Introduction
Patient’s whose floor of the mouth has been resected usually undergo immediate reconstruction with local flap, skin graft, distant flap or micro vascular free tissue transfer. Although the shape of the tongue can be more or less built. Its movement is restricted by defects of the body or frenum, attachment of the flap, residual tongue or postoperative scar ring. Each of these restrictions results in dysfunction of mastication, deglutition and speech [1].
Mastication aids by directly crushing the food against the rugae of the hard palate. The muscles of the cheek and tongue control the food bolus by repositioning it onto the occlusal surfaces after each chewing stroke, after that, saliva mixes into the bolus [2]. Sensory nerve endings in the tongue help distinguish the texture and consistency of the food. When the bolus is ready for swallowing, the tongue helps in debridement of food in the buccal vestibule and the floor of the mouth [3].
Swallowing is composed of three stages: oral, pharyngeal and oesophageal. The oral phase is under voluntary neuromuscular control and the later two phases are under involuntary neuromuscular control [4]. During the oral phase of deglutition, the tongue gathers food into a bolus and positions the bolus between the dorsum of the tongue and the hard palate. As the middle tongue and palate contacts, the soft palate elevates in combination with the lateral and posterior pharyngeal walls forming a closed seal between the oral and nasal cavity. Thus for deglutition, the anterior two thirds of the tongue is critical at the initial phase of deglutition, while the posterior one third plays an important role in generating negative pressure to push the bolus of food down the alimentary canal [5].
In the subsequent pharyngeal stage, as the bolus moves inferiorly from the base of the tongue, continual palatopharyngeal closure prevents food from the entering the nasopharynx. Next, elevation of the larynx towards the base of the tongue is accomplished by the suprahyoid musculature. This is followed by closure of the larynx by inferoposterior rotation of the epiglottis. This is a laryngopharyngeal protective mechanism to prevent aspiration during swallowing. A finite period of apnea must necessarily take place with each swallow. Relating deglutition to respiration, deglutition most often occurs during expiration and includes a period of apnea ranging from 0.3- 2.5 seconds [4].
The tongue is the major component modulating air to create speech. The tongue shapes the oral and pharyngeal cavity for vowel production. It also restricts air flow to produce consonants such as k,g,t,d,s and z [3].
Tongue Size
Classification according to House [6]
Class 1: Normal in size, development, and function. Sufficient teeth are present to maintain normal form and function.
Class 2: Teeth have been absent long enough to permit a change in the form and function of the tongue.
Class 3: Excessively large tongue, all teeth have been absent for an extended period of time, allowing for abnormal development of the size of the tongue. Improper denture contour sometimes can lead to development of a class 3 tongue.
Tongue Position
Classification according to Wright [6]
Normal: The tongue fills the floor of the mouth and is confined within the mandibular teeth. The lateral borders rest on the occlusal surfaces of the posterior teeth and the apex rests on the incisal edges of the anterior teeth.
Class 1: Retracted: The tongue is retracted. The floor of the mouth is pulled downward and is exposed back to the molar area. The lateral borders are raised above the occlusal plane and the apex is pulled down into the floor of the mouth.
Class 2: Retracted: The tongue is very tense and pulled backward and upward. The apex is pulled back into the body of the tongue and it almost disappears. The lateral borders rest above the mandibular occlusal plane. The floor of the mouth is raised and tense.
Class 3: When tongue is low in relation to mandibular ridge crest or retarded in relation to anterior ridge, retention of the mandibular denture will be poor.
Investigation
Articulatory function after glossectomy has been evaluated by means of dynamic palatography. The dynamic palatograph is an electronic apparatus that generate a visual display of constantly changing linguo-palatal sounds as a function of time using an artificial palatal plate with affixed electrodes. Palatography can examine whether tongue contacts the palate or not at measuring point [7]. The glossal sounds which are one of the misheard sounds in glossectomy patients categorised into three types by type of articulation, stop plosive, affricate and fricative. These sounds cannot be evaluated by observing simply whether not the tongue contacts the palate. Therefore, to assist with the rehabilitation of glossectomy patients, it is necessary to evaluate objectively the degree of linguo-palatal contact [8].
Wax trial and patient’s speech was assessed with the help of Dr. Speech Software Version 4 (Tiger DRS, Inc., Seattle). This software allows the user to record, analyze and display the acoustic signals. The programme will automatically compute statistical information and plot a voice profile from sustained vowel and continuous speech. This is an objective, non-invasive method to evaluate acoustic signals [9].
