Introduction
Geographic tongue (GT) is a benign harmless transient oral condition. It is also referred by various terminologies such as benign migratory glossitis, erythema migrans, annulus migrans and wandering rash of the tongue [1].
GT was first described as wandering rash of the tongue by Rayer in 1831 [2]. The characteristic pattern of the lesions gives the dorsal surface of the tongue the appearance of a map. The lesion persists for a period of time of several days to weeks depending on the individual and disappears only to reappear at a different location giving a different pattern [1]. Symptomatic GT is rare in children and may produce anxiety [3].
Case Report
In an annual dental screening camp, geographic tongue was noticed in three year male child. Clinically, lesions characteristic of geographic tongue were found on the anterior two thirds of the dorsal surface as well as lateral surface of the tongue [Table/Fig-1]. Oblate pattern was observed in the present case. He was unaware of condition and had no pain or discomfort. His parents were informed about the condition. No contributing history was elicited. However, oral examination revealed dental caries in relation to 51, 61, 74, 84 teeth. Patient was asymptomatic and since GT is a self limiting condition reassurance, plenty of fluid intake, restoration of carious teeth, and oral hygiene maintenance was advised. Patient’s parents were informed and a recall was advised after three months but patient didn’t turn up.
Red atropic areas surrounded by white circinate borders seen on lateral and dorsal surfaces of tongue.

Discussion
Epidemiology
Overall prevalence of geographic tongue is approximately 1-2.5% of the population [4]. The prevalence of GT in the paediatric population ranges from 0.37% to 14.3% with unknown aetiology [5,6].
In India, prevalence is 0.89% [7]. The highest incidence of about 39.4% occurs in the age group of 20-29 years [8]. GT is more frequently reported in adults than in children [9] while others believe it to be common in younger individuals [10]. Females are more commonly affected than males with the ratio of 1.5:1 [8]. Some studies have reported this condition to affect males more frequently [10].
Google and Medline literature search revealed the prevalence of geographic tongue in paediatric age group worldwide as shown in [Table/Fig-2] [4,8,9,11–39].
Prevalence of geographic tongue in Paediatric population worldwide [4,8,9,11–39].
| Author(s) | Country | Year | Prevalence of Geographic Tongue (%) |
|---|
| Rahamimoff [11] | Israel | 1957 | 14 |
| Togo et al., [12] | Japan | 1961 | 8 |
| Luigi [13] | Italy | 1963 | 28.7 |
| Redman [14] | USA | 1970 | 1.41 |
| Ghose et al., [15] | Iraq | 1982 | 43 |
| Kullaa et al., [16] | Finland | 1982 | 2.5 |
| Sawyer et al., [17] | Nigeria | 1984 | 3 |
| Sedano et al., [18] | Mexico | 1989 | 1.9 |
| Kleinman et al., [19] | Denmark | 1994 | 0.6 |
| Arendorf et al., [20] | South Africa | 1996 | 1.6 |
| Bezerra et al., [21] | Brazil | 2000 | 21 |
| Voros-Balog et al., [22] | Hungary | 2003 | 5.7 |
| Rabiei [23] | Iran | 2003 | 13.4 |
| Avcu & Kanli [24] | Turkey | 2003 | 1.2 |
| Sanei [25] | Iran | 2003 | 6.2 |
| Sadolah et al., [26] | Iran | 2003 | 3 |
| Garcia-Pola et al., [27] | Spain | 2002 | 4.48 |
| Bessa et al., [28] | Brazil | 2004 | 9.8 |
| Shulman et al., [4] | USA | 2005 | 1.05 |
| Jainkittivong et al., [8] | Thailand | 2005 | 39.4% (both C+A) |
| Ugar-Cankal et al., [29] | Turkey | 2005 | 1.8 |
| Khozeimeh et al., [30] | Iran | 2006 | 4.9 |
| Mozarrad & Viziri [31] | Iran | 2008 | 27 |
| Mathew et al., [32] | Southern India | 2008 | 0.84 |
| Byahatti et al., [33] | India | 2010 | 17.2 (both C+A) |
| Darwazeh et al., [9] | Jordan | 2011 | 4.8 |
| Ambika et al., [34] | India | 2011 | 1.4 |
| Yilmaz et al., [35] | Turkey | 2011 | 2.68 |
| Jahanbani et al., [36] | Iran | 2012 | 0.8 |
| Madera et al., [37] | Colombia | 2013 | 0.8 |
| Patil et al., [38] | India | 2013 | 16.4 (both C+A) |
| Rezai et al., [39] | Iran | 2015 | 7.86% (both C+A) |
C-Children, A-Adults.
