Accurate diagnosis of underlying dysfunctions by novice clinicians using conventional clinical tests is questionable. Amongst the recently recognized dysfunctions, dynamic instability, is important [10,11]. An optimum stability of Lumbar Motor Control (LMC) is important [12]. Deficits in dynamic stability may cause Motor Control Impairment (MCI) [13]. MCI is defined as a deficit in the control of movements during functional daily activities [14].
Studies have shown altered recruitment patterns of Transverse Abdominis (TrA) and Lumbar Multifidus (LMF) muscles in patients with LBP [15–20]. Assessing these altered patterns give an idea about the underlying dysfunctions [21]. Excessive relative flexibility at specific segments is a cause of many spine dysfunctions [14]. The provocative movements performed by patients underlie the pathomechanics of these dysfunctions [22,23]. These subjects show affected spinal stability, which underlies their pain disorder [20]. In recent years the assessment LMC in NSLBP has drawn tremendous attention [10].
This study proposes a new test - the ‘Back extension in standing’ for the assessment of MCI with passive extension pattern. This test is based on O’Sullivan’s definition for ‘passive extension pattern’ which is stated as, ‘MCI around the lumbar spine with a tendency to passively over-extend at the symptomatic segment of the lumbar spine’. The biomechanical basis of this test is to assess lack of motor control to extend the thoracolumbar spine with a tendency to hinge into extension [28]. A study has shown increased extension movement in patients with CLBP of extension subgroup [29].
It was hypothesized that the excessive excursion of the lumbar spine that occurs during the standing back extension test represents the inability of the stabilizers of the spine to control the movement of low back.
The reliability and validity of the test tool requires to be established within acceptable confidence limits before being accepted [25].
As per the currently available data, no test with appropriate psychometric properties has yet been established for detecting passive extension subgroup of MCI. The purpose of this study was to find the reliability and validity of the Standing Back Extension Test for lumbar spine. This study investigates whether a novice rater trained to perform the Standing Back Extension Test can diagnose MCI with reliability.
Materials and Methods
Setting: A case control study was conducted in tertiary health care teaching hospitals which represents one of the major healthcare treatment providers, for the duration of one year (April 2012 to March 2013).
The study protocol was approved by the Institutional Ethics Committee, Kasturba Medical College, Mangalore, Manipal University. The study is registered under Clinical Trial Registry of India. CTRI Registration Number: CTRI/2013/04/003555
Participants: Participants were selected through convenient sampling.
The sample size obtained was 50, using the formula
n= {2(Zα +Zβ)2+3}/C2, with 95% confidence interval and 80% power.
Inclusion Criteria: Participants for this investigation included men and women between 18-60 years of age.
For cases,
Inclusion criteria were current nonspecific low back pain (NSLBP) of musculoskeletal origin, diagnosed by the physician. NSLBP was defined as pain or discomfort between the 12th-rib costal margin and above the gluteal folds, with or without leg pain [30].
Exclusion criteria: Neurological involvement, prior lumbar surgery, history of acute trauma, pregnancy, spinal deformities like scoliosis, rheumatologic disorders, medical red flag conditions like unhealed fracture, tumour, systematic diseases [30,31] or current tremendous pain resulting in the inability to perform the test.
For controls
Inclusion criteria were absence of low back pain of any known or unknown origin.
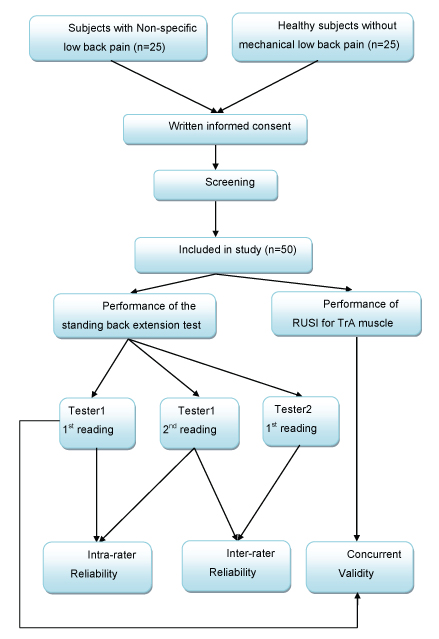
Exclusion criteria were same as for cases. Twenty-five healthy individuals without LBP were selected. Though previous studies [6,10] have shown presence of altered motor control in subjects with NSLBP, the cause of altered motor control is yet unknown. Hence to avoid selection bias 50% of cases and 50% of controls were selected in this study [Table/Fig-1].
