Calcaneum or heel bone fractures are the commonest fractures of the tarsal bones [1]. They result primarily due to high energy trauma and axial loading to the foot [2].
The incidence of calcaneal fracture is 11.5 per 100,000 population annually. It occurs 2.4 times more frequently in males. In males, the age of incidence is noted to range between 20-29 years [1].
The appropriate standard operative treatment for calcaneal fractures is a controversy. Several studies in the past have encouraged open reduction and internal fixation as the standard protocol. But, there have been several complications associated with it [3–6].
The main aim of this study was to assess the outcome of ankle function, restoration of radiological parameters in terms of Gissane’s and Bohler’s angle and complications.
Materials and Methods
A prospective study was conducted in the orthopaedics department of Justice K.S. Hegde Charitable Hospital from October 2012 and September 2014. A total of 23 patients who presented to us with tongue type intra-articular calcaneal fractures (as per the Essex-Lopresti classification) were included in the study [Table/Fig-1]. Patients with joint depression type fractures, open fractures, pathological fractures, skeletally immature patients and other associated fractures of the ankle were excluded from the study. The preoperative protocol involved complete clinical and radiographic evaluation. They underwent definitive surgical fixation at a later date when the skin and soft tissue conditions improved, after a period of immobilization and conservative management. People with good skin conditions were taken up for surgery on the day of presentation. Preoperative Gissane and Bohler’s angles were measured.
Preoperative radiographs lateral and axial views of left calcaneum showing tongue type intra-articular fracture of calcaneum

Preoperatively, all patients received intravenous injection of ceftriaxone 1g, 30 minutes before the incision.
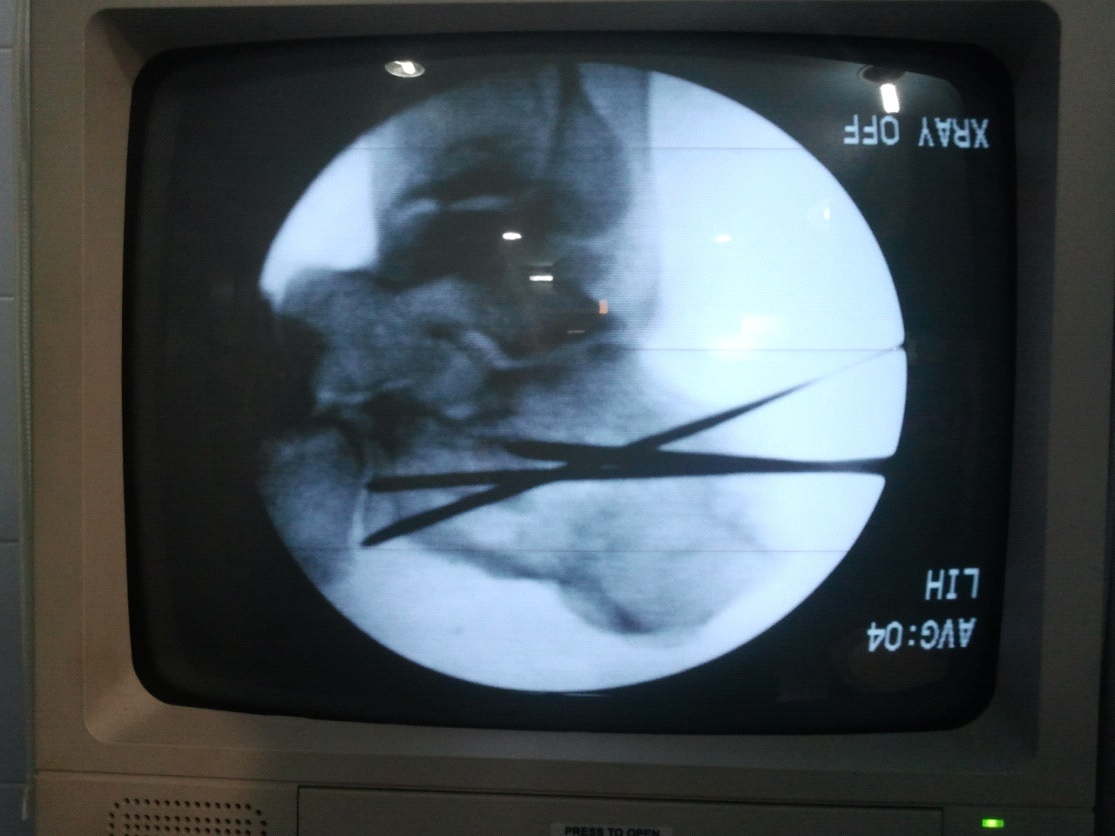
Under spinal anaesthesia, the patients were position in prone position on the split- legs operative table. Step one of the procedure was insertion of a Steinmann pin (3mm) into the fractured tongue fragment (superolateral to the Achilles tendon) for manipulating and restoring the posterior facet [Table/Fig-2]. Manual traction and compression force was applied throughout the surgery to restore the calcaneal alignment was done with tentaculum type bone holding forceps [7].
