Persistent Primitive Hypoglossal Artery (PPHA) – A Rare Anomaly with Literature Review
MR Srinivas1, KS Vedaraju2, BH Manjappa3, BR Nagaraj4
1 Assistant Professor, Department of Radiodiagnosis and Imaging, Victoria Hospital Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
2 Associate Professor, Department of Radiodiagnosis and Imaging, Victoria Hospital Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
3 Post Graduate Student, Department of Radiodiagnosis and Imaging, Victoria Hospital Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
4 Professor and Head, Department of Radiodiagnosis and Imaging, Victoria Hospital Bangalore Medical College and Research Institute, Bengaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. MR Srinivas, Assistant Professor, Department of Radiodiagnosis and Imaging, Victoria Hospital Bangalore Medical College and Research Institute, Fort, Bangalore- 560002, India.
E-mail: sinumr25@gmail.com
Persistent primitive hypoglossal artery (PPHA) is a rare embryonic carotid vertebrobasilar artery anastomosis. Hypoglossal artery arises from the internal carotid artery (ICA) between the C1 and C2 vertebral levels and traverses through the hypoglossal canal to join the vertebro-basilar system. We present a rare case of an anomalous right sided PPHA as a sole supply to posterior circulation of brain with absent/hypoplastic bilateral vertebral arteries in a two year child who had presented with acute left sided haemiplegia. Three dimensional time of flight magnetic resonance angiography identified an anomalous vessel arising from the right internal carotid artery at the level of axis vertebra and joining the vertebra-basilar arterial system after coursing through the right hypoglossal canal. This anomaly when present may predispose the person to aneurysm formation, ischaemia in the posterior circulation and atherosclerotic disease of the intracranial vessels.
MR Angiography, Proatlantal intersegmental artery, Vertebro-basilar artery
Case Report
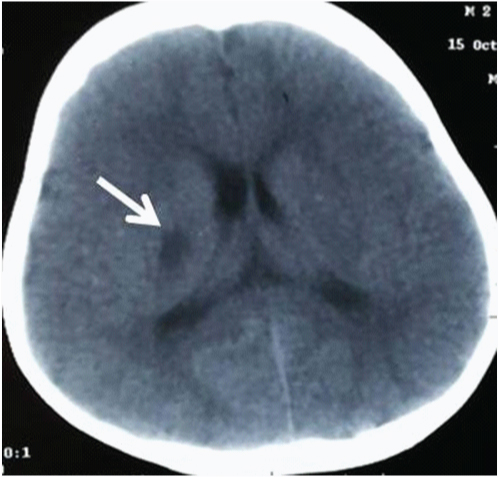
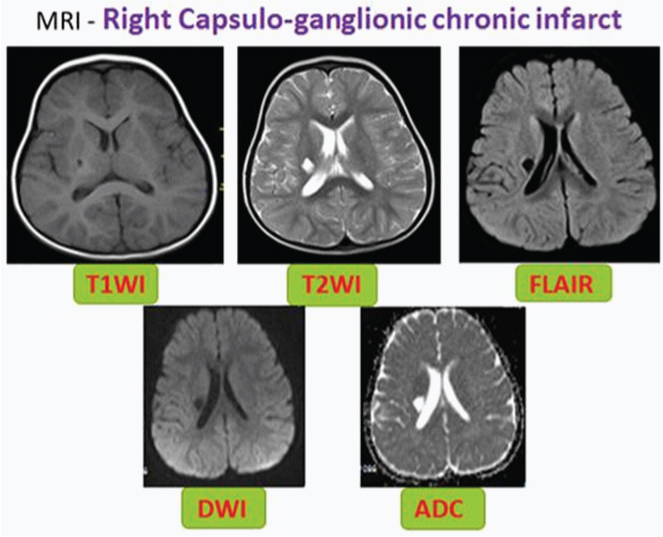
A two-year-old male child presented with acute onset of weakness of left upper and lower limb. There was no facial deviation. He underwent unenhanced computed tomography (CT) scan of the brain in a different hospital and was diagnosed with acute in-farct in the right capsulo-ganglionic region [Table/Fig-1]. Further routine blood investigations and biochaemical investigations did not reveal any abnormality. There was slow improvement in power of the limbs. He was referred to our institute for further evaluation with magnetic resonance (MR) imaging 2 months after the initial onset of symptoms. MRI of the brain along with three- dimensional time of flight (3D- TOF) MR angiography of cervical and intracranial vessels was performed. MR imaging of the brain revealed a chronic infarct in the right capsulo-ganglionic region [Table/Fig-2].