Cases and controls were age and gender matched to avoid potential selection bias. Written informed consent was obtained from participants.
Testers: Two qualified physiotherapists pursuing the degree of Master of Physiotherapy in Orthopedics (Manual Therapy) conducted the study under the guidance of Associate Professors of the Physiotherapy Department representing physical therapists in clinical practice. A third physiotherapist, who was aware of participant’s group; recruited them after confirming eligibility the criteria.
Both the raters were blinded to the findings of other rater to avoid any influence in their test findings. Raters were blinded to their own prior findings of the test under evaluation. RUSI measurements of TrA muscle were performed by an experienced radiologist using Diagnostic ultrasound machine (GE Logic- 5, GE Voluson Expert- 730, Phillips Envisor, B- mode) to assess the thickness of TrA muscle.
Subjects were assessed involving two visits that were 24 to 48 hours apart, at the same time of the day to interfere with short term memory recall.
Raters were not blinded to the subject’s disease status, as practically it is difficult to not to have an idea about cases v/s controls; but were not aware about the underlying pathology, (i.e. if the altered motor control is underlying cause of NSLBP in cases). Also, it was evident from the quality of movement to identify subjects with LBP from healthy subjects. Raters were blinded to clinical information of results of Rehabilitative Ultrasound Imaging (RUSI). Raters also were blinded to additional cues that are not part of the test.
Order of examination was varied to avoid information bias or order effects. Time interval among repeated measures was appropriate to avoid recall bias [32–35]. The test was applied correctly and results interpreted appropriately
Procedure : The study was a repeated-measures design, involving two visits that were 24 to 48 hours apart, at the same time of the day. After signing consent forms, participants completed demographic details and self-reported measures.
An 11 point Numeric Pain Rating Scale (NPRS) was used to measure the intensity of current pain [36,37]. Oswestry Low Back Pain Disability Questionnaire (ODQ) was used to assess self-reported and performance-based disability [36]. After the completion of self-reported measures, the participants were asked to perform the Standing Back Extension Test.
All the participants (healthy and with NSLBP) were assessed by both the raters separately involving two visits that were 24 to 48 hours apart, at the same time of the day. Both the raters took two readings for each subject in two different visits.
Standing back extension test
Starting position: Standing with feet shoulder width apart. The subjects were asked to perform back extension in standing position. The instruction given was ‘stand with hands on the waist and bend backwards from your low back’. The test was considered ‘Negative’ if the horizontal excursion of Anterior Superior Iliac Spine (ASIS) was not excessive. The test was considered ‘Positive’ if the horizontal excursion of ASIS was excessive.
Rating protocol: As the subjects didn’t know the tests, only the clear movement dysfunction was rated as ‘Positive’. If the movement control improved by instruction and correction, it was considered that it did not infer a relevant movement dysfunction, as shown in [Table/Fig-2,3].
Lateral view of subject performing the standing back extension test. No excessive anterior horizontal excursion of ASIS with back extension is considered as ‘Negative’ test.

Lateral view of subject performing the standing back extension test. Excessive anterior horizontal excursion of ASIS with back extension, considered as ‘Positive’ test.

