Introduction
Unsafe injection can transmit many diseases to patients, injection providers and healthy people of community.
Aim
To find out critical steps whether executed according to recommended best practice methods, availability of equipments in health facilities for safe injection practices and some important steps of waste disposal methods.
Materials and Methods
This facility-based cross-sectional observational study was conducted among 30 Auxiliary nurse midwives (ANM) & 27 nursing staffs (NS) to assess certain aspects of their practice while administrating injection and disposal of the disposables. Health facilities were also observed to asses necessary equipments of safe injection and waste disposal methods.
Results
Among the health workers 93.3% ANM and 100% NS took sterile syringe from sterile unopened packet, all of the study subjects washed hand before giving injection, 13.3% of ANMs and 8% of NS are fully vaccinated against Hep B, 53.3% of ANM and all NS are practices non recapping. Only 13.33% sub centres along with PHC & BPHC had at least one puncture resistant leak proof container, 86.7% sub centres, PHC are free from loose needles. Transport for off side treatment is the method of waste disposal in case of 73.3% cases sub centres, PHC & BPHC.
Conclusion
There is need to educate, train and motivate service providers in proper methods of giving injection along with improve the adequacy of supply of required equipments.
Introduction
Injection is an important drug delivery system especially for severely ill patient, acute emergency condition and immunisation. But this can spread disease to patient, health workers, waste handlers and even in common healthy people if not used and disposed in proper way [1].
A safe injection is one that, does not harm the recipient (patient), does not expose the provider (Health Workers) to any avoidable risk and does not result in waste that is dangerous for the community [1], so safe injection practice involves administration of rational injection by a well trained, qualified person using sterile syringe, needle, adopting sterile technique, and disposing the used ones in a puncture-proof container. Any breach in the process makes the injections extremely unsafe and hazardous to Health workers (HWs) as well recipients.
Common infectious agent’s are- HBV, HIV, HCV, some bacterial infection, which create a major problem related to unsafe injection practice. These viruses can remain “silent” in the body for a long time before they cause symptoms. Thus, unsafe injections can lead to a silent epidemic that occurs many years after the original events [2].
The global burden of disease, due to unsafe injection use, estimated by the World Health Organization (WHO) by probability model for the year 2008 was 340,000 Human Immunodeficiency Virus (HIV) infections, 15 million Hepatitis B Virus (HBV) infections, 1 million Hepatitis C Virus (HCV) infections, 3 million bacterial infections and 850,000 injection site infections. This accounted for 14% of HIV, 25% HBV, 8% HCV and 5% of bacterial infections worldwide and for 28 million preventable disability adjusted life years” [3].
WHO has estimated that interventions implemented in 2000 for the safe and appropriate use of injections would have cost $102 per year of life saved (adjusted for disability) [4].
The INCLEN (International Clinical Epidemiology Network) report of Assessment of Injection Practices in India (2004), found that approximately 6 billion injections are given in this country every year; however it has also been reported by industries that only 3 billion syringes are actually manufactured. This clearly spells out the huge magnitude of reuse of syringes in India [5]. A study by Kotwal et al., showed that only 22.5% of injections were administered with a sterile syringe and needle in the metropolitan cities of North India [6].
In a study done in a tertiary hospital of West Bengal on nursing staff showed that, 60% of the nursing personnel maintained correct procedure during giving injection; while sterile gloves are used by only 3.7% nurses [7].
Proper disposal of waste that generated after injection is another important issue. According to Biomedical Waste (Management and Handling) Rules 1998, needles, syringes should disposed by disinfection (chemical treatment/autoclaving /micro-waving and mutilation /shredding) [8]. Government of India has made a provision for treating biomedical waste at outside the health facilities through Common Bio-medical Waste Treatment & Disposal Facility (CBMWTDF) with the collaboration of private sector [9]. In Siliguri municipality and adjoining area there is a private company, which treat biomedical waste and Government health facilities of Naxalbari block use it.
In Northern part of West Bengal especially in Darjeeling District there is a lack of documented information and studies on injection safety in primary health care system. Nursing staffs and ANMs are the main injection provider in the government primary health care facilities.
