Numerous studies have shown that placement of implants in the maxillary region with resultant successful osseointegration can be achieved by the use of sinus lift procedures using piezosurgical technique. In this case report a middle aged patient had come to the outpatient department of A. J. Institute of Dental Sciences with a chief complaint of missing right posterior molar. Since the radiographic ball marker showed only 4 mm bone below the sinus in #16 region, direct sinus lift procedure was done for placement of a dental implant. Piezosurgery was performed, as it reduces the risk of damaging vital soft tissues such as nerves, dura matter and blood vessels. To stabilize the implant in the maxillary sinus region and also to stimulate bone regeneration, gamma irradiated cancellous allograft was used. Periapical radiographs were taken 10 months after implant placement which showed good bone growth over the implant collar. Bone formation in the maxillary antrum was seen clearly in the panoramic radiograph. Using piezosurgical unit, sinus lift procedure with sinus grafting proved to be less traumatic and more successful.
Allograft, Bone augmentation, Endosseous implant, Sinus lift
Case Report
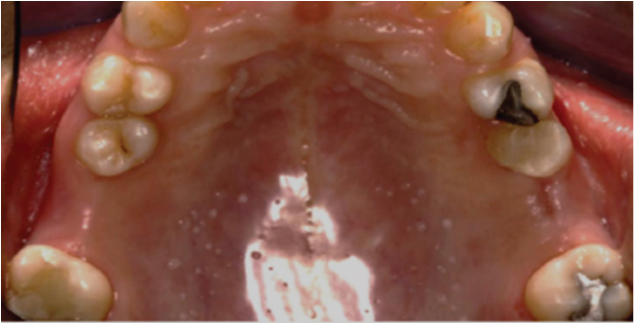
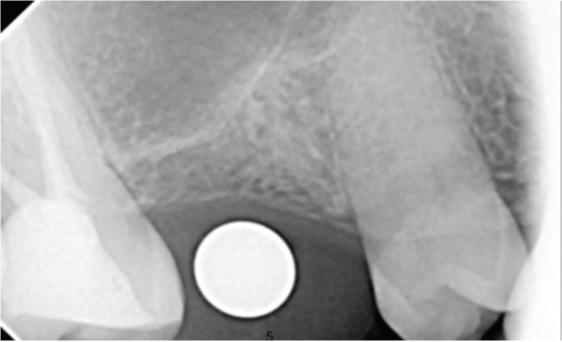
A 42-year-old female patient came to the outpatient Department of A J Institute of Dental Sciences, Mangalore in 2014, with a chief complaint of missing upper back teeth. On examination, teeth no #16 and #26 were missing [Table/Fig-1]. Detailed case history of the patient revealed that both the teeth were extracted due to extensive caries and persistent pain. The patient had no relevant extraoral or intraoral abnormalities. Blood investigations were done which revealed no systemic abnormalities. The orthopentamograph (OPG) taken revealed that the bone height in 16 region and the maxillary antrum was insufficient for implant placement [Table/Fig-2]. Intra Oral Periapical Radiograph (IOPA) done with a radiographic ball marker showed only 4 mm bone below the sinus in #16 region [Table/Fig-3].
Missing lower back teeth (16 and 26).
Orthopentamograph (OPG) shows maxillary antrum pneumatised in #16 region.

IOPA done with a radiographic ball marker showed only 4mm bone below the sinus in 16 region.
Alveolar bone was homogenous in nature and bone mapping revealed the crestal width of bone in relation to 16 was 6.5 mm. According to Misch’s classification [1], bone density showed D3 type of bone. Prior to the surgery, informed consent was taken from the patient. Alternatives to the treatment were explained and she was also informed about the benefits and risks of each treatment option. As the patient wanted to avoid removable prosthesis due to its inconvenience, implant placement was opted.
Pre-surgical diagnostic casts were prepared. In the cast, the inter-occlusal distance was measured as 9 mm with respect to #16 and 8 mm with respect to #26 respectively. The interocclusal space in relation to #16 was 5 mm and 6 mm with respect to # 26 [Table/Fig-4].
Diagnostic cast prepared prior surgery.

