Age-Related Normogram for Ovarian Antral Follicle Count in Women with Polycystic Ovary Syndrome and Comparison with Age Matched Controls Using Magnetic Resonance Imaging
Senthil Kumar Aiyappan1, Bulabai Karpagam2, V. Vadanika3, Prem Kumar Chidambaram4, S. Vinayagam5, K.C Saravanan6
1 Associate Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
2 Associate Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
3 Junior Resident, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
4 Assistant Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
5 Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
6 Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Senthil Kumar Aiyappan, Associate Professor, Department of Radiodiagnosis, SRM Medical College Hospital and Research Centre, SRM Nagar, Potheri, Kattankulathur, Kancheepuram, Tamilnadu-603203, India. E-mail : senthilkumarpgi@yahoo.co.in
Introduction
Antral Follicle count (AFC) is a reliable marker for ovarian reserve. Previous studies have used transvaginal ultrasound for estimation of AFC, however we used magnetic resonance imaging (MRI) for estimation of AFC and for creating an age-related normogram in patients with polycystic ovary syndrome (PCOS) and compared it with normal patients.
Aim
The aim of this study is to create an age related normogram for AFC in women with PCOS and to compare that with women without polycystic ovarian syndrome using MRI.
Materials and Methods
A total of 1500 women were examined, out of which 400 fitted the criteria for PCOS. They all underwent MRI study and similar age matched women without PCOS also underwent MRI examination. Normogram for AFC were obtained using LMS software and a percentile chart was obtained.
Results
Normogram for AFC in PCOS women showed decline in number of AFC as the age progresses and the decline was linear. The normogram for AFC was compared with equal number of patients without PCOS and they also showed decline in AFC as the age progresses, however the decline was exponential and faster.
Conclusion
Age related normogram for AFC is widely used and considered as best clinical predictor for ovarian response in assisted reproductive technology. Knowledge of ovarian reserve is important in PCOS and non-PCOS females as PCOS patients are at risk for ovarian hyperstimulation syndrome during gonadotrophin theraphy. MRI is an equally effective and in some times better alternative to transvaginal ultrasound as it has got its own advantages.
Assisted reproductive technology, Ovarian reserve, Ovarian hyperstimulation syndrome, Transvaginal ultrasound
Introduction
Polycystic ovarian syndrome (PCOS) is a common endocrine disorder characterized by a variety of symptoms like hyperandrogenism, hyperinsulinaemia, menstrual dysfunction, unique ultrasonographic ovarian pattern and infertility [1]. Antral Follicle count (AFC) has been found to be reliable marker for ovarian reserve [2]. Since women with PCOS are extremely sensitive to gonadotrophin stimulation, knowledge of age related AFC normogram is clinically relevant. Wiser et al., published age- related normogram for AFC in women with PCOS using transvaginal ultrasound and found that the decline in number of AFC as the age progresses was linear and slower in PCOS when compared to infertile women without PCOS [2]. We used magnetic resonance imaging (MRI) instead of TVS, since MRI can acquire three dimensional images, not operator dependant and also it can be performed in patients for whom transvaginal ultrasound could not be performed like in unmarried women. The main objective of our study is to create an age related normogram for AFC (AFC) in women with PCOS and to compare that with women without polycystic ovarian syndrome using MRI.
Materials and Methods
This descriptive cross-sectional study was conducted after obtaining clearance from Institutional Ethics Committee between January 2013 to July 2015. The goal of the study was to create an age related normogram of AFC in women with PCOS and to compare it with those without PCOS using MRI. Women between the ages of 18 to 45 were included in the study. A total of 1500 women were examined, out of which 400 fitted the criteria for PCOS. PCOS was defined using the Rotterdam criteria of ESHRE/ASRM for PCOS [3] (Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group, 2004) which included two out of three of the following: (i) oligo- or anovulation; (ii) clinical and/or biochemical signs of hyperandrogenism; and (iii) polycystic ovaries (presence of 12 or more follicles in each ovary measuring 2–9 mm). Exclusion criteria included were: (i) patients with any other ovarian pathology; (ii) Patients on hormonal therapy; and (iii) patients who have metallic implants /cardiac pacemakers or any other contraindications for MRI. Similar number of age matched patients without PCOS were also examined using similar protocol. Study was done in Siemens 1.5 Tesla magnetom Essenza MRI machine. MRI was done free of cost in our institution. AFC and follicle size were assessed in both the ovaries in T2 FS axial, sagittal images. The central ovarian stroma was assessed with T1 axial, T2 coronal and axial sequences. All participants who were included in the study gave oral and written consent and the study was done in the follicular phase of the menstrual cycle. Follicular size was measured using the internal diameters of the ovary. Total number of follicles in both ovaries was taken as AFC [Table/Fig-1]. The age, height, parity and weight of the patients were recorded, including the hormonal analysis (LH and FSH) wherever available. The data was entered into an Excel sheet and analyzed using LMS software.