Aim
Hence, this study was carried out among Nursing staffs and ANM working in government primary health facilities of Naxalbari Block of Darjeeling district, West Bengal, to explore the situation of injection safety practices and safe disposal; which can be done by the following objectives:
To find out the critical steps of an injection administration which are executed according to recommended best practices, to find out availability of necessary equipments in the facilities to give safe injection and to ascertain safe disposal of the waste produced after injection in the facilities.
Materials and Methods
Darjeeling district, in the hilly region of Northern part of West Bengal had four community development blocks in the plains and 8 community development blocks in hilly areas. Naxalbari is one of them serves as our field practice area. One Primary health centre (PHC), one Block Primary health centre (BPHC) and fifteen Sub centres (SC) were the government primary health care facilities available under Naxalbari Block. All were chosen as study settings and all nursing staffs including General Nurse Midwives (GNM), Public Health Nurses (PHN), Auxillary Nurse Midwives (ANM) posted in BPHC and PHC and sub centres respectively, were considered as study population. A descriptive cross-sectional study was conducted from September to December 2013. Verbal consent was sought from each study subject before interview and observation. Those who were absent after maximum visit, had been excluded from this study.
In Naxalbari block, one BPHC, one PHC, fifteen Sub Centres were present as public health facility. Total 27 nursing staffs were working in BPHC and PHC. In all the sub centres 30 ANMs were posted. Out of total 57 health staffs, 2 nursing staffs had long leave during the study period. So ultimately, 55 study subjects were contacted.
During the observation of the injection providing procedure each health worker observed for at least 30 minutes and in that time period best practiced injection procedure was taken for study.
A pre-designed, pre tested, semi structured data collection schedule and check list adopted and modified from WHO guide line of revised injection safety assessment tool (Tool – C) [1] was used as tools of the study.
Verbal consent was obtained from respective in charge of health facilities. A semi structured schedule and checklist had been developed. It was adopted and modified from WHO guideline of safe injection practice [1]. Briefing was done to the respective authority for purpose of the study. Face validity was judged by three experts. The modified version of the schedule and check list had been pretested among a small group of ANMs of another block by pilot testing. Then it has been applied over the study population. Each sub centre, PHC, BPHC was visited maximum three, four, five times respectively during the study period. Data was collected twice a week. Investigators were visited the study settings and observe the procedure of injection practice before taking the interview. No prior intimation was provided regarding day of visit and no health education was given beforehand regarding injection safety.
Some Operational Definitions
A safe injection is a procedure that does not harm the recipient, does not expose the provider to any avoidable risk and does not result in any waste that is dangerous for other people [1].
Critical Steps
In order not to harm the patient, each procedure should be administered with a new sterile single-use device, using the right medication, vaccine and provider should wash her hands with soap and water.
In order not to expose the provider to any avoidable risk,
Gauge and proper ampoule breaker should use and any needles used during a procedure should be placed in a puncture-proof closed container immediately after use without recapping.
Providers of these procedures should be fully vaccinated against Hepatitis B.
In order that any waste produced during performance of a procedure does not become a hazard for other people, used sharps waste and infectious non-sharps waste should be safely managed and the final disposal of sharps containers and other medical waste should be conducted according to local and international health and environmental standards [1].
Statistical Analysis
All collected data was reviewed and checked. Then a master table was formed using a excel sheet (Microsoft office Excel 2007). Then the data was analysed using principles of descriptive statistics. Data was presented in tables and charts.
Ethical Clearance
Ethical approval was obtained from Institutional Ethics Committee of North Bengal Medical College, Darjeeling, India.
Results
A cross-sectional study was conducted among nursing staffs in PHC, BPHC and ANMs in sub centers along with those health facilities in primary health care delivery system of Naxalbari Block of Darjeeling district. Out of 55 study subjects 56.4% belonged to 30-39 years age group and only 5.5% were in 50-59 years age group; 56.4% were class XII pass, 36.4% graduate and only 1.8% were post graduate. Out of 55 health staffs 30 were ANM and 24 GNM and only one had completed BSC nursing. Among the study subjects 32.7% had <5 years working experience where as 14.5% had ≥20 years. These staff was recruited by recruitment board and formal in-service training was not done during study period.