NECT SCAN – Fairly defined hypodense area in Right Capsulo-ganglionic region (White arrow)
Right capsulo-ganglionic chronic infarct – T1 hypointense and T2 hyperintense area inverting on FLAIR and showing no diffusion restriction on DWI sequence
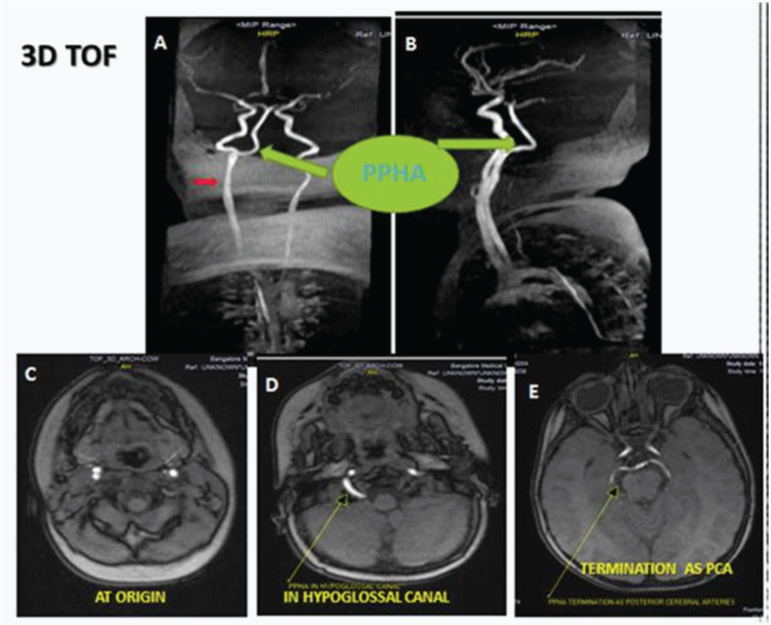
On 3D TOF angiography, an anomalous vessel was seen [Table/Fig-3] arising from the right internal carotid artery (ICA) at the level of axis vertebra. This vessel was seen anastomosing with the basilar artery after coursing through the right hypoglossal canal. Bilateral vertebral arteries were not demonstrated on 3D TOF MR angiography, probably because they were hypoplastic. Intracranial vasculature was otherwise found to be normal.
3D TOF - MIP images in coronal :(A) and sagittal; (B) planes demonstrating an anomalous vessel(PPHA) arising from the cervical part of right internal carotid artery (ICA, red arrow in A) and forming basilar trunk with termination of posterior cerebral arteries (PCA). Bilateral vertebral arteries are absent. Source images in axial planes showing origin(C), course through the hypoglossal canal (arrow in D) and bifurcation into the PCA (arrow in E)
Discussion
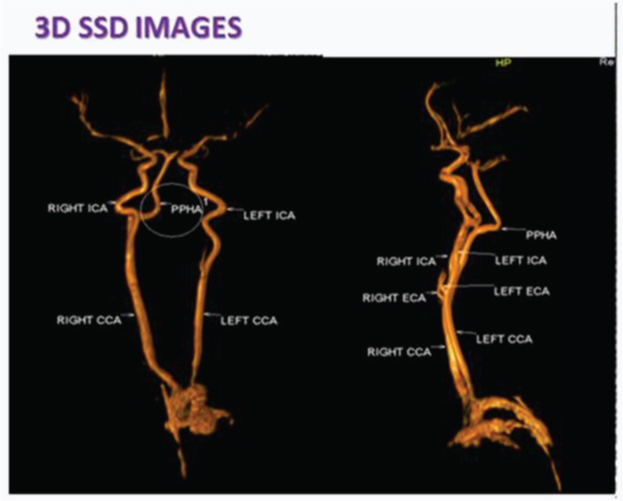
Persistent hypoglossal artery is the second most common persistent carotid-basilar anastomosis (the most frequent being trigeminal artery) [1] with a reported incidence of 0.03–0.09% which signifies that the occurrence of persistent hypoglossal artery is extremely rare [2,3]. The persistent primitive hypoglossal artery is only one among the persistent fetal anastomoses between the carotid and vertebrobasilar circulations [Table/Fig-4]. The other primitive anastomoses include the primitive trigeminal, otic (acoustic), hypoglossal, and proatlantal intersegment arteries. These are named for their relationship with the hypoglossal nerve, trigeminal ganglion, otic vesicle and dorsal aorta respectively [4] [Table/Fig-5].
3D Surface shaded display (SSD) showing PPHA with absent bilateral vertebral arteries
Persistent carotid vertebro-basilar anastomoses from superior to inferior, trigeminal artery (black arrow), Otic artery (white arrow), Hypoglossal artery (curved white arrow) and Proatlantal artery (white arrow head) (“Used with permission from Amirsys, Inc")
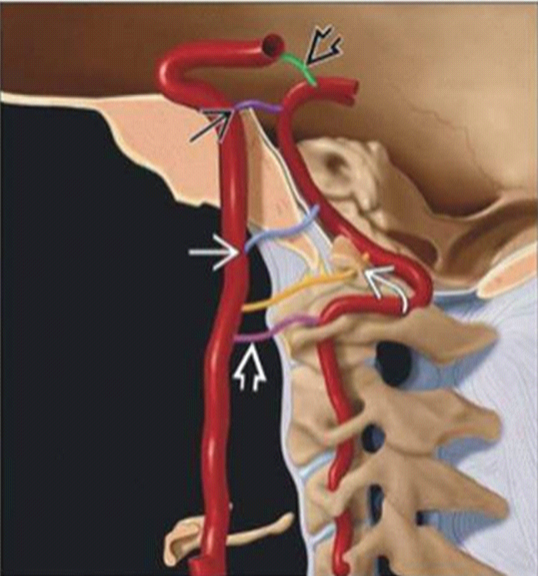
When the embryo is ~4mm, the forebrain is supplied by the carotid system. Two parallel longitudinal neural arteries form along the surface of the hindbrain. They eventually fuse to form the basilar artery. These paired longitudinal neural arteries are initially supplied by the carotid arteries through four important arterial anastomoses. These four anastomoses are named according to their course and include trigeminal artery, otic artery, hypoglossal artery, and proatlantal intersegmental artery [Table/Fig-5] [1].