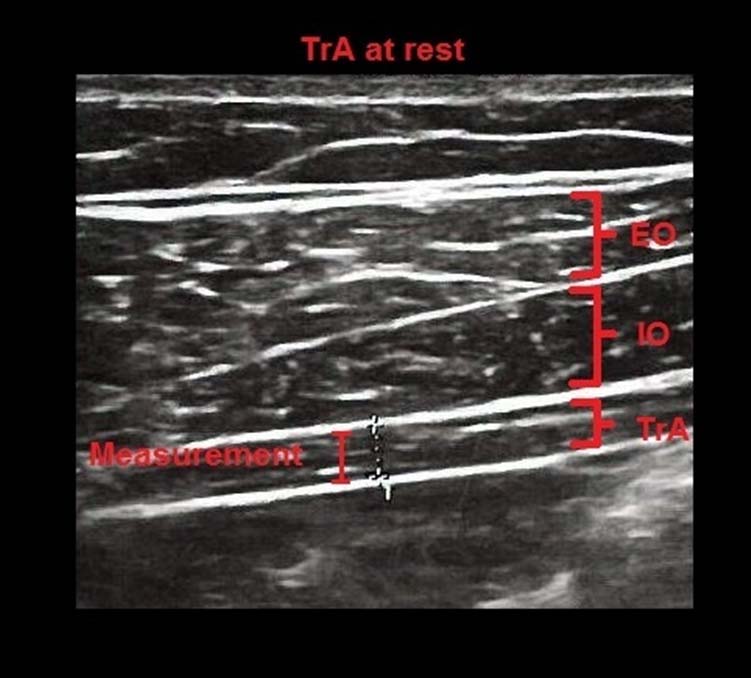
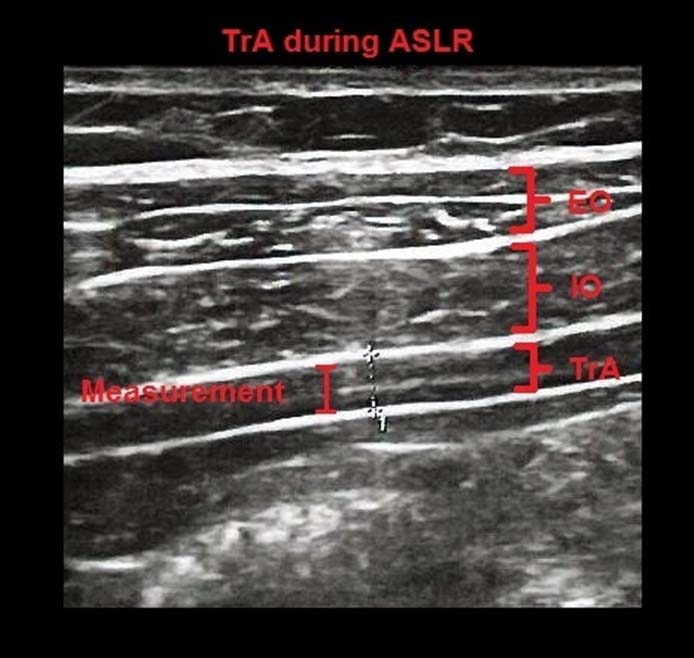
The thickness of TrA muscle was assessed with the help of RUSI using high frequency transducer 7-12 MHz, in B-mode. The subject was positioned in the supine hook-lying position with hips in 45% of flexion. Transducer head was placed along a line midway between inferior angle of the rib cage and the iliac crest. Images of the TrA muscle were acquired during the Active Straight Leg Raise (ASLR) maneuver and during the Abdominal Drawing-In Maneuver (ADIM) as shown in [Table/Fig-4,5 and 6].
Ultrasound images of the TrA, internal oblique (IO) and external oblique (EO) muscles during rest. Thickness measurements were made between the superficial and deep borders of the TrA muscle.
Ultrasound images of the TrA, internal oblique (IO) and external oblique (EO) muscles during ASLR (Active Straight Leg Raise). Thickness measurements were made between the superficial and deep borders of the TrA muscle.
Ultrasound images of the TrA, internal oblique (IO) and external oblique (EO) muscles during ADIM (Abdominal Drawing In Maneuver). Thickness measurements were made between the superficial and deep borders of the TrA muscle.
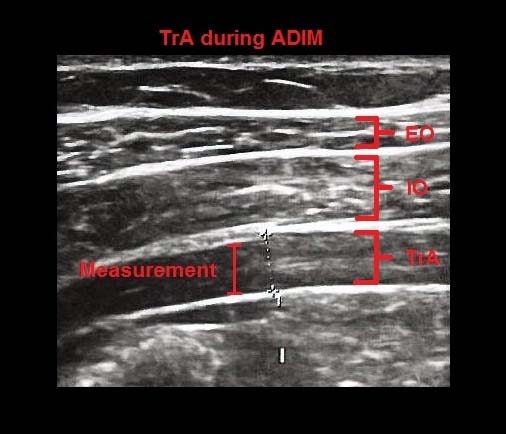
The ASLR maneuver was used to assess automatic changes in the TrA muscle thickness without the subject being asked to volitionally activate the muscle; whereas, the ADIM was used to assess changes in muscle thickness associated with a volitional activation of the TrA muscle [25]. There were no dropouts or missing data in this study.
