Total Extraction as a Treatment for Anaemia in a Patient of Glanzmann’s Thrombasthenia with Chronic Gingival Bleed: Case Report
Abhishek Ghosh1, Saurabh Kumar2, Rabin Chacko3, Arun Paul Charlu4
1 Fellow, Head and Neck Oncology, HCG Cancer Centre, (Previously Fellow at CMC Vellore), Ahmedabad, India.
2 Assistant Professor, Department of Oral and Maxillofaical Surgery, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
3 Head of Department Unit I, Department of Oral and Maxillofacial Surgery, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
4 Associate Professor, Department of Oral and Maxillofacial Surgery, Christian Medical College and Hospital, Vellore, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abhishek Ghosh, HCG Cancer Centre Sola-Science City Road, Off S.G. Highway, Sola, Ahmedabad, Gujarat-380060, India. E-mail : 13abhishekghosh@gmail.com
Glanzmann’s Thrombasthenia (GT) is a rare autosomal recessive bleeding disorder affecting the megakaryocyte lineage and is characterized by lack of platelet aggregation on stimulation. The molecular basis is linked to quantitative and qualitative abnormalities of αIIbβ3 integrin. Most of the patients with severe Glanzmann’s thrombasthenia have spontaneous gum bleeding and persistent low haemoglobin levels. Often these patients are addressed with local haemostatic measures and platelet coverage. We report a case of a severe Glanzmann’s thrombasthenia with chronic gingivitis and associated spontaneous gum bleed with chronic low haemoglobin levels, managed subsequently with total dental extraction under appropriate platelet and recombinant factor VIIa coverage. Further follow up of the patient substantiated the treatment protocol with increased and stable haemoglobin levels, thus emphasizing the need for total dental extraction in patients with severe Glanzmann’s with chronic spontaneous gum bleed, as a definitive treatment option, which has not been reported so far in the literature.
αIIbβ3 deficiency, Platelet disorder, Recombinant factor VIIa, Spontaneous gingival hemorrhage, Total extraction
Case Report
An 18-year-old male patient presented to the Department of Oral and Maxillofacial Surgery, with complain of chronic bleeding from gums since early childhood. He was born to parents who had consanguineous marriage. He was referred to our department from the Department of Haematology and had been under their care since the age of 2 years as he was a known case of severe Glanzmann’sThrombasthenia (diagnosed with flow-cytometry and family history). He had undergone extraction of all his primary teeth under general anaesthesia at the age of 8 years with improvement in his symptoms and haemoglobin levels for about a year. He had only one sibling; an elder brother also suffering from severe Glanzmann’s Thrombasthenia, who succumbed to the disease at the age of 16 years. The sibling had a similar problem of continuous gingiva bleeding with resultant very low haemoglobin levels. No dental intervention apart from repeated scalings (oral prophylaxis) under platelet cover had been done for him.
On examination the patient had generalized gingivitis and chronic spontaneous bleeding from the gingiva [Table/Fig-1,2]. Periodontal evaluation by a Periodontist led to diagnosis of Chronic Generalized Marginal Gingivitis with localized Periodontitis with respect to tooth number 45. His OPG revealed no bone loss and clinically too, there wasn’t any sign of pathological tooth mobility [Table/Fig-3]. His haemoglobin levels had never been above 5gm% for the past 6 months and on an average had been around 3.6 gm% due to recurrent and persistent gingival bleed. He had undergone frequent transfusion of platelets and packed cells and recombinant factor VIIa. After extensive examinations and investigations including full body CT scans and MRI, the sole site for haemorrhage was isolated to the oral cavity gingiva. Thus, a treatment plan of total extraction was reached at and the patient’s consent sought. The patient had undergone oral prophylaxis one year back. He had inherent fear of aggravating the bleeding from gingiva while brushing and thus maintenance of oral hygiene was an issue; leading to chronic gingivitis. After receiving the consent for the proposed treatment plan, under platelets, packed cells and recombinant factor VIIa coverage, total extraction was done under general anaesthesia on 19th march 2014. Post extraction sockets were sutured with 3-0 vicryl after packing the sockets with Tranexamic Acid powder (mixed with betadine solution to make a putty-like consistency dough which could be easily moulded and packed into the extraction sockets and retained with the sutures), thus avoiding the need of post extraction splints as mentioned in the literature [1,2]. The patient had to be repeatedly transfused with platelets and packed cells for the next 2 postoperative weeks till the extraction wounds healed satisfactorily to achieve prolonged haemostasis.