Surgical phase
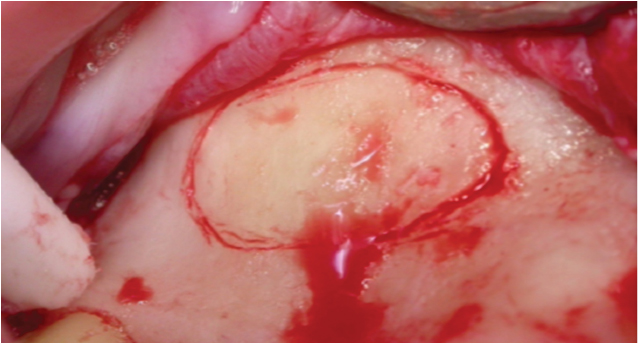
Prior to the surgical procedure, preparation of the patient was done. The maxillary posterior segment was anaesthetised with buccal and palatal infiltration using local anaesthesia of 2% lignocaine with 1:80,000 adrenaline. Once the patient was anaesthetized, an incison was made using no.15 surgical blade extending from the mesial surface of #16 up to the mesial surface of #15. A vertical incision was extended until the end of the buccal vestibule. A full thickness buccal flap was raised until the zygomatic buttress which was held in position with a Tatum Sinus Retractor throughout the surgical procedure. A bony window was then traced in the #16 region using a Piezo-surgical unit [Table/Fig-5]. The initial bone marking was done using tip #BS5. This was followed by the deepening of the mark using SL1 tip.
Bony window was traced in the #16 region using a Piezo-surgical unit.
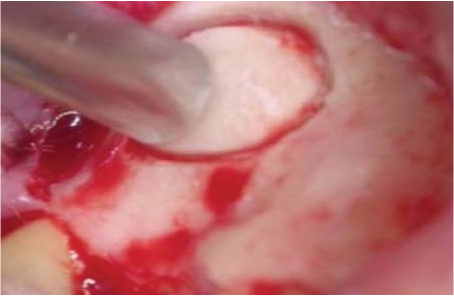
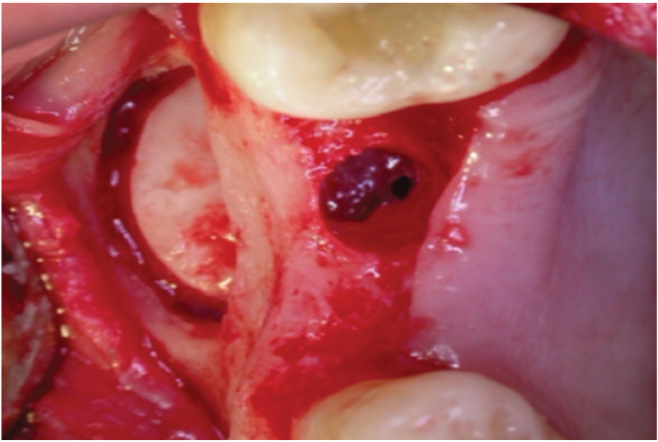
The bone tracing was made until a very thin plate of buccal bone remained over the sinus lining. A mouth mirror handle was then used to fracture the remaining buccal plate [Table/Fig-6]. The fractured section of bone was kept attached to the antral lining and no attempt was made to separate it from the lining. A SL2 tip was used to round off the bony window. This was followed by the SL3 tip to raise the lining in the vicinity of the bony window. The partially raised lining was then lifted to a greater extent using the BS4 & BS5 tips [Table/Fig-7]. The palatal flap was raised over the crest in #16 region. An osteotomy was done in the #16 region in the usual way, protecting the raised sinus lining from any damage with the implant drills. Osteotomy was widened to 4.5mm [Table/Fig-8].
A mouth mirror handle was then used to fracture the remaining buccal plate.
Partially raised lining was then lifted to a greater extent using the BS4 & BS5 tips.