Defect Classification with Treatment Option
Tongue (glossal) defects can be classified into partial or total. Factors influencing the prognosis of restoring the tongue with prosthesis depend upon the presence or absence of teeth and the type of procedure that is combined with the glossectomy (e.g., mandibulectomy, palatectomy, radiation therapy). Patients with partial glossectomy (i.e., < 50% of tongue removed) suffer minimal functional impairment and require no prosthesis. Removal of more than 50% of the tongue requires rehabilitation with either palatal or lingual augmentation prosthesis. Total glossectomy create a large oral cavity, loss of speech, and pooling of saliva and liquid. Patients with a total glossectomy require a total glossal prosthesis. In dentulous patients, the glossal prosthesis can be attached to the mandibular teeth through a lower partial denture [2].
On reviewing the literature, the following various clinical scenarios were identified and treated with different types of tongue prosthesis.
1. Completely edentulous with total glossectomy [10]
Treatment: Mandibular denture lingual flange extending over the floor of the mouth with a mushroom shaped button attached to it on which, the silicon tongue can be placed [Table/Fig-1]. After a total glossectomy the floor of the mouth becomes concave. Two prosthetic tongues can be made, one for phonetics and the other for swallowing. The tongue made for phonetics is somewhat flat, with a slightly wide anterior elevation to aid in articulation of linguo-alveolar sounds ‘t’ and ‘d’ and to aid in shaping the oral cavity for improved vowel production. The tongue for swallowing is made with a trough in the posterior aspect to guide the food bolus entery into the oropharynx.
Tongue prosthesis for swallowing.

2. Completely edentulous with total glossectomy and hemi-mandibulectomy.
Treatment 1: Mandible is reconstructed with bone graft and rehabilitated with implant retained overdenture is made with tongue prosthesis [11]. [Table/Fig-2].
Tongue prosthesis for speech.

Treatment 2: Maxillary complete denture and mandibular complete denture with guiding flange which will close the defect [Table/Fig-3]. Loss of continuity of the mandible affects the balance of the lower face and leads to deviation of the residual segment toward the resected side to aid in shaping the oral cavity for improved vowel production. The tongue for swallowing is made with a trough in the posterior aspect to guide the food bolus into the oro-pharynx [10].

3. Partially edentulous with partial glossectomy involving anterior part of the tongue.
Treatment: Maxillary partial denture with palatal augmentation [12].
4. Dentulous patient with segmental resection of mandible and resection of lateral part of the tongue.
Treatment: Maxillary partial denture with palatal augmentation prosthesis and mandibular cast partial denture obturating the defect with a guiding flange [Table/Fig-3,4]. The guidance flange for the mandibular framework was designed to extend upto the non-defect side [13].
Partial denture with palatal augmentation prosthesis.

Types of tongue prosthesis based upon the function
A. Single piece tongue
Tongue prosthesis for swallowing.
Tongue prosthesis for speech.
In edentulous patients, tongue prosthesis can be retained to either a mandibular or maxillary denture. Common problems associated with tongue prosthesis include lack of salivary control and loss of ability to maneuver food from the buccal vestibule. Therefore, it is best to fabricate two prosthetic tongues, one for swallowing and 1 for speech [14].
A typical prosthetic tongue for speech is flat with wide anterior elevation, which aids in articulation of linguo-alveolar sounds (e.g., /t/, /d/). It also has a posterior elevation, which aids in production of posterior linguo- alveolar sounds (e.g., /k/, /g/) and helps to shape the oral cavity for improved vowel productions [14].
The tongue prosthesis made for swallowing had a trough in its posterior slope to guide the food bolus into the oropharynx. A speech pathologist and a dietitian should monitor the patients who have had a glossectomy [14] [Table/Fig-5].
Tip of the tongue prosthesis (silicone).
B. Two piece tongue
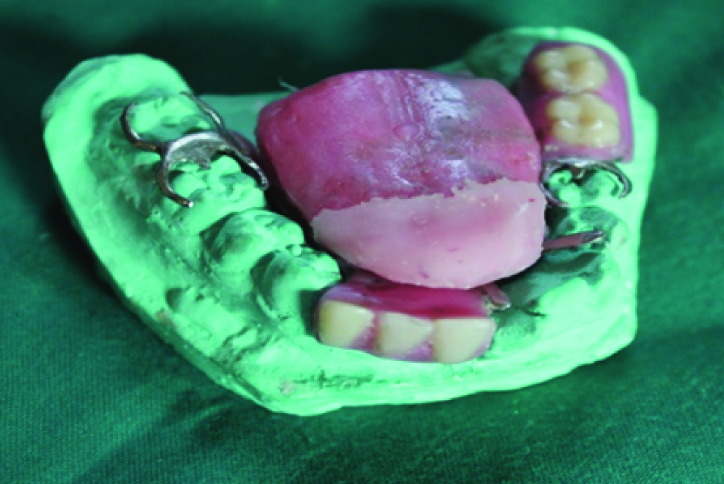
Impressions are made with alginate using a maxillary tray for mandibular arch in order to record the floor of the mouth properly. The base of the mandibular denture extends over the floor of the mouth. A “mushroom like” button is made on the mandibular prosthesis so that a silicone tongue can be placed over it [10] [Table/Fig-6,7].


