Non-Hodgkins lymphoma of the Natural Killer (NK) cell type is rare. World Health Organisation recognises 3 NK-cell phenotypic entities; extranodal NK/T cell lymphoma, nasal type (ENK/TL); aggressive NK cell leukaemia (ANKL); and chronic lymphoproliferative disorders of NK cells (CLPD-NK) which is classified as a provisional entity. Though specific clinical, morphological and immunophenotypic criteria have been laid down to diagnose these conditions there may however, be considerable variations in the clinical presentation making diagnosis difficult. We present a case with contrasting clinical and haematopathological findings posing difficulty in its diagnosis and classification, and despite the aggressive presentation showing favourable response to treatment.
Flow cytometry, NK-cell, Non-Hodgkins lymphoma
Case Report
A 30-year-old man was admitted with 1 month history of fever, weakness, lethargy, non quantifiable weight loss and cervical lymphadenopathy in a private hospital. The patient was diagnosed with diffuse large B-cell lymphoma on fine needle aspiration and was started on CHOP regimen. However, following two cycles of chemotherapy, no response was seen and he was referred to our institute. Details pertaining to diagnosis and immunophenotyping were not available with the patient on initial presentation.
The patient on arrival was febrile, pulse 90/min, BP 110/70 mm Hg. On examination bilateral cervical, axillary and inguinal lymph nodes were noted along with hepatosplenomegaly. There was also diffuse midline swelling consistent with enlargement of thyroid gland. Examination of the nasal cavity was unremarkable. On investigation, he was mildly anaemic (haemoglobin 10.8 g/dl), total bilirubin 0.7 mg/dl, ALT 27 U/L, AST 22 U/L, blood urea nitrogen 24 mg/dl and serum creatinine 0.5 mg/dl. Serum electrolytes were normal and serum LDH was raised. Peripheral blood examination showed normocytic normochromic anaemia and no atypical cell was noted.
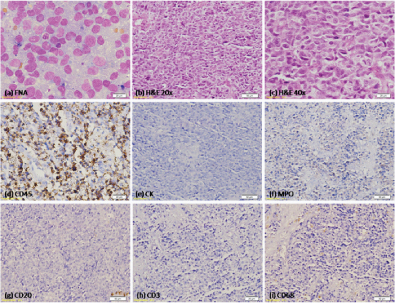
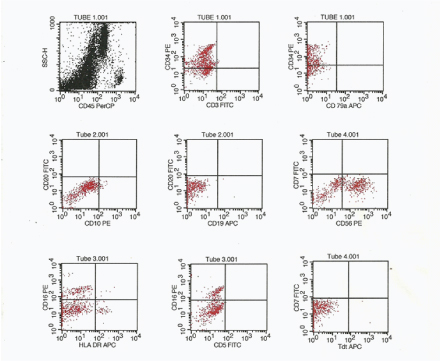
On imaging, multiple abdominal and mediastinal lymph nodes were noted, along with multiple foci of hepatic involvement. Fine needle aspiration (FNA) performed at the private hospital, from the cervical lymph node; thyroid and liver were retrieved and reviewed. All showed highly cellular smear with sheets of medium to large cells consistent with the diagnosis of non-Hodgkins lymphoma [Table/Fig-1a]. Flow cytometry (FCM) was performed using FACSCalibur (Becton Dickinson, San Jose, CA, USA) on a fresh cervical lymph node aspirate. Cells were gated on SSC/CD45 dot plot. The gated population showed strong positivity for CD56, CD16 with dimCD34, but were negative for sCD3, CD5, CD19, CD20, CD79a, CD10, CD13, CD33, CD117, MPO, HLA-DR, Tdt [Table/Fig-2]. Cervical lymph node biopsy was done which showed totally effaced lymph node, replaced by sheets of large cells with coarse chromatin, prominent nucleoli and scant cytoplasm. Areas of fibrosis were also seen [Table/Fig-1b&c]. On immunohistochemistry (IHC), these cells were CD45 positive and negative for pan-cytokeratin [Table/Fig-1d&e]. IHC further confirmed the FCM findings with negativity for MPO, CD20, CD3, CD68 [Table/Fig-1f-i], CD30 and CD117. CD34 was positive on FCM but was found to be negative by IHC. In-situ hybridisation was performed for Epstein-Barr virus encoded RNA and was found to be negative. Bone marrow aspiration was performed for staging and it showed lymphoma cell infiltration. Peripheral blood smear however failed to reveal any such cell.
FNA from thyroid showing monotonous population of large lymphoma cells. (MGG; 400X); (b,c) cervical lymph node showing lymphoma cells (H&E; 200X & 400X); (d) immunohistochemistry showing CD45 positivity; (e-i) rest of the markers were negative. (IHC; 200X).
Flow cytometry performed on the cervical lymph node aspirate. Lymphoma cell showed moderate CD45 positivity. Bright CD56 positivity was seen in majority of the gated cells. Bright CD16 and heterogeneous CD34 positivity was also noted in minor component of gated population
Based on the clinical presentation and the investigation, a diagnosis of non-Hodgkins lymphoma of NK-cell phenotype, Ann-Arbor stage IVB was made. However, we were not able to subclassify our case into any of the NK-cell lymphoma entity described in the 2008 WHO classification. The patient was started on VIPD chemotherapy regimen. Ifosfamide at 1200mg/m2/day as a slow infusion over 3 hours with mesna injection at 0, 4 and 8 hours, etoposide at 100 mg/m2/day and cisplatin at 30 mg/m2/day over 2 hours were given for 3 days. Intravenous dexamethasone, 40 mg was given on day 1 to 4. He has received 3 cycles of chemotherapy. All the cycles were uneventful and presently, as assessed by the revised response evaluation criteria in solid tumour (RECIST) guidelines [1], the patient is under partial remission and regular follow up.
