Eccrine Porocarcinoma of the Scalp: A Rare Case Report with Review of Literature
Smita Surendra Masamatti1, Aparna Narasimha2, Amoolya Bhat3, Vijaya Chowdappa4
1 Assistant Professor, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, India.
2 Professor, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, India.
3 Assistant Professor, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, India.
4 Head of the Department, Department of Pathology, Sapthagiri Institute of Medical Sciences and Research Centre, Bangalore, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aparna Narasimha, No.22, “Moyenvilla”, Moyenville Road, Langford Town, Bangalore-560025, India.
E-mail: sonrichie14@gmail.com
Eccrine porocarcinoma (EPC) is a potentially lethal neoplasm of the skin that arises from the intraepidermal portion of the eccrine sweat glands. It was previously known as eccrine adenocarcinoma or malignant eccrine poroma. It commonly occurs between 60 to 80 years of age, usually arising from hands and feet. However, few case reports on involvement of rare sites such as scalp, face and eyelids are present in literature. We herein report an unusual case of porocarcinoma arising on the right parieto occipital region of scalp in a 29-year-old young female patient. To the best of our knowledge, there have been fewer than 20 cases of porocarcinoma arising on scalp with fewer than 10 cases seen in younger age group reported previously in the literature.
Eccrine porocarcinoma, Histopathology, Malignant tumor, Scalp
Case Report
A 29-year-old female patient presented with a gradually increasing painless lobulated mass at right parieto-occipital region along with headache since one year. All routine investigations along with CT brain were within normal limits. On examination, the swelling was multilobulated measuring about 6x5x3 cm, showing surface ulceration with focal loss of hair and along with loss of pigmentation. The mass was mobile, free from the underlying structures and bled on touch. No regional lymphadenopathy was noted. A presumptive diagnosis of soft tissue sarcoma was given. FNAC was attempted twice, but yielded only haemorrhage as it was very vascular, located over scalp region. Hence, the mass was excised and sent for histopathological evaluation.
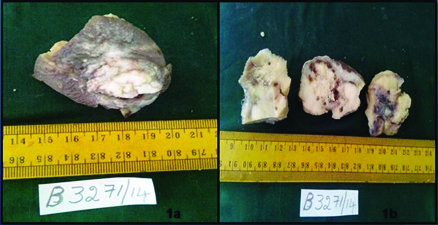
Grossly, the specimen showed a skin covered mass with surface ulceration together measuring 5x4x3 cm. The cut surface of the tumour showed grey white appearance with areas of haemorrhage and cystic degeneration [Table/Fig-1].
a) Gross specimen showing skin covered mass; b) Cut surfaces showing grey white appearance with areas of haemorrhage and necrosis
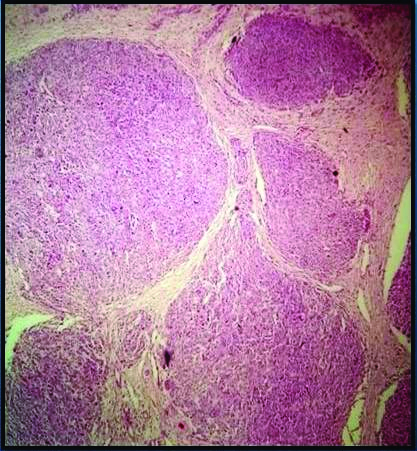
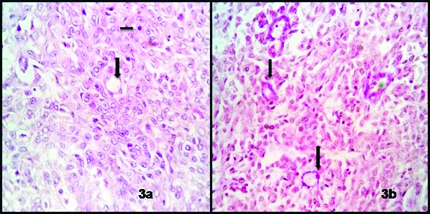
Microscopic examination revealed skin with an underlying infiltrating tumour composed of polygonal to cuboidal cells having pleomorphic vesicular nuclei with prominent one to two nucleoli and having moderate to abundant pale cytoplasm arranged in lobules, nests and cords which are separated by thick fibrous septae [Table/Fig-2]. Many mitotic figures (upto 6-7/hpf) along with duct formation [Table/Fig-3a] and foci of tumor necrosis were noted. Ducts stained with Pas stain [Table/Fig-3b]. At places lymphatic tumour emboli were noted. The tumour depth noted was >7mm and was seen reaching upto the deep surgical margin.
