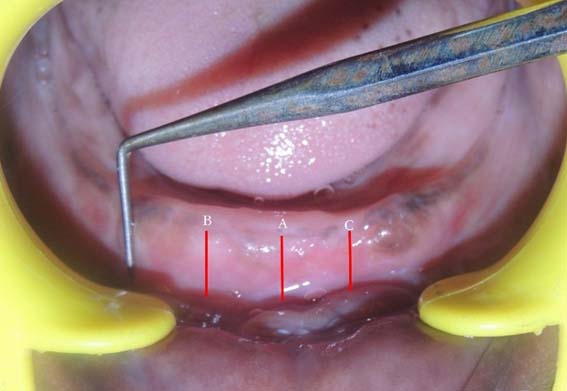
Intraoral photograph showing Preoperative Vestibular reference Markings at midline, bilaterally just before mental foramen.

Preoperative panoramic radiograph for measuring bone height.
Procedure was explained to healthy patient volunteers followed by informed consent. Preoperative clinical assessment was done using calipers and cast. Preoperative cast was arbitrarily scraped till the preplanned depth to prepare a clear acrylic surgical splint. Vestibuloplasty procedure was performed by single surgeon under local anaesthesia, postoperatively assessed by two observers. Both of them were blinded for time duration of follow-up to prevent bias.
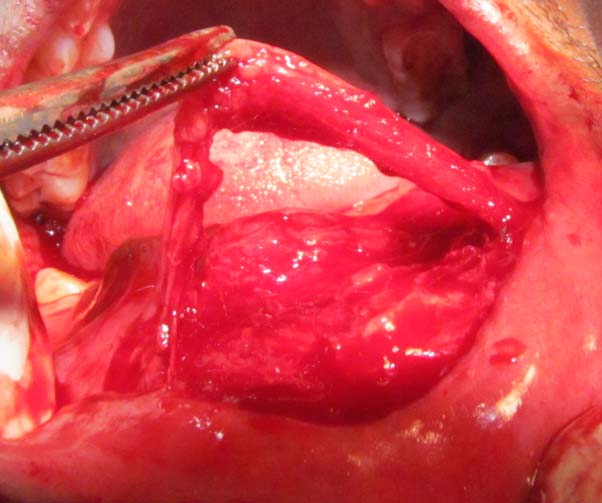
Surgical procedure: Modified Kazanjian vestibuloplasty was performed under local anaesthesia (Lignocaine-2% with 1:80000 adrenaline- Lignox-2% Indoco, India) developed by AL Belasy FA [13]. An intraoral Trans mucosal curvilinear incision was performed on alveolar ridge at the junction of attached mucosa [Table/Fig-3] till periosteum and another on labial mucosa approximately 12-15mm away from the attached mucosa between inter-foraminal area [Table/Fig-4]. Careful sharp supra periosteal dissection of muscle and connective tissue attachments were carried out till the desired depth. Bi-pedicled flap was elevated [Table/Fig-4]. The wound was irrigated with normal saline and local haemostasis was achieved. Flap was advanced apically and secured to desired depth of vestibule using poly ethylene tube; [Table/Fig-5] which was fixed to vestibular depth using percutaneous sutures around cotton rolls [Table/Fig-6]. Labial and alveolar sides of flap were sutured to the lip and periosteum respectively using horizontal mattress 3.0 silk sutures, starting from midline and ended bilaterally.
Intraoperative photograph showing mucosal incision.

Intraoperative photograph showing and labial incision bi-pedicled mucosal flap.
Intraoperative photograph showing polyethylene tube sutured to mucosal flap.

Intraoperative photograph showing final vestibular depth and placement of tube for suturing and percutaneous sutures in place extra orally.

Resultant raw surface was covered using betadine moistened gauze which was left for secondary epitheliazation. Dry gauze pack dressing was placed gently over the submental area to cover percutaneous sutures. All patients were put on Postoperative oral antibiotic and anti-inflammatory drugs (Cap.Amoxicillin-500mg 8th hourly and Tab. Ketorol DT, 12th hourly for 5 days). Patients were instructed to maintain soft diet and warm saline rinses after meals for minimum duration of four weeks.
Patients were examined during 1st week, 1st, and 3rd month follow up visits for healing and undue complications. The clinical evaluation included healing of mucosal flap, scarring of lip, effective vestibular depth achieved at first week, 1st month and 3rd month of surgery. Sutures & poly ethylene tube removal were done seven days postoperatively. The clinical parameters were evaluated consecutively for three months [Table/Fig-7] and for every six months up to 18 months after insertion of denture. Postoperative discomfort and pain was assessed using visual analogue scale. Sensation of lip and chin were assessed using two point discrimination. Depth measurements were done using digital caliper and metal scale. The comparison of pre and postoperative height were also done on pre and postoperative casts using standard metal scale [Table/Fig-8]. Clinically ridge was measured at three predetermined reference points i.e. midline, bilaterally just 2 mm before mental foramen [Table/Fig-9]. These points were checked by two investigators and data corrected for marking errors if any. Values were tabulated and analysed for test of significance (p value less than 0.05 was considered as statistically significant value). Data on demographics and denture satisfaction were recorded and computed for evaluation using modified questionnaire (Annexure-1) based on M Gargari et al., study [17].
Postoperative intraoral photograph showing desired vestibular depth with markings.
Postoperative photograph showing cast with metal scale in place for measurement of ridge height.

