Acute Pancreatitis in a Patient with Complicated Falciparum Malaria
Bhupen Barman1, Prasanta Kumar Bhattacharya2, Kryshan G Lynrah3, Tony Ete4, Neel Kanth Issar5
1 Assistant Professor, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India.
2 Professor and HOD, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India.
3 Associate Professor, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India.
4 Senior Resident, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India.
5 Post Graduate Trainee, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Shillong, Meghalaya, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Bhupen Barman, Assistant Professor, Department of General Medicine, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGRIHMS), Mawdiangdiang, Shillong-793018, Meghalaya, India.
E-mail: drbhupenb@gmail.com
Malaria is one of the most common protozoan diseases, especially in tropical countries. The clinical manifestation of malaria, especially falciparum malaria varies from mild acute febrile illness to life threatening severe systemic complications involving one or more organ systems. We would like to report a case of complicated falciparum malaria involving cerebral, renal, hepatic system along with acute pancreatitis. The patient was successfully treated with anti malarial and other supportive treatment. To the best of our knowledge there are very few reports of acute pancreatitis due to malaria. Falciparum malaria therefore should be added to the list of infectious agents causing acute pancreatitis especially in areas where malaria is endemic.
Acute febrile illness, Atypical presentation, Pain abdomen, Protozoan disease
Case Report
A 65-year-old male, from malaria endemic area was admitted with history of high grade fever associated with chills and rigor for one week. It was associated with mild abdominal pain followed by decreasing urine output and altered sensorium. There was no significant past history of major illness. The patient denied any history of alcohol or use of illicit drugs. There was also no history of taking steroids, analgesics or any other medications in the recent past. On examination, patient was stuporous, febrile (102o F) with pulse rate of 106/minute and blood pressure of 110/60 mmHg. Patient had severe pallor, mild jaundice and bilateral leg oedema. Blood investigations [Table/Fig-1] showed severe anaemia with polymorphonuclear leukocytosis and normal erythrocyte sedimentation rate (ESR).
Showing changes in hematological parameters during admission.
| Laboratory Parameter (units) | Report | On Discharge (Day 10) | Reference values |
|---|
| On admission | Day 6 |
