Case Report
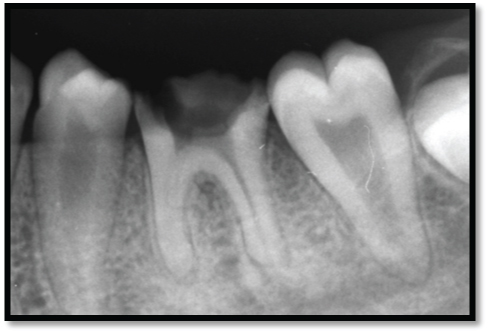
A 33-year-old female patient was referred to the Department of Periodontics, Meenakshi Ammal Dental College by the Department of Oral Medicine and Radiology. The patient complained of tooth pain which was dull and excruciating, and swelling in the lower right posterior region [Table/Fig-1,2]. Intraoral examination showed a large polypoid lesion about 1.5cm ×1.5cm wide with a 2mm diameter stalk protruding from the carious cavity of 46. Pulpal growth was pale pink in colour and was covering the entire carious cavity in relation to 46. Radiographic examination revealed radiolucency extending till the middle third of the tooth and widening of periodontal ligament space [Table/Fig-3]. Initial phase of treatment included complete scaling and root planning. So based on the clinical and radiographic examination these differential diagnosis were possible which included pulp polyp, papilloma or gingival polyp. In the present case, carious teeth with pulpal involvement, short clinical crown, were addressed in preoperative treatment planning.
Preoperative (occlusal view) depicting pulpal growth in relation to 46.

Preoperative (buccal view) depicting short clinical crown length in 46

Preoperative radiograph showing extensive pulpal involvement
The treatment plan was divided into
Step 1: Initial periodontal therapy and re- evaluation and excision of pulpal growth for histological analysis.
Step 2: Endodontic phase.
Step 3: Placement and adjustment of the post.
Step 4: Crown lengthening.
Step 5: Crown preparation of the restored tooth and Luting of finished permanent prosthesis.
Step: 1: Initial periodontal therapy and re-evaluation
Complete oral prophylaxis was done along with scaling and root planing in 46. After phase I therapy the surgical procedure for excisional biopsy of the lesion was performed under local anesthesia using 2% xylocaine hydrochloride with adrenaline (1:80,000). Pulpal growth was excised with a sterile excavator and area was irrigated with saline and the specimen sent for histological examination [Table/Fig-4,5]. The patient was referred to the Department of Endodontic for root canal treatment for 46.
Excised pulpal growth tissue.

Intraoperative view after excision of pulpal tissue and access preparation in relation to 46.

Histological Findings: ([
Table/Fig-6]40x magnification)
Histological picture depicting intense chronic inflammatory cells 40x.
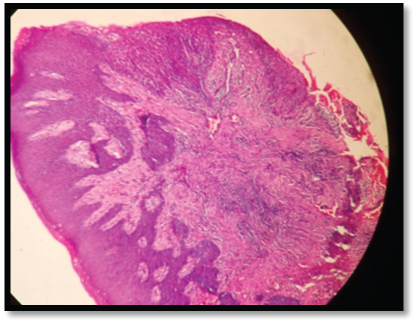
Haematoxylin and Eosin stained soft tissue section showed fibro-collagenous connective tissue with intense chronic inflammatory cells predominantly plasma cells and lymphocytes covered by parakeratinized stratified squamous epithelium which exhibited irregular rete hyperplasia and mild acanthosis with focal ulcerated areas with these findings inflammatory fibroepithelial hyperplasia consistent with the clinical diagnosis of pulp polyp was given.
Step 2: Endodontic procedure
The first step in treatment plan after phase I therapy was to deal with endodontic procedure. After application of the rubberdam, an access cavity was prepared and refined with EX24 bur (nonend cutting tapered fissure; Mani, Japan). Working lengths were determined electronically using an apex locator (Root ZX II, J Morita, koyoto, Japan) and confirmed radiographically. The root canals were instrumented manually with K-files (Mani, Japan). Apical enlargement was then completed to size 25 followed by step back procedure.
After instrumentation, a needle was inserted 1mm short of the working length, and each root canal was irrigated with 5ml of 5% NaOCl (Niclor; Ogna, Milan, Italy). The root canals were dried with sterile paper points and filled using lateral compaction technique with gutta-percha and AH plus sealer (Dentsply De Trey, Konztanz, Germany). Prior to obturation the placement of the gutta-percha cones was confirmed radiographically. Post-endodontically the tooth 46 was restored with zincoxide eugenol [Table/Fig-7].
Radiographic image showing completion of obturation in relation to 46.