Osteotomy widened to 4.5mm
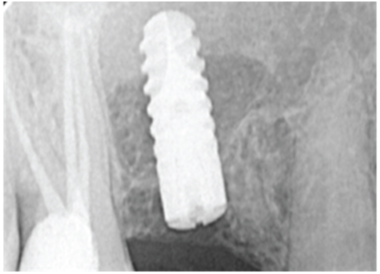
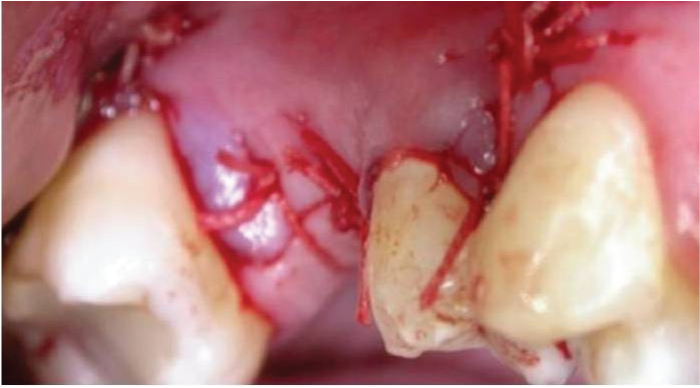
One cc of cancellous particulate allograft from Rocky Mountain tissue bank-Colorado, USA, was placed in the space between the raised sinus lining and the floor of the sinus. Ankylos (4.5mm, 11mm) implants were then placed in the sockets and tapped in place using the motor driver at 25 rpm. As the implant was seated, it pushed the bone graft apically, which in turn elevated the sinus floor. Once the implant-seating tip reached the crest of the bone, the implant was properly seated. The implant mount was removed after judging the sub-crestal placement of the implant by 1mm. The remaining space between the implant and sinus floor was again filled with the gamma irradiated bone graft [Table/Fig-9]. Bone graft was not packed too tight into the space. Flaps were approximated and primary sutures were placed using 3-0 vicryl [Table/Fig-10]. Post implant placement, an IOPA was taken to assess the position of the implant [Table/Fig-11]. The patient was given postoperative antibiotic and anti-inflammatory cover. After postoperative instructions were given, the patient was recalled in 10 days for re-evaluation and suture removal.
The sockets were half-filled with gamma irradiated cancellous bone graft (allograft).
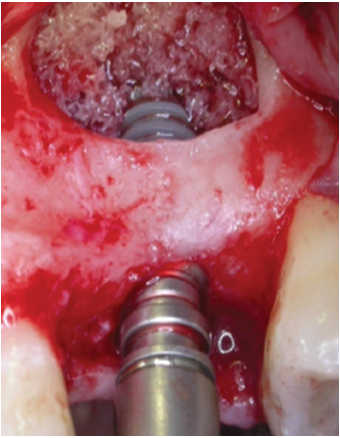
Ankylos 4.5mm 11mm implants were then placed in the sockets.
Flaps approximated & Primary sutures placed using 3-0 vicryl.
Prosthetic Phase
After a healing period of 3 months of implant placement, the implant sealing screw was removed and a gingival former (GH) was placed [Table/Fig-12]. The gingival former was removed after one week [Table/Fig-13]. An impression was made using a closed tray technique with polyether (impregum-3M). The abutment selection was done using the posterior balance selection tray technique. Posterior balance abutment with GH 0.75 and 15 degree angulation were placed [Table/Fig-14]. The abutment tightened with a torque driver at 15Ncm. Access hole was sealed with light cure composite resin.
Implant sealing screw was removed and a gingival former (GH3) was placed.

Emergence profile with gingival former.


Pattern resin was used in the fabrication of abutment jig [Table/Fig-15]. After a week, metal coping trial was prepared on the milled abutment to check for proper positioning of the crown. Proximal contacts were checked thoroughly to ensure proper seating and the occlusion was adjusted for centric and lateral movements. Shade A3 (VITA classic shade guide) was selected for the final porcelain fused to metal crown (PFM). A bisque trial of the crown was done after 3 days [Table/Fig-16]. Finally the PFM crown cementation with zinc phosphate cement was done [Table/Fig-17]. All excess cement was removed and floss ability of contacts was checked. An IOPA was taken to check for excess cement and crown fit [Table/Fig-18].
Abutment jig made in pattern resin.

Bisque trial of the crown.
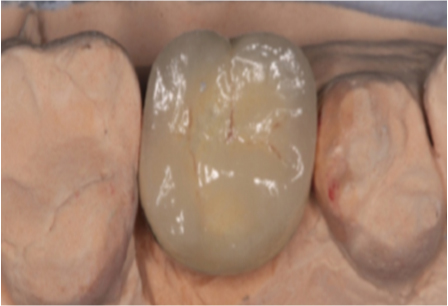
Final crown placed (porcelain fused to metal).

Postoperative radiogragh.

Maintenance phase
Following the prosthetic restoration, the main concern was proper home care (provided that proper margins and embrasures with proper occlusion were present during the fabrication of the prosthesis). The patient was given postoperative instructions and was advised to maintain her oral hygiene with the use of chlorhexidine mouthwash, inter-dental brushes and dental floss. Recall visit was scheduled for the patient every 3 weeks, 1 month, 6 months and 1 year for regular checkup.