|---|
| Haemogram |
| Hemoglobin (gm/dL) | 4.8 | 6.2 | 9.8 | 12-18 |
| Total Leucocytic count (x103/mm3) | 10.0 | 11.20 | 8.6 | 4.0 – 11.0 |
| Differential leucocytic count (%)NeutrophilLymphocyteMonocyteEosinophilBasophil | 8413030000 | 7025030200 | 7621020100 | 40-7520-452-101-6≤1 |
| Platelet count (x103/mm3) | 165 | 260 | 280 | 150- 400 |
| Erythrocyte Sedimentation rate (mm/h) | 08 | 12 | 15 | 0-20 |
| Peripheral blood smear | Trophozoite of Pf with parasitic index of 1.5% | Normal | | |
| Paracheck rapid antigen test | Positive for Pf malaria | | | |
| Liver Function Tests |
| Bilirubin (mg/dL)Total DirectIndirect | 2.31.11.2 | 1.90.51.4 | 1.40.60.8 | 0.3 – 1.30.1 - 0.40.2 - 0.9 |
| ALT (U/L) | 60 | 85 | 54 | 7 - 41 |
| AST (U/L) | 24 | 34 | 36 | 12 - 38 |
| Alkaline Phosphatase (IU/L) | 110 | 92 | 87 | 30-120 |
| Protein, total (g/dL) | 5.8 | 6.2 | 6.8 | 6.3-8.2 |
| Albumin (g/dL) | 2.1 | 2.1 | 3.2 | 3.5-5.0 |
| Globulin (g/dL) | 3.7 | 4.1 | 3.6 | 1.5-3.0 |
| Coagulation Profile |
| Prothrombin Time (s) | 18.1 | 14.2 | Not done | 12.7 – 15.4 |
| INR | 1.47 | 1.38 | Not done | 1.34 |
| APTT (s) | 41.2 | 38.2 | Not done | 26.3 – 39.4 |
| Renal Profile |
| Serum Creatinine (mg/dL) | 11.8 | 2.1 | 1.2 | 0.5 - 0.9 |
| Blood Urea (mg/dL) | 522 | 100 | 48 | 10-50 |
| Sodium (meq/L) | 145 | 138 | 143 | 135-145 |
| Potassium (meq/L) | 5.6 | 3.8 | 4.01 | 3.5-5.5 |
| Calcium (mg/dL) | 9.2 | 9.3 | 9.4 | 8.7 – 10.2 |
| Chloride (meq/L) | 111 | 110 | 110 | 90-110 |
| Blood Glucose, Random (mg/dL) | 103 | 108 | 106 | 70-140 |
| Serum Amylase (U/L) | 1955 | 1051 | 345 | 20-96 |
| Serum Lipase (U/L) | 5501 | 1150 | 112 | 115-221 |
| Serum Lipid Profile (mg/dl) |
| Total Cholesterol | 200 | Not done | Not done | < 200 |
| Low Density Lipoprotein (LDL) | 75 | Not done | Not done | < 100 |
| High Density Lipoprotein (HDL) | 10 | Not done | Not done | 19-62 |
| triglyceride | 289 | Not done | Not done | 53-150 |
| Blood Culture | Sterile | Not done | Not done | |
| HIV I, II | Non Reactive | Not done | Not done | |
| HBsAg | Negative | Not done | Not done | |
| Anti HCV | Negative | Not done | Not done | |
ALT = Alanine Aminotransferase; AST = Aspartate Aminotransferase; INR = International Normalised Ratio; APTT = Activated Partial Thromboplastin Time, Pf = Plasmodium Falciparum
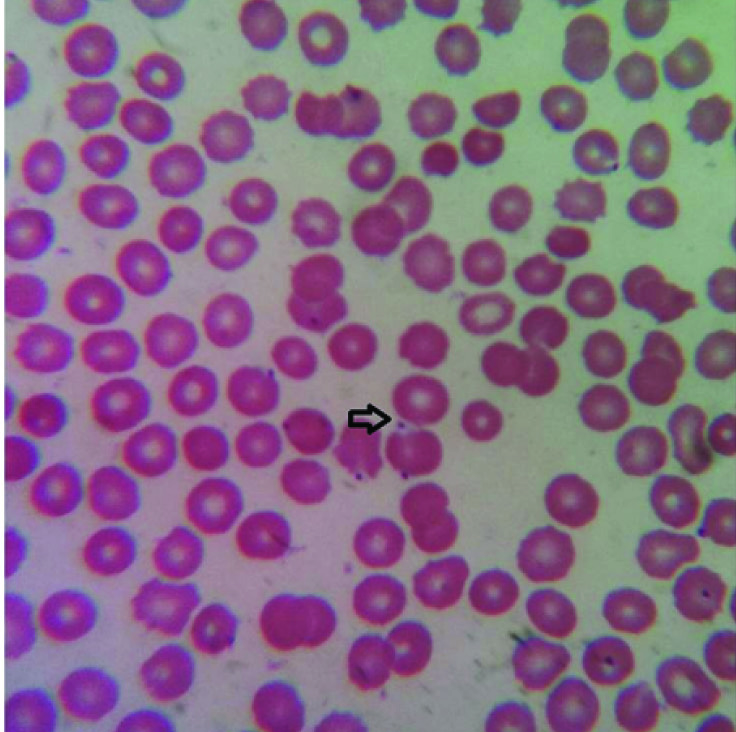
Peripheral blood smear demonstrated accole formation of falciparum malaria [Table/Fig-2] with parasitic index of 1.5% and Paracheck rapid antigen test for plasmodium falciparum malaria was positive.
Peripheral blood smear demonstrated accole formation of falciparum malaria. (Leishmans stain 100x).