C. Prosthesis Attached to Maxillary Denture-Palatal Augmentation Prosthesis
The Palatal Augmentation Prosthesis (PAP) has been defined by the Glossary of Prosthodontic Terms as a palatal prosthesis that allows reshaping of the hard palate to improve tongue/palate contact during speech and swallowing because of impaired tongue mobility as a result of surgery, trauma, or neurologic/motor deficits [15]. The palatal augmentation prosthesis is used to restore impaired speech and swallowing in glossectomy [Table/Fig-8] patients by artificially lowering the palatal vault to provide contact between the remaining tongue and the palatal contours [15]. The function of the residual tongue is recorded with softened modeling compound. The patient is asked to repeat the linguo-velar sounds and the linguo-alveolar. The compound gets moulded accordingly and then the denture is processed. Modification if acceptable speech articulation is attained for most elements of speech except the linguo-alveolar fricatives ‘s’ and ‘t’, for which another modification can be done. A narrow, sharp groove carved in the midline of the palatal prosthesis can, by directing the air stream, improve the production of these sounds [16].
Maxillary denture with palatal augmentation prosthesis;

Wax up for the tongue prosthesis was done on the auto-polymerized acrylic resin record bases, which was done like the shape of a tongue that conforms to oral cavity dimensions with rounded edges [Table/Fig-9]. The tongue tip was arched downwards to approximately a 15-degree angle, and the entire pattern was then arched slightly to form the highest point at the anterior one third of the tongue. Wax pattern was then folded to form a wide central V-shaped angle (approximately 160 degrees). The thickness of the wax was reduced 4 to 5mm at the base and the posterior two thirds of the tongue.
Mandibular denture with wax pattern.

Materials Used for Tongue Prosthesis
Acrylic Resin
Polymethylmethacrylate (PMMA) resin is the material of choice in the past. It is easy to work with acrylic resin and it is, hygienic, durable and easily matches to skin colour. It has many advantages like, intrinsic and extrinsic colouration can be done easily with acrylic resin. Strength of this is material is high compared to silicone. Alterations can be easily done and compatible with most adhesive systems, heat PMMA preferred over the auto polymerizing PMMA (Presence of free toxic tertiary amines). The colour stability when exposed to UV light is better in heat polymerized resin. Also, it remains serviceable for up to two years. Surface colour applications can be easily done and lasts for longer periods. It has some disadvantages like rigidity, cannot be used in movable tissue beds which leads to local discomfort and exposure of margins and high thermal conductivity which may precipitate discomfort in cold climates. Duplication of the prostheses is not possible because removal of prosthesis is possible only after destruction of the mold [18].
Silicone
Long chain molecules composed of alternating chain of silicone and oxygen atoms. The extraordinary properties of silicones are due to the special characteristics of the silicon oxygen bonds in their backbone. Because the silicon oxygen bond is much stronger than the carbon-carbon bond of organic polymers, silicones make better electric insulators and are more resistant to oxidation. Two types of silicone are RTV and HTV (According to vulcanising temperature) [18].
RTV – Silicone (Silastic 382, Silastic 399)
They set by condensation polymerisation in which stannous octate is the catalyst; Ortho-alkyl Silicate is cross linking agent. The advantages are, allows intrinsic colouration, easy handling, quick processing, good thermal and colour stability and inert. The disadvantages are they have weak edge strength, zipper effect, poor tear strength, high specific gravity, stiff, poor wettability [19].
Silicone (MDX 4-4210)
Most commonly used material for maxillofacial prosthesis. It requires heat for vulcanization. It is highly viscous, white and opaque. It is available as one or two component in which platinum salts (for addition polymerisation) and Hydro-methylsiloxane for cross-linking. It requires advanced equipment for processing and it has better physical properties. It exhibits improved qualities relating to colouration and edge strength, not heavily filled, making it translucent, increased elongation and resistant to tear. Surface characterization can be achieved with pigments immersed in a silicon adhesive. Superior cosmetic results are achieved with this material. The advantages are excellent thermal stability, colour stablity with UV, superior strength, biologically inert, polychromatic and it has good tear strength. The disadvantages are low edge strength, poor wettability, low elasticity, require two roll milling machine for intrinsic colouring and metal molds for processing. Also, extrinsic colouring is difficult [20].
