Intralesional Sclerotherapy - A Novel Approach for The Treatment of Intraoral Haemangiomas
G.Siva Prasad Reddy1, G. Venkateshwara Reddy2, K. Sravan Kumar Reddy3, B. Srilatha Priyadarshini4, P. Karuna Sree5
1 Professor, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental sciences, Hyderabad, Telangana, India.
2 Professor and Head, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental sciences, Hyderabad, Telangana, India.
3 Post Graduate Student, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental sciences, Hyderabad, Telangana, India.
4 Post Graduate Student, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental sciences, Hyderabad, Telangana, India.
5 Post Graduate Student, Department of Oral and Maxillofacial Surgery, Panineeya Institute of Dental sciences, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K. Sravan Kumar Reddy, Post-Graduate Student, Department of Oral and Maxollofacial Surgery, Panineeya Mahavidyalaya Institute of Dental Sciences, Kamalanagar, Chaitanyapuri, Hyderabad-500060, India. E-mail : sravankothuru@gmail.com
In infancy and childhood haemangiomas are the most common neoplasms in head and neck region with an occurrence of about 60%. Approximately 40%-50% of all haemangiomas resolve incompletely, leaving permanent changes in the skin, such as telangiectases, epidermal atrophy, hypopigmentation or redundant skin with fibro-fatty residue but a few stubborn, problematic haemangiomas may result in serious disfigurement and dysfunction, and even become life-threatening. Most haemangiomas are managed by conservative methods that include corticosteroids (either systemic or local injection), sclerotherapy, interferon-alpha, laser therapy, embolization, cryotherapy, and radiation. Due to risk of haemorrhaging, surgical removal for small vascular lesions is not considered and it is more invasive than sclerotherapy. This case report presents the efficacy of intralesional sclerotherapy for the management of haemangiomas on dorsum and lateral border of tongue.
Sodium tetra decyl sulphate, Sclerosing agent, Vascular lesions
Case Report
A 24-year-old female patient was referred to the Department of Oral and Maxillofacial Surgery of Panineenya dental college of Hyderabad, with a chief complaint of a bluish coloured swelling on the lateral aspect of tongue since 10 years. Patient gave history of the swelling which began as a peanut size on the tongue which gradually progressed to present size.
Clinical examination revealed a round shaped bluish coloured swelling measuring about 1 cm in diameter present on left dorsum and lateral border of tongue [Table/Fig-1]. It was non tender on palpation, soft to firm in consistency and without any pus discharge or bleeding associated with it. The swelling was compressible and blanched on application of pressure.
Intra oral photograph showing an elevated purple-blue swelling on dorsum and lateral border of the tongue.

All the haematological investigations were within normal limits. Considering the age of the patient, size and extent of the lesion, to reduce surgical morbidity and to eliminate need for the hospitalization and general anaesthesia, it was planned to treat the patient with intralesional sclerotherapy with sodium tetra decylsulphate [Table/Fig-2] under local anaesthesia. Under aseptic conditions, 1ml of intralesional sclerosing agent (sodium tetra decylsulphate, with trade name of SETROL) was injected intralesionally in a circumferential manner around the lesion [Table/Fig-3]. Patient was kept on course of antibiotics and analgesics and advised to use chlorhexidine mouth wash.
Injection of 1 mL of sodium tetra decylsulphate in circumferential manner.

Regular follow-up’s were done at 24 hrs [Table/Fig-4], 15 days [Table/Fig-5] and at weekly intervals upto one month [Table/Fig-6] and at six months. No complications were noted except for oedema of tongue and slight discharge from the same site on 7th day of follow-up. The lesion had virtually disappeared and no further injections were necessary. The patient was asymptomatic since then without any complaints. At the 6 months follow-up examination there was no evidence of recurrence [Table/Fig-7].
Gross oedema of dorsum and lateral border of the tongue 24 hours after injection.

Reduction in inflammation and oedema at 15th day follow-up.

Break down of the lesion and healing ulcer at one month follow-up.

Six months follow-up photograph showing normal architecture of the tongue.