Discussion
Lymphoma of the NK cell phenotype is rare. International T-cell lymphoma project reports that 10.4% of T cell lymphomas are of NK/T cell type (NK/TCL). WHO recognized entities include extranodal NK/T cell lymphoma, nasal type (ENK/TL), which is predominantly nasal or may rarely be extranasal; aggressive NK cell leukaemia (ANKL) and chronic lymphoproliferative disorders of NK cells (CLPD-NK). These disorders are uncommon and are seen in Asians, Central and South Americans, and Mexicans. Among these entities, CLPD-NK is indolent but the other two follows an aggressive course with variable prognosis and short survival [2–4]. The 5 year overall survival for NK/TCL is 32% and this drops down to 9% for extranasal, aggressive and unclassifiable NK cell lymphoma [5]. Diagnosis of NK cell lymphoma can be challenging. Unlike T-cell lymphomas, NK-cell lymphoma fails to show receptor gene rearrangement. So, immunophenotyping of the NK-lymphoma cells play a critical role in disease characterisation [6].
ENK/TL shows an Asian and South American predilection, occurs exclusively in extranodal fashion involving nasal and upper aerodigestive tract with rare advanced cases showing disseminated lymphadenopathy, hepatomegaly or leukaemic phase. Rarely, exclusive extranasal site like skin, salivary glands, testis, and gastrointestinal tract may be involved. They present mostly in stage I/II, with the extranasal cases being more aggressive, presenting at stage III/IV. They are associated with Epstein-Barr virus (EBV), and quantification of EBV DNA helps to assess tumour load, and disease prognosis. Morphologically, it exhibits ulceration, geographic necrosis with angiocentricity and angiodestruction and these cells shows cytoplasmic CD3 and CD56 positivity [2,7].
ANKL are aggressive involving peripheral blood (PB), bone marrow (BM), spleen, liver, presenting with fever, jaundice with variable cytopaenia, leukaemic blood picture, sometimes associated with haemophagocytosis and generally progresses to multiorgan failure. They are associated with EBV. It occurs at a younger median age than ENK/TL or CLPD-NK, with frequent BM involvement and rare cutaneous involvement. These features are contrary to the suggestion that ANKL are merely the leukaemic phase of ENK/TL [3,8]. The disease is aggressive, not responsive to conventional chemotherapy with median survival of 2 months [9].
CLPD-NK is rare and indolent. Most patients are asymptomatic or show variable cytopaenias. PB and BM are the predominantly involved sites, with hepatosplenomegaly, lymphadenopathy and cutaneous involvement being infrequent. They may occur in association with other medical conditions, and rarely may transform to aggressive forms [4,10].
The present case had a unique presentation of a young patient, in a disseminated state of nodal and multiple extranodal site involvement, without evidence of nasal or PB disease. Immunophenotype was consistent with NK cell but based on the clinical presentation, we were unable to place the case in any of the WHO described entities. The survival rate according to literature for such aggressive clinical presentation usually does not exceed 2 months. Despite the aggressive presentation, the patient responded to the prescribed chemotherapy regimen. After six months of diagnosis and 3 cycles of chemotherapy, the patient significantly improved with disappearance of all the peripherally palpable target lesions, including lymph nodes and thyroid. Presently, the abdominal lymph nodes and hepatic lesion show partial remission.
Conclusion
We wish to highlight that a revision including wider clinical presentations, with specific diagnostic markers maybe necessary to increase the diagnostic accuracy and reproducibility for such cases, as this might have profound impact on their survival and disease prognostication.
[1]. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1)Eur J Cancer 2009 45:228-47. [Google Scholar]
[2]. Chan JKC, Quintanilfa-Martinez L, Ferry JA, Peh SC, Extranodal NK/T cell lymphoma, nasal type. In: Swedlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al, (eds)WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues 2008 LyonIARC:285-288. [Google Scholar]
[3]. Chan JKC, Jaffe ES, Ralfkiaer E, Ko YH, Aggressive NK cell leukaemia. In: Swedlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al, (eds)WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues 2008 LyonIARC:276-277. [Google Scholar]
[4]. Villamor N, Morice WG, Chan WC, Foucar K, Chronic lymphoproliferative disorder of NK cell. In: Swerdlow SH, Campo E, Harris NL, et al, (eds)WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues 2008 4th edLyon, FranceIARC:274-275. [Google Scholar]
[5]. Vose J, Armitage J, Weisenburger D, International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomesJ Clin Oncol 2008 26:4124-30. [Google Scholar]
[6]. Hasserjian RP, Harris NL, NK-cell lymphomas and leukaemias: a spectrum of tumours with variable manifestations and immunophenotypeAm J Clin Pathol 2007 127:860-68. [Google Scholar]
[7]. Tse E, Kwong YL, How I treat NK/T-cell lymphomasBlood 2013 121:4997-5005. [Google Scholar]
[8]. Lima M, Aggressive mature natural killer cell neoplasms: from epidemiology to diagnosisOrphanet Journal of Rare Diseases 2013 8:95 [Google Scholar]
[9]. Gogia A, Kakar A, Byotra SP, Bhargav M, Aggressive natural killer cell leukaemia: a rare and fatal disorderJ Assoc Physicians India 2010 58:702-04. [Google Scholar]
[10]. Morice WG, Jevremovic D, Olteanu H, Roden A, Nowakowski G, Kroft S, Chronic lymphoproliferative disorder of natural killer cells: a distinct entity with subtypes correlating with normal natural killer cell subsetsLeukaemia 2010 24:881-84. [Google Scholar]