Aetiopathogenesis
The aetiopathogenesis of the geographic tongue remains unknown till date. Some investigators have classified it as congenital anomaly while others said it to be a hereditary disorder [40]. Few authors believed it to be a chronic inflammatory condition [40]. Several aetiological factors have been suggested.
Hereditary factors: Siblings of one parent affected by geographic tongue revealed significantly higher prevalence of geographic tongue than those siblings of unaffected parents suggesting the role of familial and hereditary factors [41].
Assessment of histocompatability antigens among GT patients revealed significantly increased DR5 and DRW6 antigens in serum of GT patients when compared to controls while DR2 was reduced comparartively [42]. Recently, GT in five-year-old monozygotic twins with mild pain and discomfort on consumption of spicy food was reported supporting the genetic aetiology [43].
Association with other systemic diseases: GT is commonly associated with other systemic diseases such as atopy, allergy, stress, anaemia, psoriasis, gastrointestinal disturbances and hormonal variations [1,40]. It may be associated with syndromes like Reiter’s syndrome, Down syndrome, Aarskog syndrome, Fetal hydantoin syndrome and Robinow’s syndrome [1,44]. But none have shown a definite causal relationship.
Asthma/Atopy: Marks and Tait demonstrated an increased incidence of tissue type HLA- B15 in atopic patients with geographic tongue which provided an additional support for genetic basis.
They observed a positive association between GT and atopy/asthma which led the authors to postulate a similar pathogenesis for both the disease entities [45]. GT was more commonly found in patients with allergies to drugs, food or others in a study conducted by Jainkittivong et al., [8].
Association with psoriasis: Due to similarities in clinical, histopathologic and immunohistochemical findings, few researchers consider geographic tongue as as oral manifestation of psoriasis. Histopathologic similarity may support the hypothesis that GT may be considered as an expression of oral psoriasis.
Few studies have concluded that GT is an oral manifestation of psoriasis [46,47] while others argue that it is not [48]. Highly significant association with Human Leukocyte Antigen (HLA)-Cw6 and weakly significant association with B13 in both GT and psoriasis are reported [49].
Recently Tarakji et al., in their review have mentioned that GT is more common in psoriatic patients however a strong evidence is still lacking [50].
Few authors concluded that GT and psoriasis do not share a common aetiology and rather occur co-incidentally [51,52].
A case-control study in India examined 600 adult patients with psoriasis and revealed a strong association between psoriasis and GT. Authors concluded that GT more frequently affects males and those patients with severe psoriasis [10].
Significant occurrence of GT in early onset psoriasis and fissured tongue in late-onset psoriasis was observed in a recent study. Authors believed that GT could be used as a marker of the severity of psoriasis [53].
Association with fissured tongue: Significant co-existence of GT and fissured tongue was noticed in 60.1% patients in a study conducted by Jainkittivong et al., [8]. Ghose et al., suggested a genetic linkage between these two conditions [15].
GT and fissured tongue may share a common genetic aetiology. Deep fissures on the dorsum of the tongue ensure stagnation and subsequent development of glossitis [8].
GT and fissured tongue have been reported in association with chronic granulomatous disease [54].
Psychosomatic factors and stress: Psychosomatic factors appear to have significant role in the aetiology of GT. Redman et al., demonstrated higher prevalence of geographic tongue in mentally ill patients [14].
Ebrahimi et al., demonstrated the association between the stress and geographic tongue. They also found that decreasing stress in geographic tongue patients can be helpful in healing the lesions [55].
