Hysterectomy is the second most common operation performed by the Gynaecologists [1,2], next only to Caesarean Section and can be done through abdominal, vaginal and laparoscopic routes [3]. Despite multiple studies stating that vaginal route is preferred to abdominal route in mobile uteri of 12 weeks or lesser, ACOG committee opinion is the only formal guideline establishing the fact [4]. Traditional abdominal and vaginal hysterectomies represent the most and least invasive techniques respectively. The ease and convenience offered by a large abdominal incision have led to the preponderance of abdominal hysterectomy over the vaginal route. Laparoscopic route is associated with increased operating times and rise in the rate of intraoperative injuries [5]. The common belief that bigger, bulky uteri, endometriosis, Pelvic inflammatory disease, previous surgeries [6], and narrow vagina make vaginal hysterectomy difficult to be performed are not considered to be contra-indications for non-descent vaginal hysterectomy and can be successfully attempted in all these conditions. It has a clear advantage over the abdominal route in obese women [7,8]. However, proper selection of patients is a critical factor in determining the success of vaginal procedures. Lack of expertise and the curve in learning the technique also has major impact on the number of procedures performed [9,10]. In our centre, hysterectomy is performed by laparoscopic, abdominal and vaginal routes. However, due to the vast majority of cases being performed by the latter two methods, the comparison in this study is between vaginal and abdominal hysterectomies. The aim of this study was to evaluate the most efficient route of hysterectomy in women with mobile nonprolapsed uteri of 12 weeks or lesser by comparing the intra and postoperative complications of vaginal and abdominal hysterectomies.
Materials and Methods
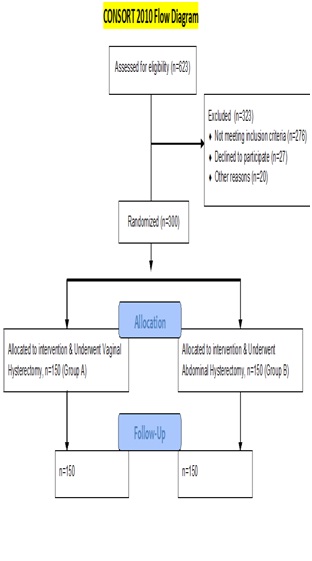
In a randomized prospective comparative study conducted at the Department of Obstetrics and Gynaecology, Gauhati Medical College and Hospital, Guwahati, 623 patients requiring hysterectomy were selected from the Outpatient Department and detailed history elicited and general and systemic examinations performed and confounding variables strictly controlled by following inclusion and exclusion criteria, as explained in [Table/Fig-1]. Of which, 256 did not meet the inclusion criteria, 47 patients declined to participate 20 patients did not come back to the hospital. Thus, 323 patients were excluded from the study and 300 consecutive patients requiring hysterectomy for benign uterine conditions were analysed over a period of 2 years (December 2012–November 2014) and were alternately allocated to vaginal and abdominal groups. Group A (n = 150) underwent vaginal hysterectomy (non-descent vaginal hysterectomy, NDVH) which was compared with group B (n = 150) who had abdominal hysterectomy. Women were included in the study only if the uterine size was 12 weeks or lesser, uterus was mobile and if the operation was being performed for a benign uterine condition. Women were excluded if their uterus was more than 12 weeks size, restricted mobility, uterovaginal prolapse, complex adnexal mass, previous 2 or more LSCS. Women who had ophorectomy concurrently with hysterectomies were included. Informed, written consent was taken from all the patients after explaining the risks and benefits associated with the procedure. Approval of ethical committee was also taken.
Operative Techniques
In the total abdominal hysterectomy group, Pfannensteil incision was made, abdomen opened in layers, uterus was elevated out of the pelvis by applying Kocher’s clamps to the side of uterine cornu bilaterally. Bilateral clamps were applied to the round and tubo-ovarian ligaments (to the infundibulo-pelvic ligaments if ovariotomy was planned), cut and ligated. Uterovesical fold was opened and bladder mobilized to the lower limit of cervix. Then subsequential clamps were applied to the uterine artery and mackenrodt’s - uterosacral ligaments bilaterally, clamped, cut and transfixed. Uterus delivered out and vault closure done. After securing haemostasis, abdomen was closed in layers [11]. In the vaginal group, labial sutures were applied, bladder evacuated. Holding the cervix with vulsellum, transverse incision was made on anterior vaginal wall. Deepening the incision, the pubo-vesico-cervical ligament was reached and incised. Pushing the bladder up with steady traction, Uterovesical peritoneum was visualized and was incised and incision extended. After opening the Pouch of Douglas, bilateral Mackenrodt’s-Uterosacral ligaments were clamped, cut and transfixed, the same procedure was followed for uterine artery and fundal structures followed by vault closure [12].