[Table/Fig-1] depicts that, 93.3% of ANM and all nursing staffs observed took syringe from unopened packet. 13.3% of ANM and 8% nursing staffs are vaccinated against Hepatitis B. Out of total, 53.3% of all nursing staffs observed did not recap after vaccination. Though two ANMs used gauge during breaking of the ampoule but none of the nursing staffs use it. All nursing staffs used proper ampoule breaker but 20% of ANMs used proper ampoule breaker.
Distribution of study subjects according critical steps of safe injection practice.
| Component of critical steps | Critical steps for health care providers | ANMn=30 | NSn=25 |
|---|
| For recipient safety | Syringe taken from unopened packet | 28 (93.3) | 25 (100.0) |
| Hand washing with soap and water before injection | 30 (100.0) | 25 (100.0) |
| For provider’s | Providers Vaccinated against Hepatitis B | 4 (13.3) | 2 (8.0) |
| Not recapped | 16 (53.3) | 25 (100.0) |
| Gauge used during breaking ofampoule | 2 (6.7) | 0 (0.0) |
| Ampoule breaker used | 6 (20.0) | 25 (100.0) |
*values in the parenthesis represent percentage
[Table/Fig-2] shows that, none of the health facilities including Sub centers, PHC, BPHC where multi dose vial used, there was no needle on diaphragm in between the two injections. A total of 13.3% of the sub centers and both in PHC and BPHC have at least one puncture resistant and leak proof container.
Distribution of study health facility according to critical steps of injection practice.
| Component of critical steps | Critical steps for health facilities | Sub-centre(n=15) | PHC(n=1) | BPHC(n=1) |
|---|
| For provider’s | Health facilities having puncture resistant and leak proof container | 2(13.3) | 1(100.0) | 1(100.0) |
| For community safety | Loose needles or syringe absent in side facility | 13(86.7) | 1(100.0) | 1(100.0) |
| Full sharp containers stored safely. | 0(0.0) | 1(100.0) | 1(100.0) |
*values in the parenthesis represent percentage
Though PHC and BPHC had running water supply but only 33.3% of sub centers had the facility, 66.7% of sub centers and both the PHC & BPHC have alcohol based hand rub. None of the health facilities had WHO recommended standard safety box, 47.1% of sub centers along with the BPHC have needle remover or needle destroyer and all the staffs of those facilities used that.
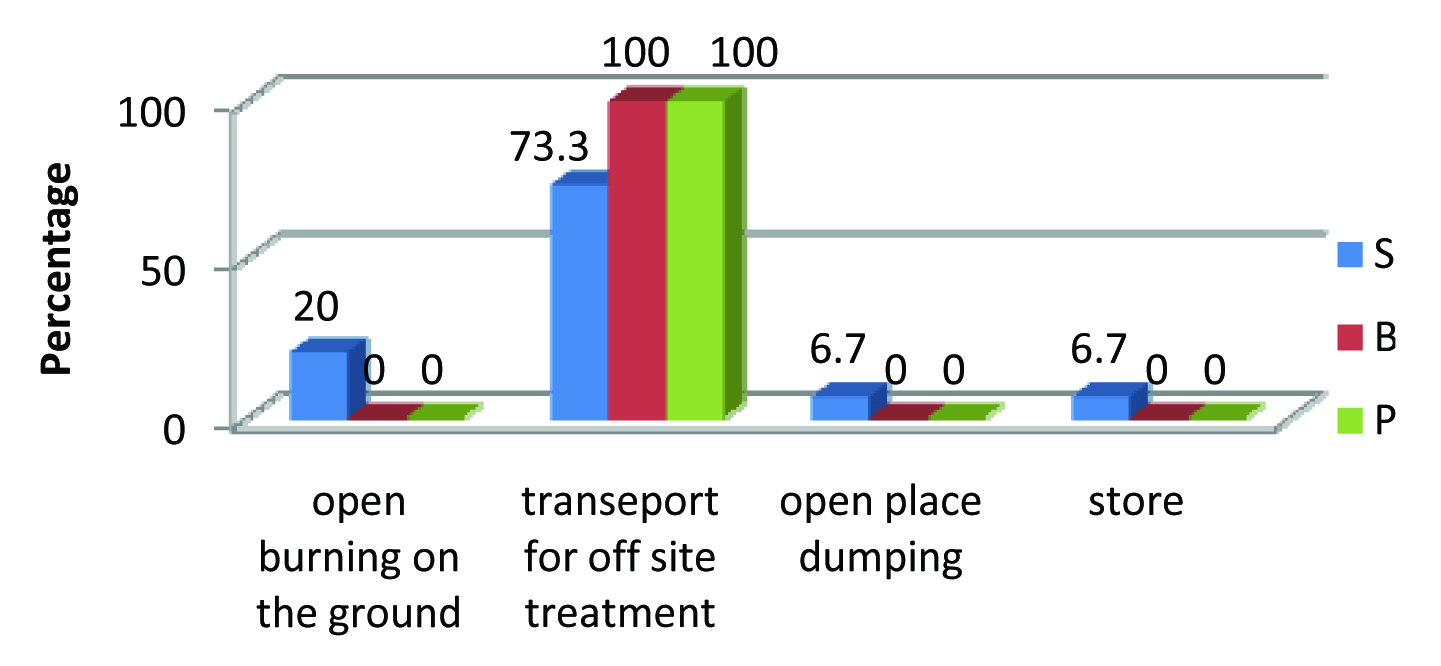
Out of 15 sub centers 11 (73.3%) transported their waste for offsite treatment and both PHC and BPHC transported their waste outside for offsite treatment. Out of total, 20% sub centers disposed waste by open burning, 6.7% disposed by open dumping and only one sub centre stored their waste in a room for last 5 years [Table/Fig-3].
Distribution of health facility according to waste disposal methods.
Over flowing of waste container was not observed in PHC & BPHC along with 3 of the total sub centers. In 5 sub centres and PHC & BPHC, providers immediately disposed sharps in appropriate container. Only 2 sub centers were found to have sharp containers closed before final destruction. In 14 sub centers and only PHC, used sharps were not seen outside the health facility.