Psychological factors, such as stress, may represent a potentially modifiable risk factor that could influence the frequency of recurrence of GT in adults [56]. Stoopler et al., in their clinical observation suggested that these factors may be associated with GT even in the paediatric population similar to the adult population [57].
Hormonal factors: Wysocky and Daley found association between the geographic tongue and diabetes and found fourfold increase in the prevalence of geographic tongue in diabetic patients. They found a prevalence of 8% in type 1 diabetic patients [58]. On the contrary, Guggenheimer et al., reported no significant correlation between geographic tongue and insulin dependent diabetes mellitus [59].
Drug induced: Geographic tongue may develop as a result of hormonal fluctuation. Women on oral contraceptive pills have shown to develop GT lesions which got severe on the seventeenth day of the cycle [60].
Drug induced GT due to angiogenesis inhibitors has also been reported. Authors believed that therapeutic inhibition of VEGF or its receptors in oral mucosa by the drugs could induce GT [61].
Tobacco smoking: A protective influence of smoking has been observed since smokers had less prevalence of geographic tongue than nonsmokers [4,24].
Vitamin defeciency: Deficiency of vitamin B6, B12, folic acid, iron and zinc have been proposed to be contributing factors as well [37,40].
Recent aetiopathogeneis according to dynamics based on physics: Recently in 2015, Seiden and Curland explained geographic tongue in terms of media dynamics based on physics. They observed different evolutionary phases between “a healed (rest) state, a highly inflamed (excited) state, and a healing (recovering state)”. Similarities between dynamics of GT and other excitable media such as forest fires, cardiac arrhythmias, chemically driven reaction-diffusion systems and morphogenesis in multicellular organisms was noted by the authors [62]. There exist different patterns of geographic tongue – oblate pattern, wavy 1D pattern and a ring shaped concentric pattern. Seiden and Curland have explained dynamics of circular or oblate or closed pattern which are more typically observed and secondly spiral or open ended pattern [Table/Fig-3] [62].
Different clinical patterns of geographic tongue - Oblate or circular pattern (A), Spiral pattern (B), Wavy 1 D pattern (C)
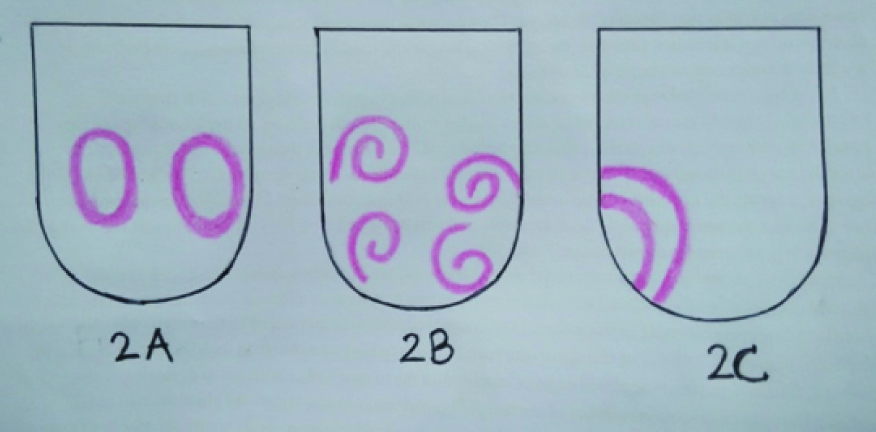
In circular pattern, shape of lesions will remain same as they expand on tongue unless there is some obstacle or inhomogenity in the epithelium. If circular pattern is exhibited in a patient it is more likely that tongue is gradually affected and subsequently healed [62].
While spiral patterns tend to be self-sustaining and will linger for a longer duration of time. These patterns result due to inhomogenities in the medium or due to external intervention in other excitable media. However, in GT more studies are further needed.
Apart from its unique composition, tongue is also exposed to external conditions like temperature variations with different foods, rubbing of tongue’s edge against teeth or gums which may trigger the phenomenon in GT. They also observed GT in a one-year-old boy with teething supporting the environmental origin [62].