A 3 mm Steinmann pin passed under fluoroscopic guidance in to the superolateral tongue fragment through the Achilles tendon to facilitate closed manipulation and restore the posterior facet. A guide wire was inserted parallel to the Steinmann pin through the tongue fragment stabilizing the superomedial fragment-left calcaneum

A guide pin was inserted parallel to the Steinmann pin, fixing the superomedial fragment, through the tongue fragment and across the fracture site. Correct placement of the guide pins was confirmed under lateral and axial fluoroscopy [Table/Fig-3]. The second guide wire was inserted crossing the first guide wire in criss cross pattern [Table/Fig-3]. Drilling was done and 2 criss-cross 6.5 mm cannulated cancellous screws were inserted across the guide pins [Table/Fig-4]. Steinmann pin was removed. In patients with excessive heel widening, the primary fracture line was compressed with a bone clamp, and the fracture was fixed with one or two transverse screws subsequently [6].
Intraoperative fluoroscopic image showing, the second guide wire insertion was done crossing the first guide wire in a criss-cross pattern.
Intraoperative fluoroscopic image showing 6.5 mm cannulated cancellous screw insertion

Ten of the twenty three patients presented with excessive heel widening and underwent transverse screw fixation.
Post-operatively they received intravenous injection ceftriaxone 1 g till postoperative day three. Oral antibiotics (Tablet Cefixime 200mg twice daily) were continued for three more days postoperatively and then discontinued.
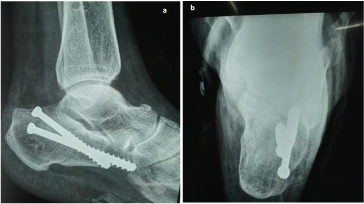
The postoperative protocol employed an immediate postoperative radiograph (lateral and axial views- [Table/Fig-5a&b]) and measurement of the Gissane and the Bohler’s angle. The patient was started on postoperative ankle mobilization on postoperative day three. Non-weight bearing axillary crutch mobilization was also started on postoperative day three. The reviews were timed at six weeks, 12 weeks and 24 weeks. Range of motion of ankle was assessed on each review. Partial weight bearing mobilization was begun at six weeks, full weight bearing at 12 weeks. Radiographs were taken during all the review periods and status of fracture union was assessed. At 24 weeks the final review was made and ankle function was scored as per the Maryland foot scoring system. The complications were documented.
A postoperative radiographs showing lateral and axial view showing the criss cross insertion of the screws with restoration of gissane and bohler’s angle.
Results
Of the 23 patients, seven patients were between the age of 50-59, seven between 40-49, seven under 30-39. Two patients were between 20-29. Out of 23 patients, 22 were males and one patient was female.
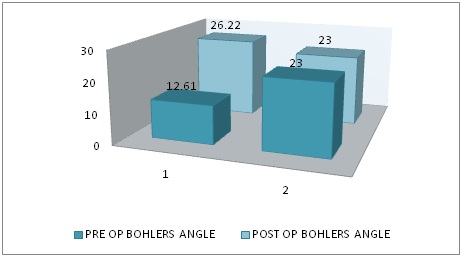
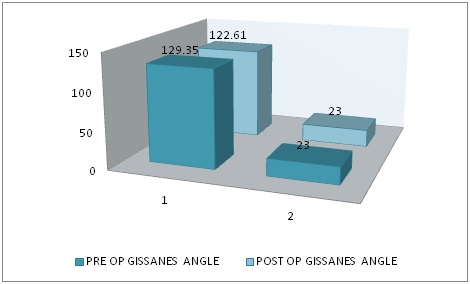
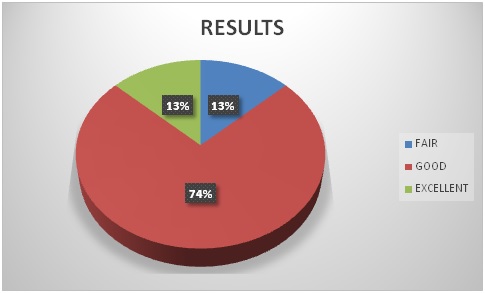
All the operated patients had an increase in the Bohler’s angle and decrease in the Gissane’s angle with a statistically significant p-value. The mean pre op Bohler’s angle was 12.61° and Gissane’s angle was 129.35°. The mean Postoperative Bohler’s angle was 26.22° and Gissane’s angle was 122.61° [Table/Fig-6,7]. The inference of the Maryland foot score concluded that 13% of the patients had excellent results. A 74% had good results and 13% had fair results [Table/Fig-8].