Discussion
Haemangiomas and vascular malformations are two major congenital vascular lesions [1]. In infancy and childhood haemangiomas are the most common neoplasms in head and neck region. Tongue and floor of the mouth are common sites in oral cavity [2]. Infantile and congenital are two different types of haemangiomas [3]. The haemangioma could be congenital or traumatic in origin and a benign tumour of patent blood vessels, formed by an increased number of blood vessels with prevalence of 0.8% in the tongue region [4].
Haemangiomas are clinically presented as sessile or pedunculated, soft, flat or raised, painless, smooth or irregular in outline and blanching of tumour on application of pressure [5]. The different modalities included for the treatment of haemangiomas, are sclerotherapy, cryotherapy, isotope radiotherapy, electrocoagulation, laser therapy, and surgical therapy [4]. Multidisciplinary management is often needed for best efficacy. In treatment of haemangiomas due to scarring or hyper-pigmentation, skin atrophy, due to high cost and slight depression of the skin, laser and cryotherapy are not commonly used [6,7].
In haemangiomas as the line of treatment surgical intervention is the last choice due to intraoperative bleeding, postoperative scarring, incomplete excision, recurrence, functional impairment and surgical morbidity [8,9].
Sodium tetra decylsulphate, sodium morrhuate, bleomycin. Sodium psylliate are commonly used sclerosing agents in treatment of haemangiomas [10]. Some of these drugs occasionally cause local discomfort and allergic reactions in the oral haemangioma cases. The mechanism of action of sclerotherapy is depicted in [Table/Fig-8]. Necrosis and sloughing of the tissue have been reported when the sclerosing agent was used superficially. Total or partial regression can be seen by injecting sclerosing agents. The exophytic scar tissue is surgically removed in case of partial regression.
Flow chart showing the mechanism of action of sclerotherapy [15].
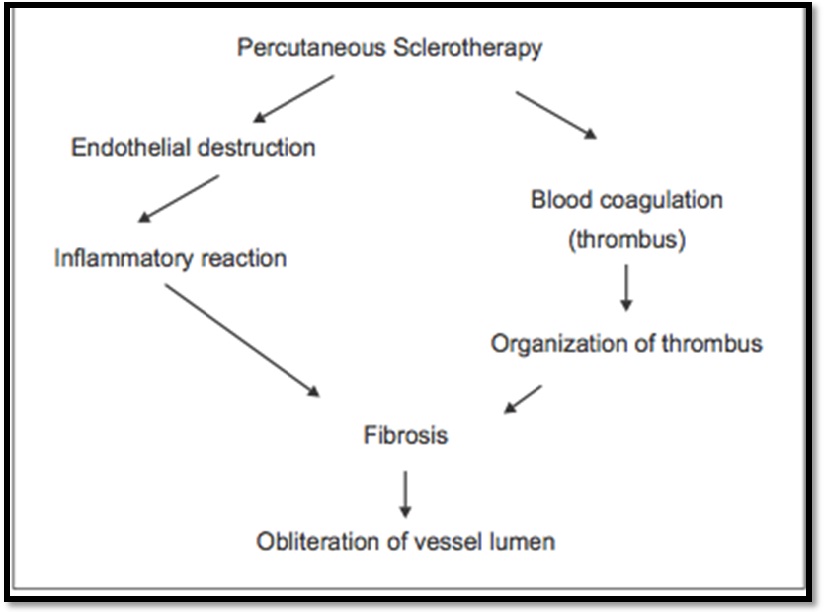
For the treatment of benign vascular lesions sclerotherapy is an effective and conservative method and it is non invasive, low cost technique and there is low risk of haemorrhaging [11,12]. When injected into or adjacent to blood vessels the sclerosing agent causes vascular thrombosis, endothelial damage, leading to endofibrosis and vascular obliteration [13]. The advantages of sodium tetra decylsulphate are absence of pain, no haemolysis, less hyperpigmentation, complete regression of low vascular lesions and very low incidence of allergic reactions [14].
Concusion
Considering the risks and benefits of the various treatment modalities and depending on the anatomic location, size and growth pattern we have choosen sclerotherary as the choice of treatment. Sclerotherapy is a simple, safe, and effective procedure with minimal complications for small and uncomplicated intraoral haemangiomas.
[1]. Sung MW, Bleomycin sclerotherapy in patients with congenital lymphatic malformation in the head and neckAmerican Journal of Otolaryngology 1995 16(4):236-41. [Google Scholar]
[2]. Hibbert J, Oral cavity. In: Hibbert J, editorScott- Brown’s Otolaryngology and head and neck surgery 1997 5:1-32. [Google Scholar]
[3]. Mulliken JB, Enjolras O, Congenital haemangiomas and infantile haemangioma: missing linksJ Am Acad Dermatol 2004 50(6):875-82. [Google Scholar]
[4]. Kukde MM, Haemangioma of tongue: a conservative approach by sclerotherapy- a case reportInt J Biol Med Res 2015 6(2):4981-83. [Google Scholar]
[5]. Aitha H, Kubbi JR, Gantala R, Korvipati NK, Sclerotherapy: A conservative approach in the treatment of oral haemangiomasJ Indian Acad Oral Med Radiol 2015 27:291-93. [Google Scholar]
[6]. Kaplan I, Gassner S, Shindel Y, Carbon dioxide laser in head and neck surgeryAm J Surg 1974 128:543-44. [Google Scholar]
[7]. Imai T, Matsuo N, Yamashita T, Two cases of haemangioma of the upper lip in infants—treatment using the Nd: YAG laserAichi Gakuin Dent Sci 1991 4:35-44. [Google Scholar]
[8]. Selim H, Use of sclerosing agent in the management of oral and perioral haemangiomas: review and case reportsMed SciMonit 2007 13(9):CS114-19. [Google Scholar]
[9]. Govrin-Yehudain J, Moscona AR, Calderon N, Hirshowitz B, Treatment of haemangioma by sclerosing agents: an experimental and clinical studyAnnal Plast Surg 1987 18:465-69. [Google Scholar]
[10]. Agarwal S, Treatment of oral haemangioma with 3% sodium tetradecyl sulfate: study of 20 casesIndian J Otolaryngol Head Neck Surg 2012 64(3):205-07. [Google Scholar]
[11]. Gitelman JM, Malkin M, Travin MS, Haemangioma of the lip: combined treatmentN Y State Dent J 1976 42:420-22. [Google Scholar]
[12]. Iso MA, Kitano S, Iwanga T, A prospective randomized study com- paring the effects of large and small volumes of the sclerosant 5% eth- anolamineoleate injected into esophageal varicesEndoscopy 1988 20:285-88. [Google Scholar]
[13]. Croffie J, Somogyi L, Chuttani R, DiSario J, Liu J, Mishkin D, Technology assessment committee. sclerosing agents for use in GI endoscopyGastrointest Endosc 2007 66:1-6. [Google Scholar]
[14]. Dietzek CL, Sclerotherapy: introduction to solutions and techniquesPerspect Vasc Surg EndovascTher 2007 19:317-24. [Google Scholar]
[15]. Saraf S, Sodium tetradecyl sulfate in venous malformationsIndian J Dermatol 2006 51(4):258-61. [Google Scholar]