Showing vestibular depth at point A, B, and C. with different time intervals.
| Time points for follow up | Pre -op | Immediately After surgery | 1st week post op | 1st month post op |
|---|
| Groups | A1 | B1 | C1 | A2 | B2 | C2 | A3 | B3 | C3 | A4 | B4 | C4 |
| Minimum in mm | 1.00 | 2.50 | 2.50 | 4.00 | 6.00 | 6.00 | 5.00 | 7.00 | 7.00 | 3.50 | 6.00 | 6.00 |
| Maximum in mm | 4.50 | 5.00 | 6.00 | 20.00 | 20.00 | 20.00 | 16.00 | 15.00 | 15.00 | 14.00 | 14.00 | 14.00 |
| Mean | 3.25 | 3.55 | 3.55 | 11.25 | 11.55 | 11.65 | 9.90 | 9.70 | 9.95 | 8.70 | 8.95 | 8.75 |
| #SD | 0.98 | 0.76 | 0.98 | 5.18 | 4.55 | 4.69 | 3.38 | 2.79 | 8.75 | 3.54 | 3.17 | 2.93 |
| *p-Value | .00(S)** | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) | 0.000(S) |
# Standard deviation, * p-value less than 0.05 is considered statistically significant, S** - Significant
Patient satisfaction questionnaire modified from M. Gargari et al., study.
| Questionnaire for patient/ Grading | Poor | Not bad | Okay | Good | Excellent |
|---|
| How do you rate the aesthetics of your smile? | | | | | |
| How do you rate the quality of your mastication? | | | | | |
| How do you rate the facility of cleaning of the prosthesis? | | | | | |
| How do you rate the facility of removal and insertion of your denture? | | | | | |
| In the last year how many times did you need to change the prosthesis for trouble, fracture or other problems? | | | | | |
Results
Increased vestibular depth was seen with MKV technique. Average age of patients involved in the study was 56.75 years in males and 50.83 years in females [Table/Fig-10]. Postoperative depth obtained in relation to point A, B, and C were significant when compared to preoperative measurements [Table/Fig-9]. Healing of raw surface was seen in 60% of cases within a week and by the end of second week healing was satisfactory in all the cases [Table/Fig-11]. Scarring was minimal and postoperative pain score observed were ranged between 2-3 during 1st week and gradually reduced 0-1 at the end of 2nd week. All patients were completely relieved from the pain by the end of 3rd week.
Showing demographic data and mean time taken for surgery.
| Gender | Number of patients | Mean age in years | SD of Age # | Mean operating time in minutes | SD # |
|---|
| Female | 6 | 50.83 | 6.05 | 29.50 | 1.52 |
| Male | 4 | 56.75 | 22.54 | 29.00 | 4.24 |
| Total | 10 | 53.20 | 14.11 | 29.30 | 2.71 |
# Standard deviation
Showing healing and lip scarring at different time intervals.
| Parameters | Time Points | Description | No.of cases | % |
|---|
| Healing after | 1 week | Satisfactory | 6 | 60 |
| Unsatisfactory | 4 | 40 |
| Lip scaring | after 1 month | Positive | 4 | 40 |
| Negative | 6 | 60 |
Discussion
Ideal ridge should have adequate, uniform bone height without any protuberance, undercuts, sharp ridges, redundant soft tissue and hypertrophy [1,2]. Ridge should be free from any bone pathology [3–6]. Millard started pre prosthetic surgery for reduction of interdental papilla and alveolar margins immediately after extraction [3]. Later prototype vestibuloplasty was advocated by Kazanjian [4]. Many surgical procedures were described in published literature by clinicians with varying results [4–12]. Vestibuloplasty techniques can be generally categorized as mucosal advancement, secondary epithelization and grafting vestibuloplasty [2]. Physical status and age of patient are prime important factors for the selection of technique involved [2]. Success of sub mucosal vestibuloplasty depends on availability of adequate bone, free mobile mucosa so that deepening can be achieved without tension [7,8]. If mucosa available is not adequate or of poor quality then submucosal vestibuloplasty is not indicated. Instead secondary epithelization technique will be preferred [4–7].
Kazanjian first described secondary epithelization technique in mandible to overcome poor quality of mucosa viz. hyperplastic mucosa, scar tissue and so [4], labial incision performed and large flap reflected so that mucosal flap was transposed on to the bone and sutured to desired vestibular depth [2,4]. Raw surface of lip heeled by granulation, secondary epithelization and contracture [2,4]. Later Godwin modified Kazanjian technique by vestibular deepening through sub periosteal stripping instead of supra periosteal dissection [5]. Vestibular mucosa was placed against the bare bone and sutured to connective tissue by excising or pushing down periosteum and connective tissue [5]. Disadvantages associated with both the techniques are scar contracture and loss of sulcus depth [2,4,5]. Catheter and suture removal were done at 7-11 days postoperatively. To overcome the drawback of Kazanjian technique, Lipswitch vestibuloplasty was advocated. In this technique mucosal flap will cover the bare bone and periosteal flap will cover the labial side, so that epithelization of periosteum occurs in 2-3 weeks without scarring [2,9,15].