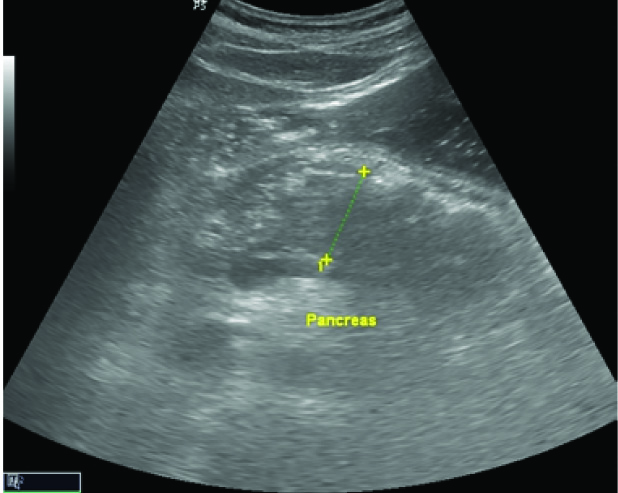
The patient had severe renal dysfunction with hyperkalemia with raised levels of serum amylase and lipase. His random blood sugar, serum sodium and calcium and chest x-ray were within normal limit. The viral markers for HIV and Hepatitis B & C were non reactive. Blood culture (three samples taken within 12 hours of hospitalization) was sterile. Sonography of abdomen showed bulky and hypoechoic body and tail of pancreas suggestive of acute pancreatitis [Table/Fig-3].
Ultrasonograhy shows features suggestive of acute pancreatitis. The pancreatic body and tail are bulky and hypoechoic due to edema anterior to the pancreatic duct.
Diagnosis of complicated falciparum malaria and acute pancreatitis was made. Patient was given intravenous Artesunate (120 mg stat, followed by after 12 hours and 24 hours and than daily for total 7 days) with oral Doxycycline (100 mg twice daily for 10 days), intravenous Imipenem (500 mg thrice daily for 7 days), intravenous fluids and other supportive measures. Haemodialysis was done on day one and day three of admission with two units of packed red cell transfusion. Over the next three days, patient regained his consciousness and became afebrile and anicteric. Follow up investigations on day sixth showed improvement in blood parameters and clearance of parasites from peripheral blood smear. Contrast enhanced computerised tomography of abdomen done on day seventh after normalisation of renal function, showed bulky and oedematous pancreas and diffuse hypo enhancement of pancreas without any evidence of necrosis [Table/Fig-4].
Noncontrast CT scan reveals enlarged pancreatic head and tail with peripancreatic fatty stranding

There was mild peripancreatic fat stranding and oedema of adjoining second part of duodenum. Patient was discharged on day tenth of admission. He was asymptomatic on follow up after two weeks.
Discussion
Malaria is one of the most common protozal diseases of human caused by plasmodium falciparum and transmitted by the bite of infected anopheles mosquitoes. The disease is characterized by protean manifestations ranging from acute febrile illness to various systemic complications either in isolation or in combination. According to recent WHO data, the disease is endemic in 97 countries affecting over 198 million peoples (range 124-283 million) and responsible for 5,84,000 deaths (range 124000-755000) annually [1]. Acute pancreatitis as a presenting manifestation or complication of falciparum malaria, although documented is rare and a few cases have been reported in the literature especially from tropical countries like India [2,3]. There is evidence of association of falciparum malaria and acute haemorrhagic pancreatitis in autopsy series where parasitized red cells and rosettes have been demonstrated in the small blood vessels of pancreas [4]. The parasitized erythrocytes bind with the receptors of the endothelial cells by the formation of knobs and by the process of cyto adherence, agglutination (P. falciparum–infected RBCs adhere to other parasitized erythrocytes), and resetting (P. falciparum–infected RBCs adhere to uninfected RBCs) causes obstruction of microvasculature blood flow. These vascular changes lead to anoxic damage or ischemia resulting in activation of pancreatic enzymes and damage to the pancreatic tissues. Several vascular receptors for the adhesive surface protein of infected red cells have been identified, which causes adhesion of the infected erythrocytes to the vascular endothelium. The molecules responsible are CD 36, vascular cell adhesion molecule 1(VCAM 1), thrombospondin (TSP), intra cellular adhesion molecule 1(ICAM 1) and histidine rich protein (HRP) [5]. The resulting micro vascular damage may be exacerbated by the release of cytokines such as tumour necrosis factor (TNF) and toxic substances by the parasite. The releases of cytokines make the endothelial cells more adhesive for the surface of parasitized erythrocytes.