Clinical Presentation
Lateral margins and tip of the tongue are the most commonly involved sites followed by dorsal and ventral surfaces [8]. If the lesions occur in different sites other than tongue, then the term ectopic geographic tongue is employed as first coined by Crooke in 1955 [1]. The extra glossal sites include the labial mucosa, buccal mucosa, gingival floor of the mouth, soft palate and uvula. GT is also known by various names such as geographic stomatitis, wandering rash of tongue, erythema migrans, benign migratory glossitis and stomatitis areata migrans [2].
Clinically, lesion of the geographic tongue reveal erythematous atrophic areas with loss of filiform papillae surrounded by the white circinate borders [1].
Periods of remission and exacerbation of varying duration are usually evident. The lesion recurs in the new locations thereby producing the migrating pattern. Continuously changing patterns and migration of lesions on the tongue surface with unusual appearance of the tongue are the usual chief complaints of the patient [8,40].
GT can occur either as isolated or multiple lesions, can be asymptomatic or present with symptoms like pain, burning sensation, discomfort, dysgeusia, sensitivity to hot, spicy and sour food pain in ears or ipsilateral submandibular lymphadenopathy [8,40]. Majority of the patients will be asymptomatic. Two symptomatic cases in paediatric age group with environmental allergies presenting with oral discomfort, increased salivation, altered taste, pain while eating and drinking were reported by Sigal et al., [40].
Regezi et al., suggested that presence of deep fissures infected with candida organisms could be responsible for symptoms [63]. However, this has to be further investigated.
Histopathology
Microscopic examination reveals a thick keratin layer infiltrated by mixed inflammatory cell infiltrate, thin elongated rete ridges and epithelial oedema. The inflammatory cells produce small micro abscesses called Monro’s abscesses in the keratin and spinous layer. Superficial areas may reveal candidal hyphae and spores [63]. Areas corresponding to the red patches show increased oedema, acanthotic epithelium and complete absence of filiform papillae [7]. The areas from the centre of the atrophic areas show complete absence of filiform papillae and parakeratotic layers. The elevated white borders include subepithelial infiltration of neutrophils, micro abscesses, leukocyte invasion into the epithelium, intraepithelial oedema, acantholysis, glycogen deposits in the epithelial cells and exfoliation of necrotic cells in the surface layer [64].
Under scanning electron microscopy, two types of abnormal mucosa have been demonstrated from the surface of geographic tongue: an atropic area on which the extensions of filliform papillae are absent but the bodies appear typical and the white margin of desquamating cells. Micro fissures were observed between the atrophic and normal mucosa [65].
Differential Diagnosis
GT is usually diagnosed by its characteristic history and unique clinical features. Histologic confirmation is rarely needed. In case of atypical lesions, differential diagnosis of GT includes atrophic candidiasis, neutropenia, psoriasis, Reiter’s syndrome, leukoplakia, lichen planus, systemic lupus erythematosus, herpes simplex and drug reaction [7,66]. Isolated/solitary geographic tongue lesions may sometimes show striking resemblance to leukoplakia which is a precursor to squamous cell carcinoma of tongue (at times causing cancerophobia in patients), in which case the risk factors that are associated with oral cancer (such as old age, alcohol consumption, and tobacco use) are not associated with GT [5,67].
If the clinician encounters a solitary ulcer on the oral mucosa, the first consideration should be conditions associated with ulcers of short duration (less than 3 weeks), including trauma, recurrent aphthous ulcer, infection, and vesiculobullous disease. If the ulcer persists beyond three weeks after removing any local irritants, consideration should be given to chronic trauma, chronic infection, major aphthous ulcer, gumma (from syphilis), and leukoplakia.
Investigations are required if diagnosis of GT cannot be made by history and examination due to atypical and symptomatic presentation. Blood investigations would rule out anaemia and neutropenia, while Periodic acid Schiff stained cytosmears can rule out candidiasis. If a definite diagnosis is still not made then biopsy from most representative area is warranted to rule out cancerphobia in patients [5,7,40].
