Unraveling the Mystery Behind A Patient with ‘Refractory Seizures’
Mithun Jacob Varghese1, Anadaroop Lahiri2, Vipin Kumar3, Devi A Manuel4, Oommen K George5
1 Associate Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
2 Registrar, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
3 Assistant Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
4 Assistant Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
5 Professor, Department of Cardiology, Christian Medical College, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mithun Jacob Varghese, Associate Professor, Department of Cardiology, CMC, Vellore, Tamil Nadu-632004, India.
E-mail: drmithunjv@gmail.com
Neurological manifestations such as seizures although rare are well recognized presentations of cardiac arrhythmias. Almost always, such events are primarily generalized in nature leading on to loss of consciousness. Rarely however, cardiac seizures can manifest with focal neurological events. We report a case of a sexagenarian who presented with recurrent focal seizures with secondary generalization, who was misdiagnosed and treated as seizure disorder; only a careful history and focussed investigations helped in realising a precise diagnosis.
Focal seizure, Neurological manifestions, Postictal
Case Report
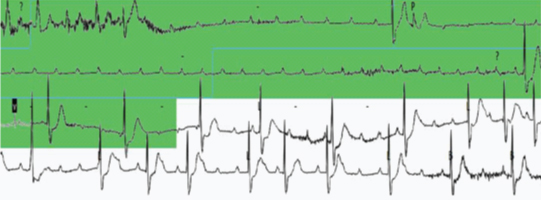
A 61-year-old man, with well-controlled Type 2 diabetes mellitus, presented with episodes of light-headedness followed by tonic clonic movements of the right upper limb and, later, of his entire body consistent with secondary seizure generalization. Each event culminated with rapid recovery of symptoms and minimal postictal confusion. In the three months since the commencement of these symptoms, he had suffered at least fifteen to twenty incidents of similar nature. He had undergone neurological evaluation elsewhere for the aforementioned complaints with investigative modalities such as electroencephalogram (EEG) and magnetic resonance imaging (MRI) of the brain, all of which failed to demonstrate any definite aetiology. In view of multiple ongoing episodes, he had been initiated on various antiepileptic drugs (sodium valproate, levetiracetam, clobazam), in spite of which these events persisted. He was presently admitted for evaluation of refractory seizures. His physical examination revealed a regular pulse rate and a normal blood pressure with no orthostatic hypotension. His baseline electrocardiogram (ECG) showed a left bundle branch block (LBBB) with a QRS axis deviation to the left and a normal PR interval. The abnormal ECG instigated a review of the chronology of symptoms, wherein the patient insisted on a very quick recovery after each episode. In view of the ECG abnormality, brief nature of the individual episodes and minimal post-ictal confusion, it was decided to observe him in the intensive care unit with continuous telemetric ECG and holter monitoring, as the likelihood of an arrhythmic syncope triggering the seizures was contemplated. Providentially, this period of observation comprised a similar event wherein the ECG [Table/Fig-1] revealed an episode of complete heart block (CHB) with a prolonged continuous episode of ventricular asystole lasting no less than twenty three seconds!
Image of an ECG which revealed an episode of complete heart block (CHB) with a prolonged continuous episode of ventricular asystole.
A diagnosis of intermittent CHB was arrived at, following which he underwent dual chamber permanent pacemaker implantation. His formerly scheduled MRI brain and EEG appointments were cancelled and antiepileptics were discontinued. He has not experienced any further episodes following the pacemaker implantation.
Discussion
Neurologic events as part of syncope are observed in up to 8% of cases [1], tonic clonic seizure like movements being the most frequent. Zaidi et al., studied 74 patients with ages ranging from 16 to 77 years, with treatment resistant epilepsy to look for possible cardiovascular causes of the seizures [2]. A total of 41.9% of these patients on re-evaluation were found to have alternative diagnoses. A history of partial seizures should not entirely eliminate the possibility of a syncopal episode, especially if the post-ictal confusion is unremarkable and the recovery is swift [3]. In such patients, an accurate history of the exact sequence of events [4] may prove invaluable in guiding appropriate diagnostic evaluation. It may not be easy to demonstrate paroxysmal complete heart block in patients with bundle branch blocks and it may be even more difficult to actually correlate a patient’s symptom with the development of high degree atrioventricular block. It is also noteworthy that LBBB with left axis deviation in the ECG generally denotes severe conduction system disease whereas right axis deviation indicates an associated myocardial pathology [5].