Statistical Analysis
Statistical analyses were conducted using SPSS version 17.0 for Windows. Differences were considered statistically significant at p<0.05. The demographic and baseline characteristics of the two groups were analyzed using chi-square test. Standard Error of Measurement (SEM) and Minimal Detectable Changes (MDC) of the muscle thickness was calculated for current population using following formulae:
SEM = Standard deviation × √ (1-r), r = correlation coefficient.
MDC = SEM ×√2 × 1.96.
MDC for ASLR= 0.7 and for ADIM= 1.7; which were used as cutoff values. Subjects scoring difference in thickness less than cutoff were considered to suffer from impaired motor control.
For reliability: The reliability was assessed by the percentage agreement and by Cohen’s kappa. For intra-rater reliability, two findings taken at different times from the 1st rater were used. For inter-rater reliability, first finding from the 1st rater and finding from the second rater were used. The percentage agreement was calculated by dividing the numbers of agreed results with the total number of tests for each measured test.
For validity: To establish validity, results of movement test from 1st rater were compared with difference in thickness during ASLR and ADIM results. Receiver Operator Characteristic (ROC) curves was used for assessing the validity of the standing back extension test with respect to gold standard of ultrasound measurements during ADIM and ASLR maneuvers. Two by two contingency tables were constructed and sensitivity, specificity, positive and negative predictive values, and likelihood ratios with 95% Confidence Interval (CI) were calculated.
Results
The descriptive statistics of participants are tabulated in [Table/Fig-7]. There was no significant difference in age and gender between the two groups; but significant difference was seen in NPRS and ODQ. The standing back extension test showed very good intra-rater (k=0.87 with % agreement of 96%) and good inter rater (k=0.78 with % agreement of 94%) reliability. AUC for ADIM was 0.785 and for ASLR was 0.780. [Table/Fig-8] presents sensitivity, specificity, positive and negative predictive values and likelihood ratios for the standing back extension test.
Demographic and baseline characteristics of participants.
| Characteristics | Cases | Controls | Significant difference |
|---|
| N | 25 | 25 | |
| Age (years) | 33.52 ± 9.33 | 32.6 ± 8.74 | p= 0.774 ns |
| Female % | 52% | 52% | p= 0.084 ns |
| NPRS (pain intensity) | 4.638 ± 1.091 | | |
| Oswestry LBP DQS | 29.106 ± 7.940 | | |
| Duration of pain (in days) | 653.234 ± 69.17 | | |
N: Number of subjects; NPRS: Numerical Pain Rating Scale; Oswestry LBP DQS: Oswestry Low Back Pain Disability Questionnaire Score; p: significance level; ns: not significant at p<0.05
Validity of the standing back extension test.
| Property | ASLR | 95% CI | ADIM | 95% CI |
|---|
| Sensitivity | 34.62% | 17.25- 55.66% | 43.75% | 19.83- 70.08% |
| Specificity | 95.83% | 78.81- 99.30% | 94.12% | 80.29- 99.11% |
| Positive likelihood ratio | 8.31 | 1.14- 60.78 | 7.44 | 1.74- 31.86 |
| Negative likelihood ratio | 0.68 | 0.51- 0.91 | 0.60 | 0.38- 0.93 |
| Positive predictive value | 90% | 55.46- 98.34% | 77.78% | 40.06- 96.53% |
| Negative predictive value | 57.50% | 40.89- 72.95% | 78.05% | 62.38- 89.42% |
ASLR: Active Straight Leg Raise; ADIM: Abdominal Drawing In Maneuver; LMF: Lumbar Multifidus; CI: Confidence Interval
Discussion
The aim of this study was to establish intra and inter-rater reliability and concurrent validity of the standing back extension test. This study introduced a new test for stratifying passive extension subgroup for MCI in subjects with NSLBP which was never used before in any other study for assessment of motor control. The standing back extension test used in this study was selected as per O’sullivan’s classification for subgroups of MCI [17,28,37].
As per our knowledge, this is the first study that establishes reliability and concurrent validity of a movement control test, for detecting passive extension subgroup of MCI in patients with NSLBP. Also, this is the first study that uses clinical and ultrasound measures to demonstrate a clear difference between patients with NSLBP and healthy individuals regarding their ability to actively control the movements of the low back during the movements of trunk and lower extremities.