Graph showing preoperative and postoperative comparison of the Bohler’s angle. The mean preoperative Bohler’s angle was 12.61° the mean Postoperative Bohler’s angle was 26.22°. Note the significant increase in Bohler’s angle.
Graph showing preoperative and postoperative comparison of Gissane’s angle. The mean preoperative Gissane’s angle was 129.35°. The mean Postoperative Gissane’s angle was 122.61°. There is significant drop in Gissane’s angle.
Pie diagram showing the inferences as per the Maryland foot score. Three patients had excellent scores, three had fair and 17 patients had good scores
Of the 23 patients, one patient had subtalar arthritis as a complication. All fractures united radiologically by 12 weeks. None of the patients developed infection, malunion or non-union.
Discussion
Fractures of the calcaneum make up about 2% of all fractures and form the commonest of the tarsal bone fractures [1]. The extra-articular fractures have a uniformly good prognosis, but that for an intra-articular fracture is varied. The management of every aspect of an intra-articular calcaneal fracture is controversial. Although studies which have cited 31-61 fractures have demonstrated good results for open reduction and internal fixation of intraarticular calcaneal fractures [6,8], the most appropriate choice of treatment still is controversial [3,9,10]. However, Buckley et al., found better results in some subgroups of patients after surgery [11].
It was noted in our study that patient distribution was equal under the age groups of 30-39, 40-49 & 50-59 years and the least no. of patients were between 20-29 years. Nambiar noted that 56% of his patients were in the 3rd to 4th decade of life [12]. Buckley noted that in his study the maximum age incidence was between 30-39 years (60%) with age range between 15-68 years [11].
The commonly used classification systems for calcaneal fractures are Essex-lopressti, Rowe and Sanders classification. However, none of these classification systems show any correlation with choice of treatment [13–15].
Essex Lopresti Classification [
13–
15].
A) Extra-articular fractures
1) Fractures of anterior process
2) Fractures of tuberosity
3) Fractures of medial calcaneal process
4) Fractures of sustentaculum tali
5) Fractures of body not involving the subtalar joint
B) Intra-Articular Fractures
1) Non-Displaced
2) Tongue Type
3) Joint Depression Type
4) Comminuted
Two important angles are primarily calculated which indicate the anatomy as seen on lateral radiographs:
The first is Böhler’s angle; this angle is formed by a line drawn from the superior aspect of the anterior process to the superior aspect of the posterior facet and a second line drawn from the superior aspect of the posterior facet tangential to the superior edge of the tuberosity. A normal Böhler’s angle is approximately 25° to 40°. Values below the normal values signify an intraarticular fracture also loss of sagittal bony alignment and calcaneal height [16].
The second is the critical angle of Gissane which is formed by the intersection of the two lines along the downslope of the posterior facet and the upslope of the anterior process [16].
In our study, the results inferred near normal restoration of Gissane’s and Bohler’s angle in all the cases, these results are comparable to the study by Yeung Yip et al., who inferred the same in most of their patients [7].
Applying the Maryland foot score in our study 74% had good scores and 13% had excellent results. Yeung Yip et al., inferred 36% good and 52% excellent results [7].
In our series, the use of percutaneous technique of screw fixation decreased the incidence of scar formation, residual stiffness and there was improved clinical and cosmetic results. Wound complications of wound dehiscence and flap necrosis were minimised when compared with open reduction and internal fixation. Early mobilisation and avoidance of prolonged bracing were reduced after fixation by screws. Operation time, hospital stay and time required for return to normal life were reduced.
Schepers et al., conducted a study on ‘Percutaneous treatment of displaced intra-articular fractures of calcaneum’ and concluded that percutaneous technique had a better prognosis as compared to the open technique despite similar levels of complication rate. Total scores of subtalar motion was good as compared to the open technique [17].
El khalifa et al., conducted a study from January 2006 to May 2009 on Limited open reduction and percutaneous screw fixation of displaced intra articular fracture of calcaneus and concluded that operable cases of displaced intra-articular fracture of calcaneum, mild to moderate comminution were treated adequately and effectively using percutaneous screw fixation. Percutaneous screw fixation of the displaced intra-articular fracture of the calcaneum is an effective, safe, and reproducible method of treatment [18].
Conclusion
Percutaneous screw fixation of tongue type calcaneal fractures is a very effective surgical technique with good functional and radiological outcome and minimal complication rate.