Discussion
In this study health workers who are posted in different levels of primary health care in Naxalbari block and involved in injection delivery procedure are of ANMs and Nursing staffs. They had different category of training, age, working experience, etc. More than half of the study subjects were 30-39 age group and had less than 10 years working experience.
The entire ANMs used auto disabled syringe where all of the nursing staff used disposable syringe. All of them washed hands with soap water before giving injection though running water is not available in all facilities. None of the study subjects used gloves in current study because of unavailability at sub centre level and patient over load in PHC & BPHC. Another study done by Paul B et al., in a tertiary care hospital of West Bengal shows that only 12.5% of study subjects washes hand before giving injection and only 3.7% of them used gloves during injection, which differs from current study [7]. Health workers in present study washed hands once at the beginning of the procedure irrespective of giving multiple injections to same recipient or injections to multiple recipients in same occasion.
13.3% of the ANMs and 8% of Nursing Staffs immunised with Hep B vaccination, which was quite lower than studies by Chowdhury AK et al., at PHC level in Bangladesh (23%) and Paul B et al., in Kolkata (52.5%) [7,10].
A total of 53.33% of ANMs and all nursing staffs did not recapped needle after injection, which corroborating with the study done in that tertiary care hospital of West Bengal, where 57.5% of the nursing staffs did not recap but differed with a study done among primary health care worker in Illrion district, Nigeria, where staffs of 13.3% health facilities did not recap [11].
In none of our study facility, needle was found on the diaphragm of multi dose vial. Though both the BPHC and PHC had puncture resistant leak proof container but only 2 sub centres (13.3%) possessed that. This result is corroborating with a study done in Bangladesh where only 16.5% health facilities possessed it [10]. Instead of WHO recommended safety box in India puncture resistant leak proof container is supplied in Government health facilities. This study showed there were no loose needles or syringe inside the 86.7% sub centres and PHC but unfortunately it was in BPHC. Similar study by Bolarinwa et al., in Nigeria shows that there were no loose needles in 66.7% health facilities [11]. So, though overall picture compare to Nigeria was good but there was scope to improve in BPHC in current study. Though in PHC and BPHC full sharp containers stored safely, none of the sub centres stored that safely. Out of 15 sub centres, 10 sub centres practices outside treatment along with PHC and BPHC. Similar study done by Mahfouz et al., in south-western Saudi Arabia showed that all the rural and urban health facilities had provision of professional company service for waste disposal [12]. Another study among PHC level worker in Nepal by Gyawali S et al., showed that in 80% case open burning was the main method for waste disposal [13].