Intra-Oral Pre-Op Photograph Right Side.

Intra-oral pre-op photograph left side.


Blood Product Cover
4 units packed cells (red blood cells).
34 units platelet rich concentrates.
Inj. Novoseven (recombinant coagulation factor VIIa) 2mg, 18 doses over 1 week period.
One month postoperatively patient’s haemoglobin was 11.4gm% and then 6 months post operatively it was stable at 10.1gm%. After the initial haemostasis was achieved post operatively, the patient has not been yet transfused with factor/platelets/packed cells. Last blood and platelet transfusion had been done on 13th April 2015. The patient has been on follow-up, most recently reviewed in the month of August 2015. The patient has not been rehabilitated with complete denture, as the gingival was erythematous and atrophic [Table/Fig-4,5] at few sites and there was risk of subsequent ulceration and bleeding with denture usage. Further the patient was apprehensive of trauma from denture and refused the same. Thus a wait and watch policy was adopted till a healthier gingiva replaces the existing one. The patient continues to be on diet which is soft and semi-liquid in consistency.
April 2015 1 year post op photographs of edentulous maxilla.

April 2015 1 year Post Op photographs of edentulous mandible.

Discussion
Glanzmann’s Thrombasthenia is an extremely rare qualitative platelet disorder, characterized by platelets containing defective or low levels of integrin αIIbβ3 (formerly known as Glycoprotein IIb-IIIa), which is a receptor for fibrinogen. It is an integrin coded by the ITGA2b and ITGB3 genes. As a result, no fibrinogen bridging of platelets to other platelets can occur and the bleeding time is significantly prolonged. Dr. Eduard Glanzmann a German paediatrician in the year 1918 first described this bleeding disorder in children from a village named Le Valais in the Swiss Alps, as “Hereditary Hemorrhagic Thrombasthenia” [3]. In this village there were frequent marriages between close relatives. Glanzmann’s Thrombasthenia is inherited in an autosomal recessive manner or acquired as an autoimmune disorder.
Epidemiology
There is an increased frequency of consanguinity in affected families and an increased incidence in populations in whom marriage among close relatives is an accepted custom. In certain ethnic groups for example South-Indian Hindus, Iraqi Jews, French gypsies, and Jordanian nomadic tribes, thrombasthenia is a common hereditary haemorrhagic disorder [4].
Classification
Type I: (Severe): < 5% of Glycoprotein (IIb-IIIa) levels.
(Absent platelet aggregation and absent clot retraction)
Type II: (Less Severe): 10-20% of Glycoprotein (IIb-IIIa) levels, but functionally inactive.
(Absent aggregation but residual clot retraction)
Type III: (Variant): Normal levels, but functionally inactive. (first described in 1987) [4]
Our patient had Severe Glanzmann’s Thrombasthenia (diagnosed with flow-cytometry) and had frequent episodes of gum bleeding and consequent decreased haemoglobin concentration at the time of presentation. Patient had been repeatedly admitted or treated at the Emergency Department for the same. Maintenance of oral hygiene was a problem for the patient. The patient was afraid to brush properly; apprehensive of initiating another episode of bleeding from the gums. Consequently the patient suffered from chronic generalised gingivitis and subsequently it led to bleeding from the gums. The chronic inflammation of the gingiva and the fragility of capillary walls during the inflammatory process along with the inherent qualitative defects of the platelets in GT patient preventing clot formation and retraction led to spontaneous chronic gingival bleed. Thus, a continuing vicious cycle propagated.