Reliability: As the test was rated dichotomously in this study; to establish reliability, k statistics were used which has gained widespread acceptance as a measure of reliability as it takes into consideration for the role of chance in dichotomous agreement [38,39].
This test showed very good intra-rater (k=0.87 with % agreement of 96%) and good inter-rater (k=0.78 with % agreement of 94%) reliability which could be attributed to the similar levels of experience and knowledge, training and understanding about the MCI in both the testers, leading to parallel clinical reasoning and decision making.
Validity: In this study, to establish concurrent validity; difference in thickness of TrA muscle was used as a criterion measure to assess altered motor control of lumbar spine which was measured using RUSI. TrA muscle was selected for assessment in spinal stability because of the important role it plays by acting in a feed forward manner, which is essential for dynamic functional stability during extremity movements [40,41] also because of its anatomical and biomechanical orientation which enables it to control the eccentric extension of the lumbar spine [31]. Also, various studies have suggested that the TrA muscle may be important for normal motor control of lumbar movement [33].
For TrA, difference in the thickness of muscle was assessed during two maneuvers: ASLR and ADIM. The ADIM was used to assess changes in muscle thickness associated with a volitional activation of the TrA muscle, whereas the ASLR maneuver was used to assess automatic changes in the TrA muscle thickness without the subject being asked to volitionally activate the muscle [25].
RUSI which was used in this study to assess the difference in the thickness of TrA is a noninvasive tool and is a reliable and valid measurement of abdominal muscle recruitment in LBP patients and has acceptable association with the gold standard electromyography (EMG) and magnetic resonance imaging (MRI) [35].
RUSI is an alternative approach to measure the recruitment of the muscles indirectly by assessment of morphologic changes of the muscles (i.e. thickness changes) [34]. It directly assesses the changes in muscle geometry [35]. RUSI observes changes in muscle thickness during the ADIM and ASLR movements, which are considered to be indicators of muscle activation [34,35].
The passive extension pattern showed high validity to TrA measure of ultrasound probably owing to the forces produced on lumbar spine during the standing back extension test, as standing back extension test puts stress on lumbar spine in the direction of extension. Inability to control the amount of extension is considered as altered motor control.
According to previous studies, the horizontal orientation of lower fibers of TrA, contributes to the enhancement of the stability of the spine by either increasing the intra abdominal pressure or the tension in thoracolumbar fascia through its attachment to the lumbar vertebrae. Both the mechanisms enhance the stiffness of the spine by which TrA may contribute in controlling the stability [35]. This study meets 10 out of 11 items of Quality Appraisal of Diagnostic Reliability [42].
Effects of Body Mass Index (BMI) on the thickness of abdominal muscles were not considered in this study, as the positive association between BMI and TrA muscle thickness at rest and on contraction had been demonstrated in the previous study [43]. Effects of chronicity of LBP on MCI and on TrA muscle thickness are unknown. The effect of chronicity of pain on MCI was not considered in this study. Since the current study is a reliability and validity study, the results are not influenced by these factors. Further limitations were the narrow age group and the use of only 2 novice testers. A previous study has demonstrated, experienced testers demonstrate better inter-rater reliability than novice raters [6].
This study provides a reliable and valid test for passive extension subgroup of MCI which can be easily administered in clinical practice without any equipment. It will help to diagnose impaired motor control of lumbar spine and categorize it into the passive extension subgroup as per O’sullivan’s classification. Findings on reliability have clear clinical implications. In a clinical practice it is necessary to have consistency in assessing and recording the data so as to guarantee its efficient use when it is recorded/used by novice therapists. However, the study does not rule out the fact that future validity studies should be done on populations with larger age groups, considering their BMI in different populations and using different levels of experience raters, that is, novices and experts.
Conclusion
The present study has shown very good intra-rater and good inter-rater reliability for the standing back extension test. The study has also established the concurrent validity for the Standing Back Extension Test.
N: Number of subjects; NPRS: Numerical Pain Rating Scale; Oswestry LBP DQS: Oswestry Low Back Pain Disability Questionnaire Score; p: significance level; ns: not significant at p<0.05
ASLR: Active Straight Leg Raise; ADIM: Abdominal Drawing In Maneuver; LMF: Lumbar Multifidus; CI: Confidence Interval