All patients were given prophylactic Inj. cefotaxime on operation table just before skin incision. The operating time was noted from time of incision till the end of the procedure. To measure intraoperative blood loss, weight of swab in the dry and blood soaked states was measured and 19mg weight difference was equted to 1ml blood loss. Temperature was assessed and charted 4 hourly, defining Febrile Morbidity as 38°C on 2 occasions 4 hours apart, excluding the first postoperative day. Patients were routinely given injectable analgesics on day 1 twice. After this, patients were given oral/injectable analgesics on request only and the total number of days of analgesic requirement was noted. Intraoperative blood loss and injuries, postoperative pain, blood transfusion, mobility, febrile morbidity, infections, hospital stay, conversion to abdominal route, re-laparotomy were recorded and the data was statistically analysed using Chi-square test and t-test and p-value was determined.
Results
A total of 300 patients were included in the study. One hundred and fifty patients underwent vaginal hysterectomy and 150 patients underwent abdominal hysterectomy. Baseline demographic characteristics were comparable in both abdominal and vaginal hysterectomy groups [Table/Fig-2]. 6.67% (n=10) of the patients in the vaginal group had previous pelvic surgeries while 3.33% (n=5) of the patients in the abdominal group had history of one pelvic surgery (e.g. tubal ligation, ovarian cystectomy or laparotomy). 40% of patients in each of the groups had co-morbidities like hypertension, diabetes mellitus, bronchial asthma, ischemic heart disease and anemia, as shown in [Table/Fig-2]. The Gynaecological diseases were diagnosed by pathological examination, and the results are also shown in [Table/Fig-3]. The diseases in each group were comparable. In the vaginal group, 25.33% (n=38) had undergone concurrent salpingo-ophorectomy (unilateral in 21% & bilateral in 4.33%), whereas 30.67% in the abdominal group (n=46), had undergone concurrent salpingo-ophorectomy (unilateral in 24% & bilateral in 6.67%), as shown in [Table/Fig-4].
Baseline demographic characteristics.
| BASELINE CHARACTERISTICS | VAGINAL HYSTERECTOMY | ABDOMINAL HYSTERECTOMY |
|---|
| Age, (in years) | 43.83 | 42.23 |
| Parity | 2.53 | 2.47 |
| No.of patients with previous pelvic surgeries | 6.67% (n=10) | 3.33% (n=5) |
| Medical illness | 40% (n=60) | 40% (n=60) |
| DIAGNOSIS | VAGINAL HYSTERECTOMY | ABDOMINAL HYSTERECTOMY |
|---|
| Fibroid | 56.67% (n=85) | 54.67% (n=82) |
| Endometrial hyperplasia/polyp | 21.33% (n=32) | 24% (n=36) |
| Chronic cervicitis | 6% (n=9) | 4.67% (n=7) |
| Adenomyosis | 7.33% (n=11) | 9.33% (n=14) |
| Dysfunctional Uterine Bleeding | 6% (n=9) | 5.33% (n=8) |
| Cervical Intraepithelial Neoplasia | 2.67% (n=4) | 2% (n=3) |
| Salphingo-oophorectomy | VAGINAL HYSTERECTOMY | ABDOMINAL HYSTERECTOMY |
|---|
| Done | 25.33% (n=38) | 30.67% (n=46) |
| Not done | 74.67% (n=112) | 69.33% (n=104) |
None of the cases in the vaginal group were converted to abdominal route. There were no intraoperative complications such as bladder, rectum or urethra injuries or re-laparotomies in any groups. The mean duration of surgery was 37.07 minutes in the vaginal group, whereas, it was 56.4 minutes in the abdominal group, implying a significant difference (p< 0.05). Similarly, a significantly higher blood loss (249 ml) was noted in the abdominal hysterectomy group, compared to 102.5 ml in the vaginal group (p< 0.05). Postoperatively, the abdominal group required more analgesia in comparison to the vaginal group as measured by number of days requirement of analgesics postopeartively as shown in [Table/Fig-5]. The mean length of hospital stay was 10.87 days in the abdominal group while the duration was 4.67 days in the vaginal group. Mean time to postoperative mobility and mean maximum postoperative body temperature in the vaginal hysterectomy group were significantly shorter and less severe respectively than those in the abdominal group (p< 0.05). Significantly lesser number of patients required postoperative blood transfusion in the vaginal group (n=15) compared to the abdominal group (n=55). Significantly high postoperative wound infection rate was noted in 33.33% (n=50) of patients in the abdominal group, compared to the vaginal group (n=0). However, there was no significant difference in the rates of systemic infection like respiratory tract infection, urinary tract infection, paralytic ileus and acute gastroenteritis postoperatively in both the groups.