Treatment
Geographic tongue typically does not require any treatment if asymptomatic. Periodic follow up to confirm diagnosis is required in case of first visit and when history is unclear. Reassure the patient about the benign and self-limiting nature of the lesion. If there is excessive pain and discomfort, medications like analgesics such as acetoaminophen, anti-inflammatory drugs, antihistamines like diphenhydramine hydrochloride, mouth rinses with topical anaesthetics like lidocaine gel, topical corticosteroids like betamethosone, cyclosporine, vitamin A therapy like tretinion, zinc and vitamin K2 supplements can be advised [1,68,69]. Complete reversal of condition has been noted after a few weeks of supplements.
Topical Tacrolimus application has been effective in recalcitrant cases [70]. Satisfactory improvement was observed by systemic administration of cyclosporine microemulsion pre-concentrate, with initial dose of 3mg/kg/day and maintenance dose of 1.5mg/kg/day two months later [71].
Discomfort from the geographic tongue can be limited or avoided by avoiding alcohol, tobacco products, hot, spicy and sour foods, acidic fruits and beverages, toothpaste that contains tartar control additives, heavy flavouring or whitening agents, dried, salty nuts which may aggravate the condition [67]. However, none of these treatments have been effective.
Conclusion
Geographic tongue is a benign condition of uncertain aetiology. The clinical presentation may cause anxiety in young patients as well as parents. Reassurance and follow up of patients especially in Paediatric population is needed to know about effective treatment modalities.
[1]. Hooda A, Rathee M, Gulia JS, Yadav SPS, Benign migratory glossitis: a reviewThe Internet Journal of Family Practice 2011 9(2):1528-8358.ISSN: [Google Scholar]
[2]. Prinz H, Wandering rash of the tongue (Geographic tongue)Dent Cosmos 1927 69:272-75. [Google Scholar]
[3]. Goswami M, Verma A, Verma M, Benign migratory glossitis with fissured tongueJ Indian Soc Pedod Prev Dent 2012 30:173-75. [Google Scholar]
[4]. Shulman JD, Prevalence of oral mucosal lesions in children and youths in USAInt J Paediatr Dent 2005 2:89-97. [Google Scholar]
[5]. Banoczy J, Szabo L, Csiba A, Migratory glossitis. A clinical histologic review of seventy casesOral Surg Oral Med Oral Pathol 1975 39:113-21. [Google Scholar]
[6]. Pinto A, Haberland CM, Baker S, Paediatric soft tissue oral lesionsDent Clin North Am 2014 58:437-53. [Google Scholar]
[7]. Desai VD, Baghla P, Asymptomatic reversible lesion on tongue – case series in paediatric patientsJ Adv Med Dent Scie 2014 2(2):176-79. [Google Scholar]
[8]. Jainkittivong A, Lanlais RP, Geographic tongue: clinical characteristics of 188 casesJ Contemp Dent Pract 2005 1:123-35. [Google Scholar]
[9]. Darwazeh AMG, Almelaih AA, Tongue lesions in a Jordanian population. Prevalence, symptoms, subject’s knowledge and treatment providedMed Oral Patol Oral Cir Bucal 2011 16(6):e745-49. [Google Scholar]
[10]. Singh S, Nivash S, Mann BK, Matched case-control study to examine association of psoriasis and migratory glossitis in IndiaIndian J Dermatol Venereol Leprol 2013 79:59-64. [Google Scholar]
[11]. Rahamimoff P, Muhsam HV, Some observations of 1,246 cases of geographic tongueAm J Dis Child 1957 93:519-25. [Google Scholar]
