Spinal Anaesthesia is Safe in a Patient with Wolff-Parkinson-White Syndrome Undergoing Evacuation of Molar Pregnancy
Pravalika Deviseti1, Vinayak S Pujari2
1 Post Graduate Student, Department of Anesthesiology, M.S. Ramaiah Medical College & Hospitals, New BEL Road Bangalore, India.
2 Associate Professor, Department of Anesthesiology, M.S. Ramaiah Medical College & Hospitals, New BEL Road Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pravalika Deviseti, Post Graduate Student, Department of Anesthesiology, M.S. Ramaiah Medical College & Hospitals, New BEL Road, Bangalore – 560054, India.
E-mail: dr.pravallika@gmail.com
Wolff-Parkinson-White (WPW) syndrome is an uncommon cardiac condition where there is an abnormal band of atrial tissue connecting atria and ventricles which can electrically bypass atrioventricular node. The anaesthetic management in these patients is challenging as life threatening complications can occur perioperatively like paroxysmal supraventricular tachycardia and atrial fibrillation. Also, regional anaesthetic technique like subarachnoid block is a safe and cost effective alternative to general anaesthesia as it avoids polypharmacy. We report the successful anaesthetic management of Wolff Parkinson White syndrome in a primi with hydatiform mole posted for suction and evacuation.
Accessory pathway, Subarachnoid block, Ventricular pre-excitation, WPW syndrome
Case Report
A 20-year-old primi with 13 weeks of molar gestation was planned for suction and evacuation. She was recently diagnosed as a case of WPW syndrome, when an electrocardiogram (ECG) was done incidentally at another hospital. But she was asymptomatic at the time of surgery with good exercise tolerance. On pre-anaesthetic evaluation there was no history of palpitations, syncope, dizziness or chest pain. She had no history of any other co-morbid illnesses. Patient was comfortable, her pulse rate was 74 beats/min, regular and blood pressure was 106/70 mmHg. The general and systemic examination was unremarkable. Laboratory tests including complete haemogram, renal function tests, serum electrolytes, coagulation profile and thyroid function were normal. ECG showed shortened PR interval of 0.08sec, slurred upstroke of QRS and T inversions in chest leads indicative of WPW pattern. Further evaluation with echocardiography showed normal cardiac function with ejection fraction of 60%. Cardiologist opinion was taken, as the patient was asymptomatic no treatment was started. Patient was explained spinal anaesthesia and consent was taken. In the operation theater standard monitors ECG, Non-Invasive Blood Pressure, pulse oximetry and temperature probe were applied. An 18G intravenous line was secured. Availability of anti-arrhythmic drugs and defibrillator was confirmed. Spinal anaesthesia was administered using 1.5 cc of 0.5% hyperbaric bupivacaine and 25 mcg of fentanyl. Level of sensory block achieved was T8. Oxygen was administered at 6 liters/minute through Hudson’s mask.
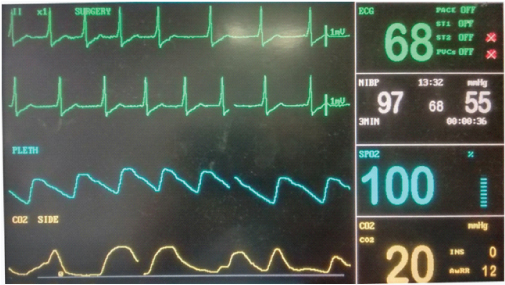
Haemodynamic parameters were stable throughout the surgery. Lead II was used for intra operative ECG monitoring which showed WPW pattern [Table/Fig-1]. Total duration of surgery was 1 hour. Intraoperatively patient received Midazolam 1 mg, Fentanyl 30 mcg intravenously and Oxytocin 20 units infusion. Total blood loss was 300 ml and one liter of crystalloid was infused. Postoperatively patient was transferred to high dependency unit for monitoring. She was comfortable, alert and vitals stable. Patient had uneventful recovery and was discharged after three days.
Discussion
The treatment for hydatiform mole is suction and evacuation during which blood loss may be substantial. Uterine relaxation may increase blood loss and inhaled anaesthetics are best to avoid in many of these patients. Spinal anaesthesia is preferred in haemodynamically stable patients because of its nontocolytic properties and the ease of using the technique [1].
Wolff-Parkinson-White (WPW) syndrome is a ventricular pre-excitation syndrome resulting from aberrant conduction pathway [2]. The incidence of WPW syndrome is 0.9–3% and the risk of sudden death due to a malignant arrhythmia is estimated at 0.4%/year in these patients [3]. The classical pre-excitation syndrome was first described by Wolff-Parkinson and White in 1930 [4]. Pre-excitation can be due to associated congenital heart diseases, mitral valve prolapse and cardiomyopathies. Diagnosis is done by the history of palpitations, dyspnoea, anxiety, angina pain, fatigue and characteristic ECG changes. Two major electro physiological(EP) criteria having an increased risk of sudden death are, shortest PR interval <250 milliseconds and ante grade effective refractory period of the accessory pathway <270 milliseconds [5]. Asymptomatic patients with WPW syndrome usually require no treatment and they have low incidence of developing paroxysmal supraventricular tachycardia (PSVT) during surgery [6].