Step: 3: Placement and Adjustment of post
The post space was prepared one week after the endodontic treatment was completed. The post space was created using sequential drilling with 1mm, 2mm and 3mm gates glidden drill (Dentsply SEC OK file) and approximately 4mm of guttapercha points was removed using 3 mm peeso reamer (Dentsply Caulk Maillefer Peeso Reamers). A prefabricated post was taken and inserted into the canal space to check for its proper adaptation. A periapical radiograph was taken which ensured that there was a minimum of 4mm guttapercha left in place to protect the apical seal and there was no gap between the post and the filling beneath. A prefabricated metal post was luted using type I GIC (GC gold label luting and lining cement) [Table/Fig-8]. Core built up was done using type IX GIC (GC gold high strength posterior restorative cement). The final finishing & polishing was done with finishing burs. Occlusal interferences in normal & paranormal mandibular movements were removed.
Radiographic image showing Metal post placement with core build-up.

Step.4: Periodontal procedure
Pre-surgical analysis including determination of tooth anatomy, finish line margins of the restoration, biological width analysis and the amount of tooth structure required to be exposed for crown lengthening was assessed. Patient was referred back to department of periodontics for crown lengthening procedure in 46, local anaesthesia was given. Bone sounding was performed. Crevicular incisions were made using Bard–Parker No.15 blade (surgeon sterile blade Kehr surgical private limited) on the facial aspect of 46. A full-thickness muco-periosteal flap was reflected on buccal surface of 46 using periosteal elevator taking care to preserve the maximum amount of gingival connective tissue in the flap [Table/Fig-9]. Flap retraction revealed that the teeth had a sufficient amount of sound tooth structure above the alveolar crest so that an ostectomy was not necessary. Full thickness flap was apically positioned and sutured using 4-0 mersilk and on lingual surface gingivectomy was performed [Table/Fig-10].
Full thickness flap reflected with vertical incision.

Flap sutured using 4-0Mersilk

Post operative care: Following surgery the patient was instructed to avoid chewing in the surgical area during the first postoperative day. She was prescribed systemic antibiotics (Amoxycillin 500mg three times a day for five days) and analgesics (Ibuprofen 400mg three times a day for three days) with instructions to rinse the mouth daily with a solution of 0.2% chlorhexidine di-gluconate for seven days. She was instructed not to brush over the surgical site and was placed on a strict maintenance schedule following surgery.
Healing: After 10 days, the sutures were removed and healing was found to be adequate and satisfactory.
Step -5: Crown preparation of the restored tooth & Luting of finished permanent prosthesis
After root canal treatment and post adjustment, crown preparation of the tooth was done as shown in [Table/Fig-11]. After the crown preparation impression was made and sent to the lab for the processing of porcelain fused to metal crown. The crown was fixed with the help of luting cement i.e. GIC TYPE I (GC gold label luting and lining cement) as shown in the [Table/Fig-12].
Crown preparation in relation to 46

Porcelin fused to metal crown placed.

