Benign Lymphangioendothelioma - A Case Report
Naveen Kumar Vittal1, Sushruth Guruputra Kamoji2, Shilpa Vinay Dastikop3
1 Post Graduate Student, Department of Dermatology, Belagavi Institute of Medical Sciences, Belagavi, Karnataka, India.
2 Resident, Department of Dermatology, Belagavi Institute of Medical Sciences, Belagavi, Karnataka, India.
3 Associate Professor, Department of Dermatology, Belagavi Institute of Medical Sciences, Belagavi, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Naveen Kumar Vittal, Postgraduate Student, Doctor’s Quarters, Room No-305, BIMS, Belagavi, Karnataka-590005, India.
E-mail: webershetty@gmail.com
Benign lymphangioendothelioma is an uncommon locally infiltrative lymphatic tumour, presenting as a slow-growing, asymptomatic, reddish-violaceous macule or plaque. Histopathologically, it is characterized by thin-walled endothelial-lined spaces that are interspersed between strands of collagen. It must be recognized and differentiated from angiosarcoma, early Kaposi’s sarcoma, in view of major differences in treatment and prognosis. A 24-year-old female presented with a raised lesion over the left leg since 2 years which was associated with minimal itching. Biopsy of the lesion showed thin walled vascular channels lined by single layer of bland endothelial cells at the dermo-epidermal junction, few vessels in the dermis.
Acquired progressive lymphangioma, Endothelial-lined spaces, Lymphatic neoplasm
Case Report
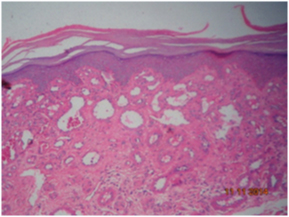
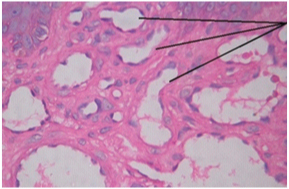
A 24-year-old female presented with raised lesion over the left leg since 2 years. It started as a dark spot and grew in size to attain the present size, associated with minimal itching. On application of topical steroids there was mild improvement and exacerbation on stopping the treatment. Hence, patient has used topical betamethasone for over 6 months as prescribed by the dermatologist. On examination, an ill defined hyperpigmented, atrophic plaque of 3x3cm in size, round to oval in shape noted over the anterior aspect of the leg below the left knee. Similar plaque was noted over the posterior aspect of left leg [Table/Fig-1,2]. Numerous stretch marks are noted around the primary lesion, most probably due to prolonged use of topical steroids. Biopsy was taken from the lesion over the anterior aspect of the leg below the left knee. The lesion was surgically excised. Histopathological examination showed hyperkeratosis is noted in the epidermis. Horizontal, thin walled vascular channels lined by single layer of bland endothelial cells are seen at the dermo-epidermal junction, few vessels are seen in the dermis [Table/Fig-3,4 and 5]. The patient is on follow up and there has been no recurrence.
Lesion on left leg, below the knee

Lesion on posterior aspect of left leg

Showing hyperkeratosis and thin walled vascular channels lined by single layer of endothelial cells in the dermis
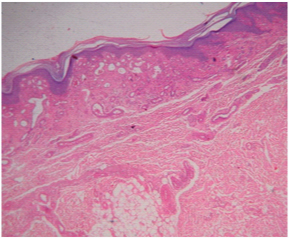
Showing hyperkeratosis and thin walled vascular channels lined by single layer of endothelial cells in the dermis (H&E,10X)
Showing the thin walled vascular channels lined by single layer of endothelial cells in the dermis. (H&E, 40x)
Discussion
Benign lymphangioendothelioma (BLAE) is a rare lymphatic neoplasm originally described by Wilson Jones et al., [1]. It was previously named as acquired progressive lymphangioma. It is postulated that benign lymphangioendothelioma may be a response to different inflammatory stimuli rather than a true neoplasm, because it has been described after different traumas, including surgery, radiation therapy, femoral arteriography, hip inflammation and tick bites [2–4]. Another pathogenic explanation could be a hormonal stimulus, because rapidly enlarging lesions have been described in many pubescent and prepubescent patients [5]. Finally, another hypothesis that has been suggested is that benign lymphangioendothelioma represents a complex vascular hamartoma with three components such as lymphatic vessels, blood vessels and smooth muscle [6].
Clinically, benign lymphangioendothelioma appears as an erythaematous to brownish plaque or as a slowly enlarging haematoma-like patch [1]. Men and women are equally affected [1]. The neoplasm is located mainly on legs, head and neck, even though there also are examples described in the wrist, shoulder, arm, forearm, breast, back, abdominal wall, buttocks, toes, soles and oral mucosa [2–6]. No haematologic or lymphatic dissemination has been yet described. A case report by Juan et al had similar presentation of the lesion over the trunk, but of larger size [7].
Histopathologically, benign lymphangioendothelioma is characterized by thin-walled endothelial-lined spaces that are interspersed between strands of collagen [1]. The endothelial cells stain positively for lymphatic markers such as podoplanin (D2-40), LYVE-1, and PROX-1. The cells are also variably positive for factor VIII, Ulex europaeus agglutinin I, CD31, and CD34 [2–4]. However, Tadaki et al., reported negative results for all these markers [5]. Benign lymphangioendothelioma should be histopathologically distinguished from Kaposi’s sarcoma, especially in patch stage, and from well-differentiated angiosarcoma [4]. Benign lymphangioendothelioma lacks the typical concomitant infiltration of the dermis with lymphocytes and plasma cells and there are usually no extravasated erythrocytes or haemosiderin deposition which is seen in Kaposi’s sarcoma [1]. Atypia and mitosis are the main features of angiosarcoma, with multi layering and endothelial-cell tufting in some areas [4]. For benign lymphangioendothelioma, complete surgical excision is the treatment of choice [1].
Conclusion
Benign lymphangioendothelioma (BLAE) is a very rare benign lesion that should be distinguished from well-differentiated angiosarcoma and Kaposi’s sarcoma, especially the patch stage, in view of major differences in treatment and prognosis.
[1]. Wilson Jones E, Winkelmann RK, Zachary CB, Reda AM, Benign lymphangioendotheliomaJ Am Acad Dermatol 1990 23:22 [Google Scholar]
[2]. Guillou L, Fletcher CD, Benign lymphangioendothelioma (acquired progressive lymphangioma) : a lesion not to be confused with well-differentiated angiosarcoma and patch stage Kaposi’s sarcoma: clinicopathologic analysis of a seriesAm J Surg Pathol 2000 24:1047 [Google Scholar]
[3]. Watanabe M, Kishiyama K, Ohkawara A, Acquired progressive lymphangiomaJ Am Acad Dermatol 1983 8:663 [Google Scholar]
[4]. Herron GS, Rouse RV, Kosek JC, Smoller BR, Egbert BM, Benign lymphangioendotheliomaJ Am Acad Dermatol 1994 31:362 [Google Scholar]
[5]. Tadaki T, Aiba S, Masu S, Tagami H, Acquired progressive lymphangioma as a flat erythaematous patch on the abdominal wall of a childArch Dermatol 1988 124:699 [Google Scholar]
[6]. Zhu WY, Penneys NS, Reyes B, Khatib Z, Schachner L, Acquired progressive lymphangiomaJ Am Acad Dermatol 1991 24:813 [Google Scholar]
[7]. Revelles JM, Díaz JL, Angulo J, Santonja C, Kutzner H, Requena L, Giant benign lymphangioendotheliomaJ Cutan Pathol 2012 39:950-56. [Google Scholar]