The indexed patient presented with high grade fever followed by abdominal pain and decreased urine output. Though pain abdomen is a frequent presenting symptom of falciparum malaria and often multifactorial [6–10], pancreatitis is one of the rare causes for the same and if it goes undetected can often be fatal. However it can be cured with proper early initiation of treatment.
Clinical accidents may happen due to failure of recognizing malaria as a cause of pancreatitis and vice versa [11]. The purpose of presenting this case is add to the body of evidence that pancreatitis is an atypical complication of malaria and should be suspected under compatible clinical setting. Furthermore in a case of acute pancreatitis of unrecognized aetiology, malaria should be rule out.
Conclusion
Despite being entirely preventable and curable disease, malaria continues to pose a major public health challenge in developing countries. Acute pancreatitis is a rare complication of falciparum malaria. A high degree of suspicion and an inquisitive approach will help for early diagnosis and successful management of this potentially severe and rare complication of plasmodium falciparum malaria.
ALT = Alanine Aminotransferase; AST = Aspartate Aminotransferase; INR = International Normalised Ratio; APTT = Activated Partial Thromboplastin Time, Pf = Plasmodium Falciparum
[1]. World Health Organization. World Malaria Report 2014. http://www. who.int/malaria/publications/world_malaria_report_2014/en (accessed on 28/09/2015) [Google Scholar]
[2]. Kumar S, Jain AP, Vikas Falciparum malaria presenting as acute pancreatitisJ Vector Borne Dis 2010 47(2):121-22. [Google Scholar]
[3]. Seshadri P, Dev AV, Viggeswarpu S, Sathyendra S, Peter JV, Acute pancreatitis and subdural haematoma in a patient with severe falciparum malaria: case report and review of literatureMalar J 2008 30(7):97 [Google Scholar]
[4]. Gurman G, Schlaeffer F, Alkan M, Heilig I, Adult respiratory distress syndrome and pancreatitis as complications of falciparum malariaCrit Care Med 1988 16(2):205-06. [Google Scholar]
[5]. White NJ, Malaria. In the Manson’s Tropical Disease. Gordon Cook (Eds) 2003 21st Edition:1205-1295. [Google Scholar]
[6]. Anthoine-Milhomme MC, Chappuy H, Cheron G, Acute acalculous cholecystitis in a child returning from the Ivory CoastPediatr Emerg Care 2007 23:242-43. [Google Scholar]
[7]. Jimenez BC, Navarro M, Huerga H, Lopez-Velez R, Spontaneous splenic rupture due to Plasmodium vivax in a traveler: case report and reviewJ Travel Med 2007 14:188-91. [Google Scholar]
[8]. Kim A, Park YK, Lee JS, Chung MH, Kim ES, A case of symptomatic splenic infarction in vivax malariaKorean J parasitol 2007 45:55-58. [Google Scholar]
[9]. Beg MA, Sani N, Mehraj V, Jafri W, Khan MA, Malik A, Comparative features and outcomes of malaria at a tertiary care hospital in Karachi, PakistanInt J Infect Dis 2008 12:37-42. [Google Scholar]
[10]. Koh KH, Chew PH, Kiyu A, A retrospective study of malaria infections in an intensive care unit of a general hospital in MalaysiaSingapore Med J 2004 45:28-36. [Google Scholar]
[11]. Bandhal SS, Irshad M, Bandhal S, Yadav K, Acute on chronic pancreatitis masking falciparum malaria: a case reportGlobal journal of health science 2009 1(2):123-25. [Google Scholar]