A similar case was reported by You et al., where a 62-year-old gentleman presented to the emergency department with generalised tonic seizures with rapid recovery of symptoms [6]. The ECG subsequently revealed paroxysmal CHB during one such episode. The episodes did not recur after the insertion of a temporary pacing wire. Another case was reported by Sidhu et al., with prolonged ventricular standstill and a similar presentation [7].
Typically patients with cardiac syncope may present with Stokes-Adams attacks. A Stokes-Adams attack is defined as sudden collapse into unconsciousness due to a disorder of heart rhythm in which there is a slow or absent heart rate resulting in syncope with or without convulsions. Stokes and Adams first described the disorder in the early 19th century (Stokes 1846 and Adams 1827). Hence eliciting a history of such attacks could be vital in considering an arrhythmia as the diagnosis, as opposed to seizures – and in many such cases, missing a diagnosis of a cardiac arrhythmia may have adverse consequences.
In our patient the prominence of the neurologic events misled clinicians into considering a primary neurologic cause for his symptoms with investigations targeted solely at the central nervous system. However, a detailed history uncovered the possibility of an arrhythmic disorder. Furthermore, a baseline ECG showing a LBBB with a left axis deviation reinforced this premonition. Finally, we were fortunate in that we succeeded in documenting the development of a high degree atrio-ventricular block both on telemetry and Holter and were able to temporally correlate the patient’s symptoms to the conduction abnormality.
The serendipitous discovery of paroxysmal CHB in our patient, especially at the time of symptoms, emphasises the importance of obtaining an electrocardiographic diagnosis correlating temporally with the symptoms. In order to achieve that it may be worthwhile to persevere with repeated ECGs in such patients where the diagnosis is suspect. Holter monitoring, telemetric monitoring and loop recorders [8–10] could be used liberally in such patients to tie up the electrocardiographic abnormality to the symptoms of the patient.
Conclusion
The evaluation of arrhythmic disorders is arduous in view of the often intermittent and irregular nature of these abnormalities. The yield in such situations, in terms of diagnostic capabilities, is consistently greater with an accurate and pertinent history along with a keen attention to the electrocardiogram in the hope of picking up an abnormality, rather than with progressively intensive and sophisticated investigations.
[1]. Passman R, Horvath G, Thomas J, Kruse J, Shah A, Goldberger J, Clinical spectrum and prevalence of neurologic events provoked by tilt table testingArch Intern Med 2003 163(16):1945-48. [Google Scholar]
[2]. Zaidi A, Clough P, Cooper P, Scheepers B, Fitzpatrick AP, Misdiagnosis of epilepsy: many seizure-like attacks have a cardiovascular causeJ Am Coll Cardiol 2000 36(1):181-84. [Google Scholar]
[3]. Sheldon R, Rose S, Ritchie D, Connolly SJ, Koshman M-L, Lee MA, Historical criteria that distinguish syncope from seizuresJ Am Coll Cardiol 2002 40(1):142-48. [Google Scholar]
[4]. Sheldon R, How to Differentiate Syncope from SeizureCardiol Clin 2015 33(3):377-85. [Google Scholar]
[5]. Bonow RO, Mann DL, Zipes DP, Libby P. Braunwald’s Heart Disease - A Textbook of Cardiovascular MedicineNinth edition:146146 p [Google Scholar]
[6]. You C-F, Chong C-F, Wang T-L, Hung T-Y, Chen C-C, Unrecognized paroxysmal ventricular standstill masquerading as epilepsy: a Stokes-Adams attackEpileptic Disord Int Epilepsy J Videotape 2007 9(2):179-81. [Google Scholar]
[7]. Sidhu M, Singh HP, Chopra AK, Kapila D, Sidhu S, Surviving ventricular standstill for 111 seconds during Holter monitoring. Ann Noninvasive Electrocardiol OffJ Int Soc Holter Noninvasive Electrocardiol Inc 2012 17(1):61-62. [Google Scholar]
[8]. Giada F, Bartoletti A, Value of Ambulatory Electrocardiographic Monitoring in SyncopeCardiol Clin 2015 33(3):361-66. [Google Scholar]
[9]. Paudel B, Paudel K, The diagnostic significance of the holter monitoring in the evaluation of palpitationJ Clin Diagn Res JCDR 2013 7(3):480-83. [Google Scholar]
[10]. Meyer C, Carvalho P, Brinkmeyer C, Kelm M, Couceiro R, Mühlsteff J, Wearable sensors in syncope managementMed Sci Monit Int Med J Exp Clin Res 2015 21:276-82. [Google Scholar]