Coronal MRI image showing both ovaries with multiple follicles (white arrows). AFC was calculated by counting the total number of follicles in each ovary.

Results
Normograms of the percentiles of AFC for each age group were created using the lambda-mu-sigma (LMS) method. The LMS method uses three eponymous parameters to model the data – lambda (skew), mu (median) and sigma (coefficient of variation) and it models the change of each parameter with respect to the independent variable (age). The data modelled using patient identification number (ID) as a random effect, age as the independent variable, and the dependent variable AFC transformed to normality via log (AFC+1). The data were fitted to the 3rd, 10th, 25th, 50th, 75th, 90th and 97th percentiles.
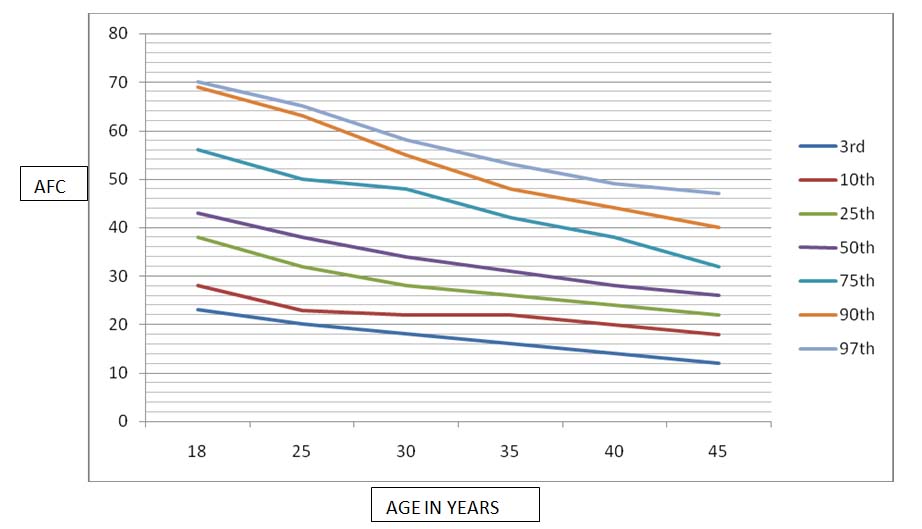
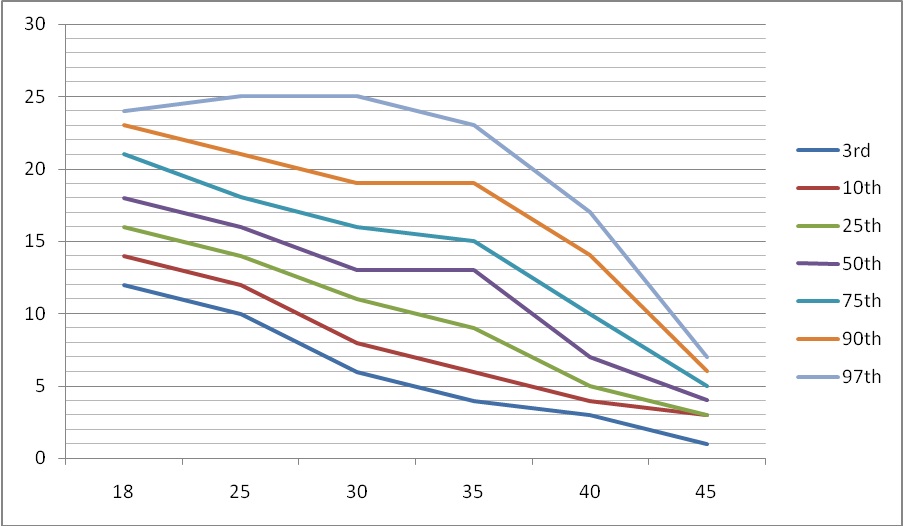
A total of 400 women fitted the criteria for PCOS. [Table/Fig-2] shows the age group of patients with PCOS. Most of them were under 35 years and only 5% of patients were above 40 years. [Table/Fig-3] shows the age-related normogram for patients with PCOS and [Table/Fig-4] shows the age related normogram for patients without PCOS. Out of 400 patients examined in non-PCOS group, 50 patients were infertile and 60 patients were unmarried. The pattern of decrease of AFC among women with PCOS was linear; while in those without PCOS, it was exponential until 32 to 34 years of age, and then became similar to that of PCOS. The rate of follicle loss per year was slower in PCOS women compared with that in non-PCOS women at any age (p < 0.001). In both groups of patients, the fastest period of follicle loss was between the ages 18–35 years. Women with PCOS had a high number of antral follicles in each ovary. The current study found large variations in the AFC between the 10th and 90th percentiles.