The material used to fabricate tongue prosthesis is silicone which. has several advantages. (i) single component, (ii) ready to use, (iii) eliminating mixing errors, (iv) easy processing, (v) can be polymerized simultaneously with acrylic, (vi) stands the influences of oral environment without deterioration, (vii) non-irritant (viii) odourless and tasteless [2].
Discussion
Tongue is the major articulator during the production of all phonemes except bilabial, labio-dentals and glottal sounds. Tongue movements modify the shape of the oral cavity and change the resonance characteristics that produce different consonants [2]. The coordination of the muscle and nerve is impaired in glossectomy patients even after reconstruction by flap [21].
When a patient undergoes a partial on total glossectomy, the ability to masticate, swallow and formulate vowels and consonants for speech sounds is dramatically altered. The size, location and extent of the defect affect the degree of disability to swallow or speak. The areas of surgical resection that affects function of the tongue include removal of the anterior tip of the tongue, lateral (partial) glossectomy, removal of the base of the tongue and total glossectomy [22]. Moore (1972) suggested that tongue prosthesis as the treatment of choice in total glossectomy. This approach seldom restores the function of speech and small; it is mostly cosmesis [23].
Artificial tongue prosthesis may be either hard or resilient acrylic which is attached to the lower denture base, which covers the alveolar ridge as well as floor of the mouth. The artificial tongue is designed such a way that the dorsum of the anterior two third of the tongue conforms to the anterior part of the palate and comes in contact with the palate when the teeth are brought into occlusion. The posterior one third of the tongue is designed to act as a funnel, Palatal augmentation (or drop) prosthesis is indicated when the tongue resection and reconstruction results in limited bulk and restricted movement of the reconstructed tongue. [22].
The palatal augmentation prosthesis allows reshaping of the hard and/or soft palate to improve tongue/palate contact during speech and swallowing. This could be a removable partial denture or complete denture prosthesis [22]. While rehabilitating a glossectomy patient, the oral functions of the residual structures must be assessed. In addition to the extent of the defect factors such as mobility of the residual oral and paraoral structures, neuromuscular co-ordination and motivation will also determine the prognosis of the treatment [24].
A patient may be able to compromise some dysfunction without prosthetic support, while desiring prosthetic treatment which will help to improve or correct other specific problems [25]. While fabricating denture for a glossectomy patient, the bucco-lingual table should be wide, height of the occlusal table to be matched to that of the tongue body, and a closely adhering tongue and lingual flange are effective means of preventing the food from dropping into the floor of the oral cavity, keeping the food on the occlusal table, and crushing the food [2].
The Space of Donders is essential for the successful function of the prostheses [26]. When constructed in a systematic manner with the assistance of the speech pathologist, the mandibular denture with tongue prosthesis can achieve the following [2,13]: (1) reduction in the size of the oral cavity, thereby improving resonance characteristics; (2) direction of food into the oesophagus with the aid of a trough carved into the prosthetic tongue; (3) protection of the underlying soft tissue; (4) development of a surface of the residual tongue coming into contact during speech and swallowing; (5) improvement in appearance, psycho-social adjustment and phonetics.
Conclusion
The prosthetic tongue may not replace the internal structure of the tongue, which is capable of infinite movements in swallowing and speech. The silicone tongue prosthesis does provide a certain degree of comfort and function.