Microphotograph showing lobules of malignant cells separated by thin fibrous septae (H&E,X400)
a) Microphotograph showing malignant cells with few mitotic figures and duct formation, (H&E, X100); b) Ducts highlighted by special stain (PAS stain, X100)
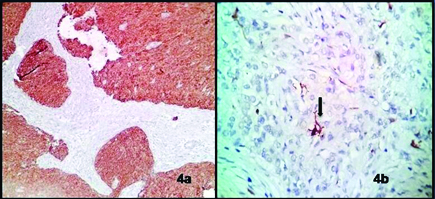
Immunohistochemical studies showed that the tumour cells were positive for cytokeratin [Table/Fig-4a] and the ductal structures were highlighted by carcinoembryogenic antigen (CEA) [Table/Fig-4b]. Based on these findings the diagnosis of eccrine porocarcinoma was arrived at. The patient developed recurrence after six months of surgery and was referred to higher centres for further management.
a) Microphotograph of Immunohistochemistry marker (pan CK) showing diffuse membrane positivity, (X100); b) Carcinoembryonic antigen (CEA) highlighting the ducts, (X100)
Discussion
Eccrine porocarcinoma also known as malignant eccrine poroma is a rare adnexal tumour that accounts for 0.005% to 0.01% of all epidermal skin neoplasms [1]. It may arise denovo as a primary tumour or develop from pre existing benign poromas after a long latency. The tumour was first described by Pinkus and Mehregan in 1963. The term eccrine Porocarcinoma was introduced by Mishima and Morioka in 1969, since then EPC have been reported fewer than 300 cases worldwide. It occurs most often in the elderly, with the age at diagnosis being between 60-80 years [2]. The tumour varies greatly in size from < 1cm to 10 cm. It commonly affects lower limbs (44%) followed by trunk (21%), head (18%), upper limb (11%) and neck (3%). Rare sites such as scalp (<5%), face, eyelids, vulva, scrotum, penis and periungual region have also been reported in the literature [3,4]. Ritter et al., and Matloub et al., have reported EPC occurring at occipital region while Roshani et al., reported EPC in left frontoparietal region [5]. Our’s is the first case of EPC seen in young female occurring at right parieto occipital region. A long standing history is often encountered (upto 50 years) reflecting that these tumours originate from pre existing benign poroma [6]. In our case there was no history of pre-existing benign lesions.
Few cases of eccrine porocarcinoma in young patients have been described previously in the literature. Poiares Baptista et al., reported a case of EPC in 12-year-old patient with xeroderma pigmentosa [7] and Valverde et al., reported in an eight-year-old girl representing the youngest patient so far [2].
Robson et al., suggested 4 histopathological findings as prognostic factors in EPC patients. Lymphovascular invasion, depth of invasion >7mm, mitosis > 14/10 hpf and lymphnode involvement. The infiltrative growth pattern than pushing border is a prediction of local recurrence. Robson et al., presented the largest series of cases with a poor prognosis in 30% of patients experiencing lymphnode (20%) or distant metastases (10%) [8].
The present case displayed a tumour depth of 8mm with infiltrating borders, mitotic rate > 14/ 10 hpf, with few lymphatic tumour emboli and foci of tumour necrosis indicating poor prognosis for the patient.
Histopathologically, metastatic adenocarcinoma, trabecular carcinoma, merkel cell carcinoma, clear cell hidradenocarcinoma, basal cell carcinoma, squamous cell carcinoma, seborrheic keratosis, amelanotic melanoma and verruca vulgaris should be considered as some of the differential diagnoses [9]. Other distinct variety of sweat gland carcinoma includes chondroid syringoma, malignant dermal cylindroma, malignant syringoma, malignant acrospiroma, malignant trichoepithelioma and apocrine carcinoma. Nearly all sweat gland carcinomas exhibit immunoreactivity for CK, CEA and EMA. Ductal differentiation with formation of PAS positive cuticle is strong evidence against metastasis, squamous cell carcinoma and sebaceous cell carcinoma [1,10]. Glandular or acinar pattern in epidermis and dermis with hyperplasia of the overlying squamous epithelium is often seen in metastatic adenocarcinoma. Trabecular and merkel cell carcinoma exhibit trabecular pattern with classical nuclear features of fine granular chromatin, nuclear moulding, fragmentation and abundant mitosis which was lacking in our case. S100, NSE and CK 20 are positive in trabecular carcinoma. Porocarcinoma and hidradenocarcinoma have got many overlapping histologic features, hence distinguishing between the two if possible, is often difficult, especially when the tumours are not well differentiated [11].