Intraoperative and Postoperative Outcomes.
| Factor | Vaginal hysterectomy | Abdominal hysterectomy | Test of significance | p-value | Statistical significance |
|---|
| Operation duration (mins) | 37.07 | 56.4 | t’ test | <0.00001 | Significant |
| Blood loss (ml) | 102.5 | 249 | <0.00001 | Significant |
| Postoperative pain (days of analgesic requirement) | 1.62 | 3.72 | <0.00001 | Significant |
| Hospital stay (days) | 4.67 | 10.87 | <0.00001 | Significant |
| Postoperative mobility (days) | 3 | 4.17 | <0.00001 | Significant |
| Postoperative blood transfusion (no. of units) | 10% (n=15) | 36.67% (n=55) | χ2 (chi-square test) | <0.00001 | Significant |
| Postoperative wound infection | 0% (n=0) | (33.33% (n=50) | <0.00001 | Significant |
| Febrile morbidity | 3.33% (n=5) | 23.33% (n=35) | <0.00001 | Significant |
| Postoperative systemic infections | 6.67% (n=10) | 6.67% (n=10) | 1 | Not Significant |
Discussion
The vaginal approach to hysterectomy has been the hallmark of the gynaecological surgeon. The impetus to extend the advantages and explore the limits of the vaginal route came from hands-on experience with patients who were desperate to avoid an abdominal incision. Vaginal surgery allows the surgeon to operate by the least invasive route of all, utilizing an anatomical orifice. Favourable factors for a Non-Descent vaginal hysterectomy are a mobile uterus with normal dimensions, large pelvis to allow manoeuvrability, single, large accessible fibroid, counselling for a tentative vaginal hysterectomy and experience. In case of uteri enlarged due to fibroids, techniques like bisection [13], myomectomy [14], wedge resection [15], slicing method [16], coring [17–19] and use of Ligasure Vessel sealing system [20], may be used either individually or in combination for successful removal of the uterus vaginally. In the absence of obvious contraindications, but with doubt concerning the route of hysterectomy, gynaecologists should consider scheduling patients for a tentative vaginal hysterectomy, a situation analogous to obstetricians performing a trial of forceps. In this study, statistically significant decrease in blood loss during surgery, duration of surgery, postoperative pain, time to postoperative mobility, wound infection, febrile morbidity, length of hospital stay and post operative blood transfusion was noted in the vaginal group when compared with the abdominal group.
Kumar et al., in a study conducted on 80 women planned for NDVH had a success rate of 95% [14]. These patients were treated by vaginal hysterectomy and the operating time, laparotomy conversion rate and intraoperative blood loss was directly proportional to the size of the uterus and concluded that vaginal hysterectomy is a safe and effective procedure in uteri of less than 12 weeks size. Garg et al., conducted a study comparing vaginal hysterectomy with abdominal hysterectomy with 23 patients in each group and found a reduced operating time, lesser intraoperative blood loss, reduced postoperative morbidity and shorter hospital stay in the vaginal hysterectomy group [21]. Mc Cracken et al., in their study concluded that intraoperative and postoperative morbidity were lesser in vaginal hysterectomy compared to abdominal hysterectomy and that vaginal hysterectomy should be the procedure of choice wherever possible [22]. Doucette and co-workers in their study on 250 patients challenged the common contra-indications to vaginal hysterectomy including large uteri, nulliparas, previous CS or laparotomies and concluded that the above mentioned factors are rarely contra-indications [23].
Nieboer et al., in a systematic Cochrane review of nine RCTs in which studies by Ottosen, Benassi, Hwang, Miskry, Ribeiro, Garry, Silva Filho were included and Nasira and co-workers and Gayak et al., summarized that Vaginal hysterectomy is better in terms of intraoperative and postoperative outcomes, when compared to abdominal, laparoscopic and laparoscopic assisted vaginal hysterectomies [24–33].
In this study, no intraoperative complications occurred in patients of the vaginal group, and no vaginal approach was converted to an abdominal approach. Results were comparable to other studies. All these studies indicate that VH is a safe and effective surgical treatment for benign gynaecological diseases and should be offered whenever possible, taking into account the low rate of complications and cost-effectiveness.
Limitations
Limitations in the present study include: 1) This is a single (tertiary) hospital based study and cannot be correlated with general population; 2) Most of the vaginal hysterectomies were carried out by consultant gynaecologists, while abdominal procedures were done equally by consultants and residents; 3) Psycho-sexual implications of both surgeries were not compared; 4) Long term postoperative effects were not taken into account.
Conclusion
In summary, it can be concluded that vaginal hysterectomy is feasible, safe and provides more patient comfort without increasing the duration of surgery, blood loss and other intraoperative complications.