[12]. Togo T, Clinical study on geographic tongueKurume Med J 1961 24:1156-72. [Google Scholar]
[13]. Luigi G, Indagine clinico-statistica sulla frequenze della lingua scrotale della linguageografica della linguanera villosa della glossite rombica mediana della anchiloglossia e del torus palatinus in 3274 stoma topazientiRass Int Stomatol 1968 19:261-68. [Google Scholar]
[14]. Redman RS, Prevalence of geographic tongue, fissured tongue, median rhomboid glossitis and hairy tongue among 3611 Minnesota school childrenOral Path 1970 30:390-98. [Google Scholar]
[15]. Ghose LJ, Baghdady VS, Prevalence of geographic and plicated tongue in 6090 Iraqi school childrenCommunity Dent Oral Epidemiol 1982 10:214-16. [Google Scholar]
[16]. Kullaa-Mikkonen A, Mikkonen M, Kotilainen R, Prevalence of different morphologic forms of the human tongue in young FinnsOral Surg 1982 53:152-56. [Google Scholar]
[17]. Sawyer DR, Taiwo EO, Mosadomi A, Oral anomalies in Nigerian childrenCommunity Dent Oral Epidemiol 1984 12:269-73. [Google Scholar]
[18]. Sedano HO, Freyre CI, Garza ML, Clinical orodental abnormalities in Mexican childrenOral Surg Oral Med Oral Path 1989 68:300-11. [Google Scholar]
[19]. Kleinman DV, Swango PA, Pindborg JJ, Epidemiology of oral mucosal lesions in United States school childrenCommunity Dent Oral Epidemiol 1994 22:243-53. [Google Scholar]
[20]. Arendorf TM, Van der Ross R, Oral lesions in a black pre- school South African populationCommunity Dent Oral Epidemiol 1996 24:296-97. [Google Scholar]
[21]. Bezerra S, Isabel C, Oral conditions in children from birth to 3 yearsJ Clin Paediat Dent 2000 25:79-81. [Google Scholar]
[22]. Voros-Balog T, Vincze N, Banoczy J, Prevalence of tongue lesions in Hungarian childrenOral Dis 2003 9:84-87. [Google Scholar]
[23]. Rabiei M, Mohtashami Amiri Z, Masoodi Rad H, Niazi M, Niazi H, Frequency of tongue anomalies in primary school of LahidjanJ Med Facul Guilan Univers 2003 12(45):36-42. [Google Scholar]
[24]. Avcu N, Konli A, The prevalence of tongue. lesions in 5150 Turkish dental out PatientsOral Dis 2003 9:188-93. [Google Scholar]
[25]. Sanei AS, Epidemiologic study of geographic tongue in population of TehranBeheshti Univ Dent J 2000 16(2):210-15. [Google Scholar]
[26]. Sadolah S, Mahboob Roshankar R, Study of burning sensation of geographic and fissured tongue in school childrenTeb Tazkeih 1995 17:43-46. [Google Scholar]
[27]. Garcia-Pola MJ, Garcia JM, Gonzalez M, Prevalence of oral lesions in the six-year-old paediatric population of Oviedo (Spain)Medicina Oral 2002 7:184-91. [Google Scholar]
[28]. Bessa CFN, Santos PJB, Aguiar CF, do Carmo MAV, Prevalence of oral mucosal alterations in children from 0 to 12-year-oldJ Oral Pathol Med 2004 33:17-22. [Google Scholar]
[29]. Ugar-Cankal D, Denizci S, Hocaoglu T, Prevalence of tongue lesions among Turkish school childrenSaudi Med J 2005 26(12):1962-67. [Google Scholar]
[30]. Khozeimeh F, Rasti G, The prevalence of tongue abnormalities among the school children in Borazjan, IranDent Res J 2006 3(1):1-6. [Google Scholar]
[31]. Mojarrad F, Vaziri PB, Prevalence of tongue anomalies in Hamadan, IranIranian J Publ Health 2008 37(2):101-15. [Google Scholar]
[32]. Mathew AL, Pal KM, Sholapurkar AA, Vengal M, The prevalence of oral mucosal lesions in patients visiting a dental school in Southern IndiaIndian J Dent Res 2008 19:99-103. [Google Scholar]