In our case, the histopathological features, immunohistochemistry and special stain (PAS stain) helped us to arrive at the diagnosis.
Local excision with negative margins is the mainstay for treatment. If regional lymphnodes are involved then lymphadenectomy should be done. Perilesional injection of interferon alpha and interleukin 2 has been reported to produce a partial response. Da Silva also mentioned successful outcome with post op radiotherapy in recurrent cases [11,12].
Conclusion
The present case is being reported because of its rarity and occurring at a rare site, the right parieto occipital region in a young female patient. It is challenging to diagnose based on clinical presentation alone, hence histopathology along with immunohistochemistry are always the mainstay for early diagnosis and better treatment.
[1]. Choi SH, Kim YJ, Kim JH, Nam SH, Choi YW, A rare case of abdominal porocarcinomaArch plast surg 2014 41(1):91-93. [Google Scholar]
[2]. Gerber PA, Schulte KW, Ruzicka T, Bruch Gerharz D, Eccrine porocarcinoma of the head: An important differential diagnosis in the elderly patientDermatology 2008 216(3):229-33. [Google Scholar]
[3]. Chang O, Elnawawi A, Rimpel B, Asarian A, Chaudhry N, Eccrine porocarcinoma of the lower extremity: A case report and review of literatureWorld J Surg Oncol 2011 9:94 [Google Scholar]
[4]. HKS ALH Ramesh DB, Soni A. VR, Eccrine porocarcinoma: A case reportJ clin diagn res 2013 7(12):2966-67. [Google Scholar]
[5]. Rana RE, Verma SS, Puri VA, Baliarsing AS, Sweat gland tumour (Eccrine porocarcinoma) of scalp: A rare tumourIndian J plast surg 2005 38(1):51-53. [Google Scholar]
[6]. Ribeiro LC, Almeida M, Montenegro MG, Biasi LJ, Ogata DC, Eccrine porocarcinoma (Malignant eccrine poroma) with bone invasion and lymphnode metastasesApplied cancer research 2008 28(4):165-67. [Google Scholar]
[7]. Poiares Baptista, Tellechea O, Reis JP, Cunha MF, Fiqueiredo P, Eccrine porocarcinoma. A review of 24 casesAnn Dermatol venereal 1993 120:107-15. [Google Scholar]
[8]. Kurashige Y, Minemura T, Nagatani T, Eccrine porocarcinoma: Clinical and pathological report of eight casesCase Rep Dermatol 2013 5(3):259-66. [Google Scholar]
[9]. Vaidya KA, Shankarling M, Sukesh Eccrine porocarcinoma of skin: A rare case report with review of literatureSch J App Med Sci 2014 2(1):125-27. [Google Scholar]
[10]. Bindra A, Bhuva V, Jasani J, Chauhan S, Shukla R, Darad D, Ductal eccrine carcinoma- A sweat gland carcinoma with ductular differentiation- A case reportInt J Biol Med Res 2012 3(2):1862-64. [Google Scholar]
[11]. Brenn J, Mckee PH, Tumours of the surface epithelium. In: Mckee PH, Calonje E, Granter SR, editorsPathology of the skin with clinical correlations 2005 3rd edPhiladelphiaElsevier Mosby:1230-38. [Google Scholar]
[12]. Choi CM, Cho HR, Lew BL, Sim WY, Eccrine porocarcinoma presenting with unusual clinical manifestations: A case report and review of literatureAnn Dermatol 2011 23(1):79-83. [Google Scholar]