Discussion
A hyperplastic response of the pulp to acute inflammation occurs in young teeth but has never been reported to have developed in the teeth of middle-aged patients [1,2]. The purpose of this case report is to report the hyperplastic pulpitis in right mandibular molar in middle aged patient and its multidisciplinary management.
Chronic hyperplastic pulpitis is characterized by the development of granulation tissue, covered at times with epithelium and resulting from long standing, low grade irritation [3]. Pulp polyp is rare in middle aged adults but it is more common in teeth of children and adolescents, in which the pulp tissue have a high resistance and a good blood supply. Its colour may vary from cherry red of the granulation tissue to opaque whiteness of moist keratinized epithelium, depending on the degree to which the appearance of the granulation tissue is modified by its covering. It is usually symptomless but discomfort can occur during mastication by the pressure caused due to the food bolus. Response to thermal and electrical stimuli may be normal and it might mimic the proliferating gingival tissues [4,5].
Pulp polyp occurs as a result of an open cavitated carious lesion which acts as a pathway for escape of the inflammatory exudate, tooth fracture due to trauma with pulpal exposure and even long standing fractured restoration can lead to pulpal stimuli and result in pulpal reactions causing pulp polyp. Type I hypersensitivity reactions is also been hypothesized to play a role in pathogenesis of pulp polyp due to the higher concentration of histamine, Immunoglobulin E(Ig-E) and Interleukin -4(IL-4) [6].
When pulp involvement is extensive or long-standing, peri-apical radiograph may reveal an incipient chronic apical periodontitis [7]. Stabholtz et al., and Çalışkan reported that hyperplastic pulpitis associated with periapical involvement presented as radiolucencies or radiopacities on radiographic examination [8–10].
Management of the tooth with chronic hyperplastic pulpitis includes extraction when minimal amount tooth structure remains which is unfavourable for restoration and conservatory approach requires a multidisciplinary approach including endodontic management, surgical crown lengthening and prosthodontic management. In cases of pulp polyp in young adults where there is only coronal pulpal tissue involvement pulpotomy has also been suggested as a treatment option [3]. In this case report root canal treatment was done according to Smulson and Sieraki [7] who suggested that even if the healing of the inflamed pulp occurs, the extensive destruction due carious process and development of pulp polyp makes root canal treatment mandatory.
There should be a healthy relationship between periodontium and tooth, any alteration in balance between the two can ultimately lead to tooth loss. Finish line margins plays key role in maintaining the integrity of the tooth, margins placed beneath the sub-gingival areas can cause severe inflammation, periodontal pocket formation and bone loss. Optimal bone reduction is required according to Wagenberg et al., 1989 [11]. At least 5.0 to 5.25 mm of tooth structure should be above the osseous crest for surgical crown lengthening to establish the ideal biological width of epithelial attachment of 0.97 mm and a connective tissue attachment of 1.07mm [12]. After the surgical crown lengthening immediate temporization should be done and healing period of 12 weeks is recommended before the placement of permanent restoration for posterior teeth and 6 months for anterior aesthetic areas [13]. This paper discusses multidisciplinary approach in the management of chronic hyperplastic pulpitis which was initiated with scaling and root planing, root canal therapy followed by post and core, crown lengthening and restoration of the tooth with porcelain fused to metal crown.
In case of extensive loss of coronal tooth structure, root canal treatment followed by prefabricated metal post. It is readily available and is easy to use which provides retention and stability to the core structure. The metal post helps to withstand the masticatory forces (Mouradian et al.,) [14] and also restores the optimal aesthetics and functions of the tooth (Freedman et al.,) [15]. Hence, this paper highlights about the multidisciplinary approach involved in the management of extensive carious lesion with pulp polyp in middle aged adults.
Conclusion
This case report highlights the unusual presentation of pulp polyp in a middle aged young woman which was confirmed by the histo-pathological analysis. It also enumerates the multidisciplinary approach involved in the treatment of the tooth with chronic hyperplastic pulpitis to restore back the esthetic, phonetics and function of the tooth.
[1]. Stanley HR, Pulp capping: conserving the dental pulp-can it be done; is it worth it?Oral Surg Oral Med and Oral Pathol 1989 68:628-39. [Google Scholar]
[2]. Seltzer S, Bender BI, The dental pulp: biologic considerations in dental procedures 1976 2nd ednPhiladelphia, USAJB Lippincott Co:252-66.:320 [Google Scholar]
[3]. Grossman LI, Oliet S, Del Rio CE, Endodontic Practice 1988 11th ednPhiladelphia, USALea & Febiger:7071:105 [Google Scholar]
[4]. Spouge JO, Oral pathologySt. LouisCV Mosby:57-61. [Google Scholar]
[5]. Walton RE, Pashley DH, Dowden WE, Pulp pathosis. In: Ingle JI, Taintor FC, edsEndodontics 1995 3rd ednPhiladelphia, USALea & Febiger:398-402. [Google Scholar]
[6]. Sattari M, Haghighi AK, Tamijani HD, The relationship of pulp polyp with the presence and concentration of immunoglobulin E, histamine, interleukin 4 and interleukin 12Aust Endod J 2009 35(3):1648 [Google Scholar]
[7]. Smulson MH, Sieraski SM, Histophysiology and diseases of in dental pulp. In: Weine FS, edEndodontic Therapy 1989 4th ednSt. Louis, USACV Mosby:142-45. [Google Scholar]
[8]. Stabholz A, Shekter M, Schwartz Z, Condensing osteitis and chronic hyperplastic pulpitis in the same pulpally involved toothQuint Int 1982 2:137-38. [Google Scholar]
[9]. Çalışkan MK, Success of pulpotomy in the management of hyperplastic pulpitisInt Endod J 1993 26:142-48. [Google Scholar]
[10]. Çalışkan MK, Pulpotomy of carious vital teeth with periapical involvementInt Endod J 1995 28:172-76. [Google Scholar]
[11]. Wagenberg BD, Eskow RN, Exposing adequate tooth structure for restorative dentistryInt J Periodontics Restorative Dent 1989 9:322-31. [Google Scholar]
[12]. Gargiulo AW, Wentz F, Orban B, Dimensions and relations of the dentogingival junction in humansJournal of Periodontology 1961 32:261-67. [Google Scholar]
[13]. Bragger U, Lauchenauer D, Lang NP, Surgical lengthening of the clinical crownJ Clin Periodontol 1992 19:58-63. [Google Scholar]
[14]. Mouradian, WE, The face of a child: Children’s oral health and dental educationJ Dent Educ 2001 65:821-31. [Google Scholar]
[15]. Freedman, G, A look at post and coresDent Today 2002 7:118-19. [Google Scholar]