Follow-up
The surgical site healed without complication or infection following implant placement. The patient reported minor discomfort during the second day post surgery. This was managed by analgesics, and no pain or discomfort was reported thereafter. Evidence of good clinical ridge contour was noted during the first 6 months of healing. Periapical radiographs were taken 12 months after implant placement which showed good bone growth over the implant collar. Bone formation in the maxillary antrum was seen clearly 12 months after the sinus lift. The sinus cavity around the implants was filled with a dense bone-like tissue. Radiographic analysis showed that the final bone gain was very significant with these implants.
Discussion
Sinus floor elevation with bone augmentation of the maxillary sinus is now a well accepted procedure used to increase bone volume in the posterior maxilla. In the present case, on radiographic examination, the available bone height in the right molar region was found to be only 4 mm from the maxillary sinus lining. Since the patient had a missing right molar for more than a year, there was atrophy of the edentulous area. This could have caused continuous loss of bone height and density and an increase in antral pneumatization [2,3]. Following certain basic criteria such as position of the implant, preexisting tooth form and position, its relation with the opposing arch, soft tissue as well as maxillary sinus anatomy and bone dimension, the decision of direct sinus lift with bone augmentation was made. Bone augmentation is required where the interocclusal dimension is normal or just moderately increased. The interocclusal distance in this case was 9 mm with respect to #16. Short term to long term clinical studies of dental implants placed into grafted sinus demonstrate a similar or even higher survival rate than for implant placed in the maxilla without a sinus augmentation procedure [4]. Gamma irradiated cancellous bone graft was used in this case. Gamma irradiation from Cobalt 60 sources has been used to terminally sterilize bone allografts for many years. These methods attempt to reduce the antigenicity of the bone graft while providing sterilization that can kill bacterial spores and viruses [5]. But the mechanical property of the allograft is reduced due to splitting of the collagen backbone of the bone matrix by the gamma rays, during gamma irradiation. A study done by Nicholas A. Russell et al., in 2012 suggests that the use of 10 kGy preserved the mechanical properties of the bone in both three and four-point bending [6]. Hence, dose dependant gamma radiated allograft was used in this case.
The traditional sinus lift membrane technique implies a great risk of perforating the "Schniderian Membrane", which is the most common complication. Perforation of sinus membrane can occur either while preparing the window or while separating the sinus membrane and performing the ostectomy using the surgical round bur [7,8]. In order to overcome these drawbacks, peizosurgical technique was used in our case. This technique prevents perforation of the "Schniderian Membrane" and cause minimal postoperative complications. Histomorphological studies reveal that the piezoelectric surgery increases the concentration of Bone Morphogenic Protein (BMP-4), Transforming Growth Factor (TGF) beta-2, Tumour Necrosis Factor (TNF) and Interleukin-1, 10 and decreases some of the pro inflammatory cytokines in the bone. Thus, neo-osteogenesis was proven to be consistently more active in cases where piezosurgery is used [9–11]. In this procedure, ultrasound vibration created during cutting, stimulates cells metabolism and since, there is lack of necrosis, bone regeneration is accelerated. Moreover, the oxygen molecules that are released have an antiseptic effect. Oscillation frequency used in piezosurgery is designed for acting only on mineralized tissue; therefore, the cutting tip becomes inactive when it comes in contact with soft tissue [12–15]. Hence, soft tissue damage is not noticed [8,16,17]. Piezosurgery is safely used in dentistry and other fields of medicine where there is high risk of damaging vital soft tissues such as nerves, dura matter, vessels, and so on [12,14,18].
Once the bony window was prepared with piezosurgical procedures, osteotomy was widened to 4.5 mm in the #16 region protecting the raised sinus lining. This trephined core of autogenous bone in many cases helps the vertical bone augmentation during the elevation of the sinus floor [19]. Since, the crestal width of bone in # 16 region was 6.5 mm, an implant named Ankylos 4.5 mm 11mm implant was placed in the area and tapped in place using the motor driver at 25 rpm. The morse taper abutment connection of ankylos implant provides high resistance to bending and rotational torque during clinical function, which significantly reduces the possibilities of screw fracture or loosening. The porcelain fused to metal crown (PFM) was placed over the implant which was preferred since the crown was placed in the posterior region. A PFM’s metal substructure achieves a more exact fit and greater strength over its tooth than an all-ceramic crown.