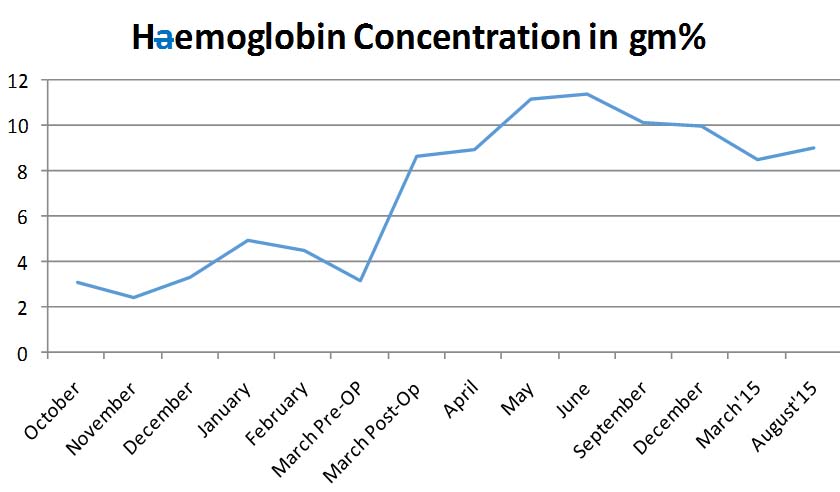
At our department we went through literature for support of our treatment plan and found no existing articles suggesting total exodontia for similarly affected GT patients. In literature there are reports of splints placed over the extraction socket to keep in place the gel foam pack [1,2]. However, in our case splint fabrication was not possible as our aim was total exodontia and any plate fabricated preoperatively would not have had the stability nor the retention post operatively and thus would have only compounded the patient’s problem. Further follow-up of the patient substantiated the treatment protocol with increased and stable haemoglobin levels [Table/Fig-6], thus emphasising total dental extraction, as a definitive treatment option. Patients having the disease can have fair prognosis with good supportive treatment. Exact prognosis of the disease is not known owing to the extreme rarity of the disease. Approximately 200 cases have been reported in the literature so far [5].
Hemoglobin Concentration in gm%.
It is very important to screen these patients for blood borne viruses owing to them having undergone repeated blood transfusions [6]. In order to avoid platelet allo-immunisation, therapeutic management must include local haemostatic procedures and or Desmopressin (DDAVP) administration, transfusion of HLA-compatible platelets. Administration of recombinant factor VIIa is also used alternatively.
Conclusion
Through the cited case report we have reported a treatment protocol of total exodontia in patients of severe Glanzmann’s Thrombasthenia suffering from chronic spontaneous gingival bleed leading to chronic low levels of haemoglobin. Such radical treatment has not so far been reported in literature. The post-operative raised and maintained levels of haemoglobin on follow-up substantiate our treatment protocol.
[1]. Yadalam U, Kranti K, Seshan H, Periodontal considerations for Glanzmann’sthrombasthenia patientJ Indian Soc Periodontol 2008 12:26-27. [Google Scholar]
[2]. Mehta DN, Bhatia R, Dental Considerations in the management of Glanzmann’s thrombastheniaInternational Journal of Clinical Pediatric Dentistry 2010 3:51-56. [Google Scholar]
[3]. Nurden AT, Glanzmann thrombastheniaOrphanet J Rare Dis 2006 1:10 [Google Scholar]
[4]. George JN, Caen JP, Nurden AT, Glanzmann’s thrombasthenia: The spectrum of the clinical diseaseBlood 1990 75:1383-95. [Google Scholar]
[5]. Bisch FC, Bowen KJ, Hanson BS, Kudryk VL, Billman MA, Dental considerations for a Glanzmann’sthrombasthenia patient: case reportJ Periodontol 1996 67(5):536-40. [Google Scholar]
[6]. Manne RK, Natarajan K, Patil R, Prathi VS, Glanzmann thrombasthenia associated with Human Immunodeficiency Virus positive patientInt J Prev Med 2014 5:500-04. [Google Scholar]