In a small percentage of cases WPW syndrome may cause major complications. Paroxysmal atrial fibrillation (PAF) develops in up to one-third of patients with the WPW syndrome [7]. The reason for this high incidence of PAF in the WPW syndrome is not known. When PAF appears in patients with WPW syndrome who have anterograde conduction via the accessory pathway, it may be life threatening if an extremely rapid ventricular response develops degenerating into ventricular fibrillation [7]. The two pathways in WPW syndrome may be differently affected by drugs, changes in EP milieu and autonomic tone during anaesthesia.
The aim of anaesthetic management should be avoidance of sympathetic stimulation such as pain, anxiety, stress response to intubation and hypovolaemia [5,8]. Anaesthetic drugs and techniques tend to change the electrophysiology of the atrioventricular (AV) conduction system. If general anaesthesia is used it is important to avoid sympathetic stimulation. Fentanyl, midazolam, thiopentone, Isoflurane and Sevoflurane has been found to have no effect on the accessory pathway. Propofol is preferred, as it has no effect on the refractory period of accessory pathway [3]. There are reports of reversion to sinus rhythm following propofol injection. Cholinergic agents such as reversal agents and succinylcholine can accentuate the accessory pathway propagating arrhythmias [3]. Regional anaesthesia is preferred technique over general anaesthesia to avoid multidrug administration [5].
Recent literature suggested that the use of regional anaesthetic techniques to avoid sympathetic stimulation would be beneficial in WPW patients [5,8]. There are few cases reported under spinal anaesthesia alone for WPW syndrome. Most of the reports of subarachnoid block have used a very low dose bupivacaine supplemented with opioids. Addition of opioid provides rapid onset of block with reduced risk of hypotension. Blockade of cardio accelerator fibers and suppression of normal AV conduction might occur in high subarachnoid block. Also, high subarachnoid block causes relative excitement of parasympathetic nerves and thus facilitating conduction through accessory pathway [9]. Hence the dosage of the drug to be given for subarachnoid block should be titrated cautiously to achieve minimum level required for the surgery [9].
Phenylephrine is effective in treatment of hypotension without causing increase in heart rate, may be a good choice in patients with WPW syndrome. Fluid preloading aids to prevent reduction in atrial filling that occurs during regional anaesthesia which may increase the arrhythmogenecity. This also helps to reduce sympathomimetic requirements which may trigger SVT [6].
Treatment of WPW syndrome is radio frequency ablation of the accessory pathway and anti-arrhythmic drugs. If dysrrhythmias develop under anaesthesia, it is important to exclude the common causes (blood gas abnormalities, electrolyte disturbances, depth of anaesthesia) before attributing them to WPW syndrome. If PSVT occurs it can be treated initially with vagal maneuvers, lignocaine, adenosine or beta blockers. If this is ineffective then procainamide can be used. Patients developing Atrial Fibrillation with haemodynamic stability should be treated pharmacologically, where as haemodynamically unstable patients should be treated with cardioversion. Digitalis and verapamil are contraindicated as they increase conduction through accessory pathway [6].
Conclusion
A patient with WPW syndrome can be managed successfully under spinal anaesthesia provided the block level is cautiously monitored. Also, thorough understanding of pathophysiology of WPW syndrome, intensive preoperative evaluation and meticulous intraoperative monitoring is essential.
[1]. Solak M, Akturk G, Spinal anaesthesia in a patient with hyperthyroidism due to hydatidiform moleAnaesth Analg 1993 77(4):851-52. [Google Scholar]
[2]. Wolff L, Parkinson J, White PD, Bundle branch block with short P-R interval in healthy young people prone to paroxysmal tachycardia. 1930Ann Noninvasive Electrocardiol 2006 11:340-53. [Google Scholar]
[3]. Scheinman MM, The History of the Wolff–Parkinson–White SyndromeRMMJ 2012 3(3):e0019doi:10.5041/RMMJ.10083 [Google Scholar]
[4]. Bengali R, Wellens HJ, Jiang Y, Perioperative Management Of The Wolff-Parkinson-White SyndromeJ Cardiothorac Vasc Anaesth 2014 28(5):1375-86.http://dx.doi.org/10.1053/j.jvca.2014.02.003 [Google Scholar]
[5]. Kaur S, Gupta P, Aggarwal S, Anaesthetic management of Wolff-Parkinson-White syndrome for elective caesarean sectionInt J Pharm Pharm Sci 2012 4:755-56. [Google Scholar]
[6]. Shora A, Gurkoo S, Farooqi A, Qazi M, W Nisa W, Anaesthetic management of Wolff Parkinson White syndrome for caesarean sectionThe Internet Journal of Anaesthesiology 2007 (16):2 [Google Scholar]
[7]. Centurión OA, Shimizu A, Isomoto S, Konoe A, Mechanisms for the genesis of paroxysmal atrial fibrillation in the Wolff—Parkinson—White syndrome: intrinsic atrial muscle vulnerability vs. electrophysiological properties of the accessory pathwayEuropace 2008 10(3):294-302.DOI: 10.1093/europace/eun031 [Google Scholar]
[8]. Sahu S, Karna ST, Karna A, Lata I, Kapoor D, Anaesthetic management of Wolff-Parkinson-White syndrome for hysterectomyIndian J Anaesth 2011 55:378-80. [Google Scholar]
[9]. Garg R, Sinha R, Nishad PK, Patient with Wolff-Parkinson-White syndrome with intermittent pre-excitation under subarachnoid block for urological surgeryIndian J Anaesth 2011 55:167-70. [Google Scholar]