Limitation
Data was collected by single researcher and maximum twice in a week due to shortage of manpower and time study was only restricted in a single block.
Observation of the health workers after obtaining informed consent may affect the results towards best practices due to Hawthorne effect.
Conclusion and Recommendation
There were different sectors and components of a safe injection. In our current study, it showed that in some components like hand washing, using syringe from sterile un-open packed and absence of loose needles inside the facility were quite good whereas in other sectors there were huge scope of improvement.
There was high unsafe injection practice among ANMs as evident from high level of needle recapping and risky final waste disposal methods.
It is suggested that there should be on the job training and regular supportive supervision of ANM and nursing staffs on proper usage of available injection equipments and follow proper procedure.
*values in the parenthesis represent percentage
*values in the parenthesis represent percentage
[1]. World Health Organization (WHO). Revised injection safety assessment tool (Tool C-Revised). Geneva. 2008 [Google Scholar]
[2]. World Health Organization (WHO). Fact sheet no.231. Geneva; 2002: 2-3 [Google Scholar]
[3]. Reid S: Preliminary results of the WHO GBD from unsafe injections [abstract]. Geneva: World Health Organization; 2010. who.int/injection_safety/sign/en/. In Report on Annual Meeting of the Safe Injection Global Network, 9-11November 2010, Dubai, United Arab Emirates (Accessed 18Jan. 2015). [Google Scholar]
[4]. Omorogbe VE, Omuemu VO, Isara AR, Injection safety practices among nursing staff of mission hospitals in Benin City, NigeriaAnnals of African Medicine 2012 11(1):36-41. [Google Scholar]
[5]. Parthasarathy A, Sukumaran TU, Kamath SS, Mishra A, IAP Guide book of safe injection practices 2012 3rd edMumbai:1[cited 2015 April 8]. Available from:http://www.iapindia.org/files/GUIDE_BOOK_ON_SAFE_INJECTION_PRACTICES_28sep.pdf [last accessed 20 May 2015] [Google Scholar]
[6]. Kotwal A, Priya R, Thakur R, Gupta V, Kotwal J, Seth T, Injection practices in a metropolis of North India: perceptions, determinants and issues of safetyIndian J Med Sci 2004 58(8):334-44. [Google Scholar]
[7]. Paul B, Roy S, Chattopadhyay D, Bisoi S, Misra R, Bhattacharya N, A study on safe injection practices on nursing personnel in a tertiary care hospital of Kolkata, West Bengal, IndiaTAF Prev Med Bull 2011 10(6):681-86. [Google Scholar]
[8]. Ministry Of Environment & Forests. Notification. New Delhi, 20th July, 1998 Available from: http://envfor.nic.in/legis/hsm/biomed.html. (last accessed on 11th February, 2015.) [Google Scholar]
[9]. West Bengal Pollution Control Board. Waste inventory (MSW & BMW) in West Bengal. Available from: http://www.wbpcb.gov.in/html/downloads/sw_inventory.pdf. (last accessed on 12th February 2015.) [Google Scholar]
[10]. Chowdhury AK, Roy T, Faroque A, Bachar SC, Aasduzzaman M, Nasrin N, A comprehensive situation assessment of injection practices in primary heath care hospitals in BangladeshBMC public health 2011 11(1):779-826. [Google Scholar]
[11]. Bolarinwal OA, Salaudeen AG, Aderibigbe SA, Musa IO, Akande TM, Bamidele JO, Injection safety practices among primary health care workers in Ilrion, kwara state of NijeriaHealth Science Journal 2012 6(3):496-508. [Google Scholar]
[12]. Mahfouz AA, Abdelmoneim I, Khan MY, Daffalla AA, Diab MM, Shaban H, Injection safety at primary health care level in south-western Saudi ArabiaEastern Mediterranean Health Journal 2009 15(2):443-50. [Google Scholar]
[13]. Gyawali S, Rathore D, Bhuvan KC, Shankar PR, Study of status of safe injection practice and knowledge regarding injection safety among primary health care workers in Baglung district, western NepalBMC international health and human rights 2013 13(3):5-6. [Google Scholar]