[1]. Chen C, Zhang Z, Goa S, Jiang X, Speech after partial glossectomy. A comparison between reconstruction and non-reconstruction patientsJournal of oral maxilla-facial Surgery 2002 60:404-07. [Google Scholar]
[2]. Aramany MA, Downs JA, Beery QC, Aslan Y, Prosthodontic rehabilitation for glossectomy patientsJ Prosthet Dent 1982 48:78-81. [Google Scholar]
[3]. Beumer J III, Marunick MT, Curtis TA, Chapter 5:Acquired defects of the mandible: etiology, treatment, and rehabilitation. In Beumer J III, Marunick MT, Curtis TAMaxillofacial prosthetics: Prosthodontic and surgical considerations 1996 St. LouisIshiyaku America, Inc:174-83. [Google Scholar]
[4]. Selley W, Ellis R, Flask F, The synchronization of respiration and swallow sounds with videofluoroscopy during swallowingDysphagia 1994 9:162 [Google Scholar]
[5]. Blonsky E, Logemann J, Boshes H, Comparison of speech and swallowing function in patients with tremor disorders and in normal geriatric patients: A cinefluorographic studyJ Gerontro 1975 30:299 [Google Scholar]
[6]. Johnson PF, Taybos GM, Grisius RJ, Prosthodontics diagnostic, treatment planning and prognostic considerationsDCNA 1986 30:503-18. [Google Scholar]
[7]. Ohira A, Yosimusu H, Oyma T, Articulation functions in patients with glossectomy 2/3 or 4/5 combined reconstruction using myocutaneous flapJapan Journal of Logopedics and Phoniatrics 1985 26(3):215-23. [Google Scholar]
[8]. Yoshida A, A method of measurement for articulatory movement utilizing synchronus 16 mm high speed cinematography and palatography-2, Analysis of articulatory movement in glossectomized patientsJapan Journal of Oral Maxilla Facial Surgery 1987 33:923-36. [Google Scholar]
[9]. Gurmit KB, Dholam Kanchan P, Long term rehabilitation of a total glossectomy patientJ Indian Prosthodont Soc 2010 10:194-96. [Google Scholar]
[10]. Gupta G, Dhaded S, Shalini BN, Rehabilitation of glossectomy patient: ReviewIndian Journal of Basic and Applied Medical Research 2014 3:487-91. [Google Scholar]
[11]. Beumer J III, Curtis TA, Marunick MT, Maxillofacial rehabilitation: prosthodontic and surgical consideration 1996 St. LouisIshiyaku EuroAmerica:184-88. [Google Scholar]
[12]. Penn M, Grossmann Y, Shifman A, Taicher S, Implant retained feeding aid prosthesis for a patient following total glossectomy and laryngectomy: A clinical reportJ Prosthet Dent 2007 97:261-65. [Google Scholar]
[13]. Moni AK, Mohit S, Subramania Iyer. Recent advances and controversies in head and neck reconstructive surgeryIndian J Plast Surg 2007 40:3-12. [Google Scholar]
[14]. Pravin B, Priyanka S, Dholam KP, Gurmeet B, Technical considerations in rehabilitation of an edentulous total glossectomy patientInt Journal of Dentistry 2012 12:36-50. [Google Scholar]
[15]. The glossary of prosthodontic termsJ Prosthet Dent 1999 81:39-110. [Google Scholar]
[16]. Sxahin N, The fabrication of cast metal guidance flange prostheses for a patient with segmental mandibulectomy: a clinical reportJ Prosthet Dent 2005 93:217-20. [Google Scholar]
[17]. Izdebski K, Ross JC, Roberts WL, De Boie RG, An interim prosthesis for the glossectomy patientJournal of Prosthet Dent 1987 57(5):608-11. [Google Scholar]
[18]. Chalian VA, Drane JB, Maxillofacial prosthetics–multidisciplinary practice 1972 The William and Wilkins. Co [Google Scholar]
[19]. Singh L, Bharathi SS, Srivastava V, Chopra D, Parashar A, Anwar F, Maxillofacial materialsJournal of dental sciences & oral rehabilitation 2012 1:14-8. [Google Scholar]
[20]. Maller US, Karthik KS, Maller SV, Maxillofacial prostheric materials - past & present trendsJIADS 2010 1(2):25-30. [Google Scholar]
[21]. Cotert HS, Aras E, Mastication, degluition and speech considerations in prosthodontic rehabilition of total glossectomy patientsJournal of oral Rehabilition 1999 26(1):75-9. [Google Scholar]
[22]. Laaksonen JP, Lowen IJ, Wolfaardt J, Rieger J, Seikalay H, Harris J, Speech after tongue reconstruction and use of a palatal augmentation prosthesis. An acoustic case studyCanadian Journal of speech- language pathology and Audiology 2009 33(4):196-202. [Google Scholar]
[23]. Zaki HS, Prosthodontic rehabilitation following total and partial glossectomyIn: Clinical Maxillofacial Prosthetics. Taylor, T.D. EdQuintessence Publication Co:205-214. [Google Scholar]
[24]. Mantri S, Khan Z. Prosthodontic rehabilitation of acquired maxillofacial defects, head and neck Cancer, Dr. Mark Agulnik (Ed.), ISBN: 978-953-51-0236-6, InTech [Google Scholar]
[25]. Pigno MA, Funk JJ, Prosthetic management of a total glossectomy defect after free flap reconstruction in an edentulous patient: a clinical reportJournal of Prosthet Dent 2003 89:119-22. [Google Scholar]
[26]. Donders FC, Ueber den Mechanismus des Saugens. Pflugers Archiv furs dieGesamte Physiologie Des Menschen Und Der Tiere 1875 10:91 [Google Scholar]