Conclusion
Sufficient bone density is required for placement of dental implants in non dentate areas of the maxillary posterior region. Bone density may be reduced due to inferior expansion of the maxillary sinus involving the residual ridge area. This case was challenging since there was ridge resorption, with reduced vertical bone height and pnuematization of the maxillary sinus. Hence we adopted piezosurgical technique which was comparatively a safer approach to the maxillary sinus, allowing sinus membrane integrity to be maintained during the surgical procedures when compared to conventional techniques. Success of the dental implant with sinus augmentation mainly depends on the skill of the operator, adequate preoperative planning, technique used to place an implant and the type of graft material used.
[1]. Misch CE, Contemporary Implant Dentistry 1999 Ed 2St. Louis [Google Scholar]
[2]. Garg AK, Augmentation grafting of the maxillary sinus for the placement of dental implants: Anatomy, physiology and procedureImplant Dent 1994 8:36-46. [Google Scholar]
[3]. Thomas GJ, Sinu s lifts—a possible solution to the atrophic maxillaJ Macomb Dent 1990 29:9-11. [Google Scholar]
[4]. Jensen OT, Shulman LB, Block MS, Iacono VJ, Report of the sinus consensus conference of 1996Int J Oral Maxillofac Implants 1998 13:11-45. [Google Scholar]
[5]. Nguyen H, Morgan DA, Forwood MR, Sterilization of allograft bone: effects of gamma irradiation on allograft biology and biomechanicsCell Tissue Bank 2007 8:93-105. [Google Scholar]
[6]. Russell NA, Rives A, Pelletier MH, Bruce WJ, Walsh WR, The effect of sterilization on the mechanical properties of intact rabbit humeri in three-point bending, four-point bending and torsionCell Tissue Bank 2013 14:231-42. [Google Scholar]
[7]. Vercellotti T, Technological characteristics and clinical indications of piezoelectric bone surgeryMinerva Stomatol 2004 53:207-14. [Google Scholar]
[8]. Schlee M, Steigmann M, Bratu E, Garg AK, Piezosurgery: basics and possibilitiesImplant Dent 2006 1:334-40. [Google Scholar]
[9]. Chopra P, Chopra P, Piezosurgery and its applications in periodontology and ImplantologyInt J Contemp Dent 2011 2:16-24. [Google Scholar]
[10]. Yaman Z, Suer BT, Piezoelectric surgery in oral and maxillofacial surgeryAnnals of Oral and Maxillofacial Surgery 2013 1:1-9. [Google Scholar]
[11]. Vercelotti T, Nevins ML, Kim DM, Wada K, Schenk RK, Fiorellini JP, Osseous response following resective therapy with piezosurgeryInt J Perio Rest Dent 2005 25:543-49. [Google Scholar]
[12]. Heinemann F, Hasan I, Kunert-Keil C, Götz W, Gedrange T, Spassov A, Experimental and histological investigations of the bone using two different oscillating osteotomy techniques compared with conventional rotary osteotomyAnn Anat 2012 194:165-70. [Google Scholar]
[13]. Barone A, Santini S, Marconcini S, Giacomelli L, Gherlone E, Covani U, Osteotomy and membrane elevation during the maxillary sinus augmentation procedure. A comparative study: Piezoelectric device vs. conventional rotative instrumentsClin Oral Implants Res 2008 19:511-15. [Google Scholar]
[14]. Pavlíková G, Foltán R, Horká M, Hanzelka T, Borunska H, Sedy J, Piezosurgery in oral and maxillofacial surgeryInt J Oral Maxillofac Surg 2011 40:451-57. [Google Scholar]
[15]. Pippi R, Alvaro R, Piezosurgery for the lingual split technique in mandibular third molar removal: a suggestionJ Craniofac Surg 2013 24:531-33. [Google Scholar]
[16]. Stübinger S, Landes C, Seitz O, Zeilhofer HF, Sader R, Ultrasonic bone cutting in oral surgery: a review of 60 casesUltraschall Med 2008 29:66-71. [Google Scholar]
[17]. Troiani C, Russo C, Ballarani G, Piezoelectric surgery: a new reality to cut and manage bone in maxillo-odonto- stomatologyInt J Maxillo Odontostomatology 2005 4:23-28. [Google Scholar]
[18]. Seshan H, Konuganti K, Zope S, Piezosurgery in periodontology and oral implantologyJ Indian Soc Periodontol 2009 13:155-56. [Google Scholar]
[19]. Nalbandian S, Piezosurgery techniques in implant dentistryAustralasian Dental Practice 2011 :116-26. [Google Scholar]