As the embryo increases in size, an anastomosis forms between the distal internal carotid artery and ipsilateral longitudinal neural artery which subsequently becomes the posterior communicating artery. Following this event, the anastomotic arteries between internal carotid artery and vertebra- basilar system begin to regress. The first anastomotic vessel to regress is otic artery, followed by hypoglossal artery, trigeminal artery and proatlantal intersegmental arteries in that order [1,5].
The last anastomotic artery to regress, the proatlantal intersegmental artery is seen till the embryo is 7 to 12mm in size. This vessel supplies the hindbrain till the vertebral arteries develop and take over the function. The vertebral arteries develop following fusion of the multiple longitudinal anastomoses between the cervical intersegmental arteries [1,5].
Persistent primitive arteries occur when there is failure of regression of the presegmental arteries that supply the posterior circulation in the early fetal brain [1,2,5].
The persistent hypoglossal artery is the second most frequent carotid vertebra-basilar arterial anastomoses, after the persistent trigeminal artery, and usually arises from the internal carotid artery and rarely from the external carotid artery [2].
Criteria for identification of PPHA are [
6]
1. It is arising from the cervical part of the internal carotid artery at C1-C2 vertebral level.
2. PPHA along with the accessory nerve enters the posterior cranial fossa through the hypoglossal canal.
3. Basilar trunk appears filled only beyond its anastomosis with the PPHA.
4. Vertebral arteries and posterior communicating arteries may be hypoplastic or absent.
Clinical Implications of PPHA
Persistent primitive hypoglossal artery is more common in females and on the left side. It may be associated with intracranial arterial aneurysms, ischaemic cerebrovascular attacks, atherosclerosis, sub-arachnoid haemorrhage and arterio-venous malformations. Identification of this rare anomaly is important before carotid endarterectomy or skull base surgery as injury to this vessel can lead to ischaemia in the posterior circulation territory where it forms the sole arterial supply [7].
In a case report by Bapuraj JR et al., a saccular basilar artery aneurysm associated with persistent primitive hypoglossal artery was successfully treated with coil embolisation by endovascular route through the primitive hypoglossal artery [8].
Conclusion
Identification of PPHA is important before carotid endarterectomy or skull base surgery in order to avoid injury as it is the sole supply to posterior circulation. 3D TOF MR Angiography is a useful noninvasive technique for demonstrating the course of this anomalous vessel.
Abbreviations
3D TOF: Three dimensional time of flight; PPHA: Persistent pri-mitive hypoglossal artery; MRI: Magnetic resonance imaging; NECT: Non- enhanced computed tomography;
Author’s Contributions
All authors have contributed significantly and are in agreement with the content of the manuscript. MR is the guarantor of this work and takes responsibility for the integrity of the data and the accuracy. BH and KS researched data and assisted in literature review. MR and BR drafted the manuscript. All authors read and approved the final manuscript.
[1]. Luh GY, Dean BL, Tomsick TA, Wallace RC, The persistent fetal carotid-vertebrobasilar anastomosesAJR 1999 172:1427-32. [Google Scholar]
[2]. Osborne AG, Osborne’s Brain 2013 1721st edCanadaAmirsys publishing Inc:74 [Google Scholar]
[3]. Fujita N, Shimada N, Takimoto H, Satou T, MR appearance of the persistent hy-poglossal arteryAJNR 1995 16:990-92. [Google Scholar]
[4]. Tubbs RS, Verma K, Riech S, Mortazavi MM, Shoja MM, Loukas M, Per-sistent fetal intracranial arteries: A comprehensive review of anatomical and clini-cal significanceJ Neurosurg 2011 114:1127-34. [Google Scholar]
[5]. Takahashi H, Tanaka H, Fujita N, Tomiyama N, Bilateral persistent hypoglossal arteries: MRI findingsBr J Radiol 2012 85:e46-48. [Google Scholar]
[6]. Lie TA, Congenital anomalies of the carotid arteries 1968 AmsterdamExcerpta Medi-ca:35-51. [Google Scholar]
[7]. Yamamoto S, Sunada I, Matsuoka Y, Hakuba A, Nishimura S, Persistent primi-tive hypoglossal artery aneurysms: Report of two casesNeurol Med Chir (Tokyo) 1991 31:199-202. [Google Scholar]
[8]. Bapuraj JR, Ojili V, Khandelwal N, Shanboque AK, Gupta SK, Basilar artery aneurysm treated with coil embolization via persistent primitive hypoglossal ar-teryAustralas Radiol 2007 51:B340-43. [Google Scholar]