Showing no. of patients with PCOS Vs Age.
| GE group | No of Patients with PCOS |
|---|
| 18-25 | 156 |
| 26-30 | 104 |
| 31-35 | 60 |
| 36-40 | 60 |
| 40-45 | 20 |
| Total | 400 |
Showing age related normogram for PCOS patients using MRI.
Showing age related normogram for Non-PCOS patients using MRI.
Discussion
With MRI, it is possible to count antral follicles down to 1 mm in size and precise three-dimensional (3D) volume estimations of ovaries independent of nonellipsoid ovarian shape measurement errors can be done [4–6]. MRI is an excellent modality for imaging ovaries with high-contrast resolution [6]. Studies using MRI alone for derivation of age related normogram for AFC in patients with and without PCOS are rare [5–7]. AFC is considered one of the reliable markers for evaluation of ovarian reserve [8,9]. The number of antral follicles and the total ovarian volume as measured by transvaginal USG predict declining fertility related to reproductive aging. AFC has the closest association with chronological age and is lower in infertile women than in matched controls. The baseline and cut-off values in Indian women are lower than that mentioned in the Western literature [8]. Because of high predictive value and low cost, AFC is widely used and is considered best clinical predictor for ovarian response in assisted reproductive technology [9–13]. AFC correlates negatively with age [7]. A percentile normogram will be useful to inform a woman about her ovarian reserve relative to her age group [7]. The ovarian reserve decline rate relative to age group is important because of the declining fertility with increasing age [7].
Knowledge of the age-related AFC normogram in women with PCOS is important, since they are at risk of ovarian hyperstimulation syndrome during treatment [14,15]. In this study, we try to establish the role of MRI in evaluation of AFC. In our study, the age-related normogram for the 3rd, 10th, 25th, 50th, 75th, 90th, and 97th percentile of AFC in patients without PCOS showed a biphasic mode of decline with two different rates of AFC loss: a steep-slope and a moderate-slope phase while that with PCOS showed linear slope indicating that the rate of follicle loss is less in PCOS women at any age. Various theories which have been described for the linear slope in PCOS are presence of more primordial follicles to start with in the polycystic than in the normal ovary, reduced loss of follicles by atresia during folliculogenesis; and the rate of progression through the various stages of follicle development are different between normal and polycystic ovaries [16]. Our study is correlating with the previous studies done by Wiser A et al., and Almog B et al., however our study is done using MRI alone [2,9]. The advantage of MRI includes three dimensional imaging, accurate ovarian volume measurement, good reproducibility and inter-observer agreement [6] and it can be done even in unmarried patients unlike transvaginal ultrasound. The limitations of MRI include cost, availability and it cannot be done in claustrophobic patients and patients with metallic implants. The results of this study are similar to other studies done using transvaginal ultrasound. Hence this study proves the fact that MRI is an equally effective method for assessing AFC, although it is expensive.
Conclusion
Age related normogram for AFC is widely used and considered as best clinical predictor for ovarian response in assisted reproductive technology. Knowledge of ovarian reserve is important in PCOS and non-PCOS females as PCOS patients are at risk for ovarian hyperstimulation syndrome during gonadotrophin theraphy. MRI is an equally effective and in some times better alternative to transvaginal ultrasound as it has got its own advantages. This study re-establishes the fact that age related decline in AFC among women with PCOS is slower than those without PCOS and the decline is linear.