[33]. Byahatti SM, Ingafou MSH, The prevalence of tongue lesions in Libyan adult patientsJ Clin Exp Dent 2010 2(4):e163-68. [Google Scholar]
[34]. Ambika L, Keluskar V, Hugar S, Patil S, Prevalence of oral mucosal lesions and variations in Indian public school childrenBraz J Oral Sci 2011 10(4):288-93. [Google Scholar]
[35]. Yilmaz AE, Gorpelioglu C, Sarifakioglu E, Dogan Bilici M, Celik N, Prevalence of oral mucosal lesions from birth to two yearsNigerian Journal of Clinical Practice 2011 14(3):349-53. [Google Scholar]
[36]. Jahanbani J, Morse DE, Alinejad H, Prevalence of oral lesions and normal variants of the oral mucosa in 12 to 15-year-old Students in Tehran, IranArch Iran Med 2012 15(3):142-45. [Google Scholar]
[37]. Madera AMV, Malagón MDCJ, Ricardi LML, Prevalence of tongue alterations and related factors in children attending the University of Cartagena, ColombiaRevista Odontológica Mexicana 2013 17(4):231-35. [Google Scholar]
[38]. Patil S, Kaswan S, Rahman F, Doni B, Prevalence of tongue lesions in the Indian populationJ Clin Exp Dent 2013 5(3):e128-32. [Google Scholar]
[39]. Rezaei F, Safarzadeh M, Mozafari H, Tavakoli P, Prevalence of geographic tongue and related predisposing factors in 7-18-year-old students in Kermanshah, Iran 2014Global Journal of Health Science 2015 7(5):91-95. [Google Scholar]
[40]. Sigal MJ, Mock D, Symptomatic benign migratory glossitis. Report of two cases and literature reviewPaediatr Dent 1992 14:392-96. [Google Scholar]
[41]. Eidelman E, Chosack A, Cohen T, Scrotal tongue and geographic tongue: polygeneic and associated triatsOral Surg Oral Med Oral Pathol 1976 42:591-96. [Google Scholar]
[42]. Fenerli A, Papanicolaou S, Papanicolaou M, Laskaris G, Histocompatability antigens and geographic tongueOral Surg Oral Med Oral Pathol 1993 76:476-79. [Google Scholar]
[43]. Gunashekar M, Geographic tongue in monozygotic twinsJ Clin Diagn Res 2014 8(4):ZD01-02. [Google Scholar]
[44]. Cerqueira DF, de Souza IP, Orofacial manifestation of a patient with Robinow’s syndrome. A case report in paediatric patientOral Surg Oral Med Oral Pathol Oral Radiol Endod 2008 105:353-57. [Google Scholar]
[45]. Marks R, Tait B, HLA antigens in geographic tongueTissue Antigens 1980 15:6-62. [Google Scholar]
[46]. Pogrel MA, Cram D, Intraoral findings in patients with psoriasis with a special reference to geographic tongue (erythema circinata)Oral Surg Oral Med Oral Pathol 1988 66:184-89. [Google Scholar]
[47]. Zargari O, Prevalence and significance of fissured tongue and geographical tongue in psoriatic patientsClin Exp Dermatol 2006 2:192-95. [Google Scholar]
[48]. Miloğlu O, Göregen M, Akgül HM, Acemoğlu H, The prevalence and risk factors associated with benign migratory glossitis lesions in 7619 Turkish dental outpatientsOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 107:e29-33. [Google Scholar]
[49]. Gonzaga HF, Torres EA, Alchorne MM, Gerbase-Delima M, Both psoriasis and benign migratory glossitis are associated with HLA-CW6Br J Dermatol 1996 135:368-70. [Google Scholar]
[50]. Tarakji B, Umair A, Babaker Z, Azzeghaiby SN, Gazal G, Sarraj F, Relation between psoriasis and geographic tongueJ Clin Diagn Res 2014 89110:ZE06-07. [Google Scholar]
[51]. Vanderwaal I, Pindborg J, Diseases of tongue 1986 ChicagoQuintessence Publishing:43-46. [Google Scholar]