Further Clark and Obwegeser modified secondary epithelization technique [7,8]. Modifications were based on the principles of plastic surgery i.e. raw surface contracts less if covered with epithelium, raw surface overlying bone do not contract, sufficient undermining is necessary to prevent tension while fixing and firm fixation is necessary to prevent the relapse [2,7,8]. Clarks technique is considered reverse of Kazanjian as incision was made on the alveolar crest with supra periosteal dissection till desired depth. The mucosal flap was sutured to lip leaving the bone covered with periosteum for secondary epithelization [7]. Later Obwegeser modifies Clarks technique primarily for maxillary vestibuloplasty [8].
Tortorelli further modifies Clark’s technique as periosteal fenestration to prevent relapse at the base of the vestibule [11]. Periosteum was incised horizontally at the desired depth of vestibule and inferior periosteal margin elevated which was sutured to mucosal flap. So that bare bone healing was delayed by 2-3 weeks than bone covered with periosteum; this difference in healing period was effective in preventing relapse [11]. Later grafting vestibuloplasty advocated overcoming drawbacks associated with healing and patient discomfort during these periods [12]. Insufficient bone available for sub mucosal and overcorrection of secondary epithelization prompted the use of epithelial grafting [2,11]. Grafting requires second surgery to harvest graft under general anaesthesia which increases cost, hospitalization and patient discomfort [2]. Drawback of skin graft is hair growth in oral cavity and poor graft take up on exposed cortical bone [2]. Skin grafting procedure is technique sensitive. Xenografts were also tried with varying rate of success using porcine skin [2]. However, limitations of all surgical procedures involved once again made the rethinking for modification of existing techniques.
Kazanjian Technique is considered to be prototype and practiced by many surgeons. To overcome postoperative complications associated with Kazanjian technique, few modifications were suggested recently [13–16]. Even in the era of implant supported denture, successful denture rehabilitation require sound attached gingiva. Different surgical procedures were developed to create better anatomical environment and to create proper supporting structure for denture reconstruction. Ultimate goal is good functional rehabilitation and aesthetics. Our study was aimed to achieve this goal. So, we had performed AL Belasy’s MKV technique to validate published literature [13,15,16]. Vestibular depth obtained was in accordance with AL Belasy [13]. It also prevented sharp V depth of extended vestibule. In our study mean increase in vestibular depth was noted ranged from 11.25 mm to 11.65 mm one week postoperatively and 8.70mm to 8.95mm one month postoperatively at predetermined reference points and were statistically significant (p-0.000) [Table/Fig-8]. The results were better when compared to AL Belasy [13]. The mean or overall depth achieved was 10 mm which was statistically significant (p-0.000) [Table/Fig-9].
Mean operating time was 29.30 minutes [Table/Fig-10]. Complete healing of wound was observed at 28.2 +/- 2.1days. One patient with pus discharge showed complete healing after topical antibiotic ointment (Soframycin) application after seven days. The advantage with this technique is no relapse in the vestibular depth [13,16]. Our study showed well acceptance by patients. The amount of anterior vestibular depth attained was 10.4mm which was measured from most superior point. In our study we have not had much scarring which will alter the effective vestibular depth in contrast to results of AL Belasy [13].
Limitation
The study has few limitations like required minimum bone height was 20 mm. If it is less, then patient may require ridge augmentation before vestibular deepening procedures. The study sample was limited to few numbers of patients only. Single surgeon involved in the study protocol. It is a single center result. The lip length and laxity of lip tissue is one of the important factors for mobilization of flap. In case of short lower lip it’s difficult to get adequate width of flap. This factor has not been considered in the selection criteria which are crucial for aesthetics and lip competency. But in our study the lower lip length was within normal limits. The study warrants consideration of soft tissue parameters along with the height of bone to evaluate the aesthetic result. Also, the scar contracture of lip should be considered for the evaluation.
Conclusion
Modification of Kazanjian technique is worth to practice to achieve good results, which will nullify secondary relapse or necessity of free graft. It provides adequate attached gingiva for successful implant prosthesis. Over correction is not required as that of standard Kazanjian technique. Improved vestibular depth enabled better fabrication of denture flange and improved oral hygiene. Our study warrants long term follow up with multi centric randomized study with more number of patients and operators.
# Standard deviation, * p-value less than 0.05 is considered statistically significant, S** - Significant
# Standard deviation