[1]. Tsikouras P, Spyros L, Manav B, Zervoudis S, Poiana C, Nikolaos T, Features of PCOS in adolescenceJ Med Life 2015 8(3):291-96. [Google Scholar]
[2]. Wiser A, Shalom-Paz E, Hyman JH, Sokal-Arnon T, Bantan N, Holzer H, Age-related normogram for AFC in women with PCOSReprod Biomed Online 2013 27(4):414-18. [Google Scholar]
[3]. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop GroupRevised 2003 consensus on diagnostic criteria and long-term health risks related to PCOS (pcos)Hum Reprod 2004 19:41-47. [Google Scholar]
[4]. Brown M, Park AS, Shayya RF, Wolfson T, Su HI, Chang RJ, Ovarian imaging by magnetic resonance in adolescent girls with PCOS and age-matched controlsJ Magn Reson Imaging 2013 38(3):689-93. [Google Scholar]
[5]. Leonhardt H, Hellström M, Gull B, Lind AK, Nilsson L, Janson PO, Stener-Victorin E, Ovarian morphology assessed by MRI in women with and without PCOS and associations with antimüllerian hormone, free testosterone, and glucose disposal rateFertil Steril 2014 101(6):1747-56.e1-3. [Google Scholar]
[6]. Leonhardt H, Gull B, Stener-Victorin E, Hellström M, Ovarian volume and AFC assessed by MRI and transvaginal ultrasonography: a methodological studyActa Radiol 2014 55(2):248-56. [Google Scholar]
[7]. Yoo RY, Sirlin CB, Gottschalk M, Chang RJ, Ovarian imaging by magnetic resonance in obese adolescent girls with PCOS: a pilot studyFertil Steril 2005 84(4):985-95. [Google Scholar]
[8]. Agarwal A, Verma A, Agarwal S, Shukla RC, Jain M, Srivastava A, AFC in normal (fertility-proven) and infertile Indian womenIndian J Radiol Imaging 2014 24(3):297-302. [Google Scholar]
[9]. Almog B, Shehata MB, Shalom-Paz E, Tan SL, Tulandi T, Age related normogram for AFC: McGill reference guideFertil Steril 2011 95(2):663-66. [Google Scholar]
[10]. de Carvalho BR, Rosa e Silva AC, Rosa e Silva JC, dos Reis RM, Ferriani RA, Silva de Sá MF, Ovarian reserve evaluation: state of the artJ Assist Reprod Genet 2008 25(7):311-22. [Google Scholar]
[11]. Ferraretti AP, Lappi M, Magli MC, Muzzonigro F, Resta S, Gianaroli L, Factors affecting thawed oocyte viability suggest a customized policy of embryo transferFertil Steril 2010 94(4):1308-13. [Google Scholar]
[12]. Hendriks DJ, Broekmans FJ, Bancsi LF, Looman CW, de Jong FH, te Velde ER, Single and repeated GnRH agonist stimulation tests compared with basal markers of ovarian reserve in the prediction of outcome in IVFJ Assist Reprod Genet 2005 22(2):65-73. [Google Scholar]
[13]. Magli MC, Lappi M, Ferraretti AP, Capoti A, Ruberti A, Gianaroli L, Impact of oocyte cryopreservation on embryo developmentFertil Steril 2010 93(2):510-16. [Google Scholar]
[14]. O’Neill KE, Senapati S, Dokras A, Use of gonadotropin-releasing hormone agonist trigger during in vitro fertilization is associated with similar endocrine profiles and oocyte measures in women with and without PCOSFertil Steril 2015 103(1):264-69. [Google Scholar]
[15]. Das M, Son WY, Buckett W, Tulandi T, Holzer H, In-vitro maturation versus IVF with GnRH antagonist for women with PCOS: treatment outcome and rates of ovarian hyperstimulation syndromeReprod Biomed Online 2014 29(5):545-51. [Google Scholar]
[16]. Webber LJ, Stubbs S, Stark J, Trew GH, Margara R, Hardy K, Franks S, Formation and early development of follicles in the polycystic ovaryLancet 2003 362(9389):1017-21. [Google Scholar]