[52]. Raghoebar GM, de Bont LG, Schoots CJ, Erythema migrans of the oral mucosa. report of two casesQuintessence Int 1988 19:809-11. [Google Scholar]
[53]. Picciani BLS, Souza TT, Santos VCB, Domingos TA, Carneiro S, Avelleira JC, Geographic tongue and fissured tongue in 348 patients with psoriasis: Correlation with disease severityScientific World Journal 2015 2015:564326:1-7. [Google Scholar]
[54]. Dar-Odeh NS, Hayajneh WA, Abu-Hammad OA, Hammad HM, Al-Wahadneh AM, Bulos NK, Orofacial findings in chronic granulomatous disease. Repot of twelve patients and review of literatureBMC Res Notes 2010 3:37 [Google Scholar]
[55]. Ebrahimi H, Pourshahidi S, Tadbir AA, Shyan SB, The relationship between geographic tongue and stressIRCMJ 2010 12(3):313-05. [Google Scholar]
[56]. Alikhani M, Khalighinejad N, Ghalaiani P, Khaleghi MA, Askari E, Gorsky M, Immunologic and psychological parameters associated with geographic tongueOral Surg Oral Med Oral Pathol Oral Radiol 2014 118:68-71. [Google Scholar]
[57]. Stoopler ET, Jaisri RT, Sollectio TP, Psychological parameters associated with geographic tongue: a clinical observationOral Surg, oral Med, Oral Pathol Oral Radiol 2015 119(1):122-03. [Google Scholar]
[58]. Wysocki GP, Daley TD, Benign migratory glossitis in patients with juvenile diabetesOral Surg Oral Med Oral Pathol 1987 63:68-70. [Google Scholar]
[59]. Guggenheimer J, Moore PA, Rossie K, Myers D, Mongelluzzo MB, Block HM, Insulin dependent diabetes mellitus and oral soft tissue pathologies. I. prevalence and characteristics of non-candidal lesionsOral Surg Oral Med Oral Pathol Endod 2000 89:563-09. [Google Scholar]
[60]. Waltimo J, Geographic tongue during a year of oral contraceptive cyclesBr Dent J 1991 171:94-96. [Google Scholar]
[61]. Hubiche T, Valenza B, Chevreau C, Fricain JC, Giudice PD, Sibaud V, Geographic tongue induced by angiogenesis inhibitorsThe Oncologist 2013 18:e16-7. [Google Scholar]
[62]. Seiden G, Curland S, The tongue as an excitable mediumNew J Phys 2015 17:1-8. [Google Scholar]
[63]. Regezi JA, Sciubba JJ, Oral Pathology. Clinico-Pathologic correlations 1993 PhiladelphiaWB Saunders:150-151. [Google Scholar]
[64]. Plackova A, Skach M, The ultrastructure of geographic tongueOral Surg Oral Med Oral Pathol 1975 40:760-68. [Google Scholar]
[65]. Kullaa-Mikkonen A, Geographic tongue: An SEM studyJ Cutan Pathol 1986 13:154-62. [Google Scholar]
[66]. Assimakopoulos D, Patrikakos G, Fotika C, Elisaf M, Benign migratory glossitis or geographic tongue: an enigmatic oral lesionAm J Med 2002 113:751-55. [Google Scholar]
[67]. Greer RO, Pathology of malignant and pre-malignant oral epithelial lesionsOtolaryngol Clin North Am 2006 39:249-75. [Google Scholar]
[68]. Helfman RJ, The treatment of geographic tongue with topical retin-A solutionCutis 1975 50:41-46. [Google Scholar]
[69]. Gibson J, Geographic tongue: The clinical response to zinc supplementationJ Trace Elem Experim Med 1990 3:203-08. [Google Scholar]
[70]. Ravi Prakash SM, Sankalp V, Rajendra P, Udita S, Tacrolimus: a novel approach against wandering rash- A pilot studySPJTS 2014 2(1):269-73. [Google Scholar]
[71]. Abe M, Sogabe Y, Syuto T, Ishibuchi H, Yokoyama Y, Ishikawa O, Successful treatment with cyclosporine administration for persistent benign migratory glossitisJ Dermatol 2007 34:340-43. [Google Scholar]